Ann Rehabil Med.
2018 Jun;42(3):425-432. 10.5535/arm.2018.42.3.425.
Relationship Between Swallowing Function and Maximum Phonation Time in Patients With Parkinsonism
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. srcho918@yuhs.ac
- 2Brain Korea 21 Plus Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 3Avison Biomedical Research Center, Yonsei University College of Medicine, Seoul, Korea.
- 4Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2417834
- DOI: http://doi.org/10.5535/arm.2018.42.3.425
Abstract
OBJECTIVE
To identify the relationship between maximum phonation time (MPT) and swallowing function, as well as the elements of swallowing, in order to provide a rationale for speech therapy in patients with Parkinsonism manifesting dysphagia.
METHODS
Thirty patients with Parkinsonism who underwent speech evaluation and videofluoroscopic swallowing study (VFSS) were recruited. The MPT, the longest periods of sustained pronunciation of /aa/, was evaluated. The VFSS was evaluated using Penetration Aspiration Scale (PAS), National Institutes of Health-Swallowing Safety Scale (NIH-SSS), and Videofluoroscopic Dysphagia Scale (VDS). The relationship between dysphagia scales and MPT was analyzed using Pearson correlation. The difference in VDS variables between subgroups (Parkinson disease or Parkinsonian syndrome, independent or dependent ambulation, and normal or abnormal MPT) and the difference in MPT between subgroups based on the VDS variables were analyzed using the independent t-test.
RESULTS
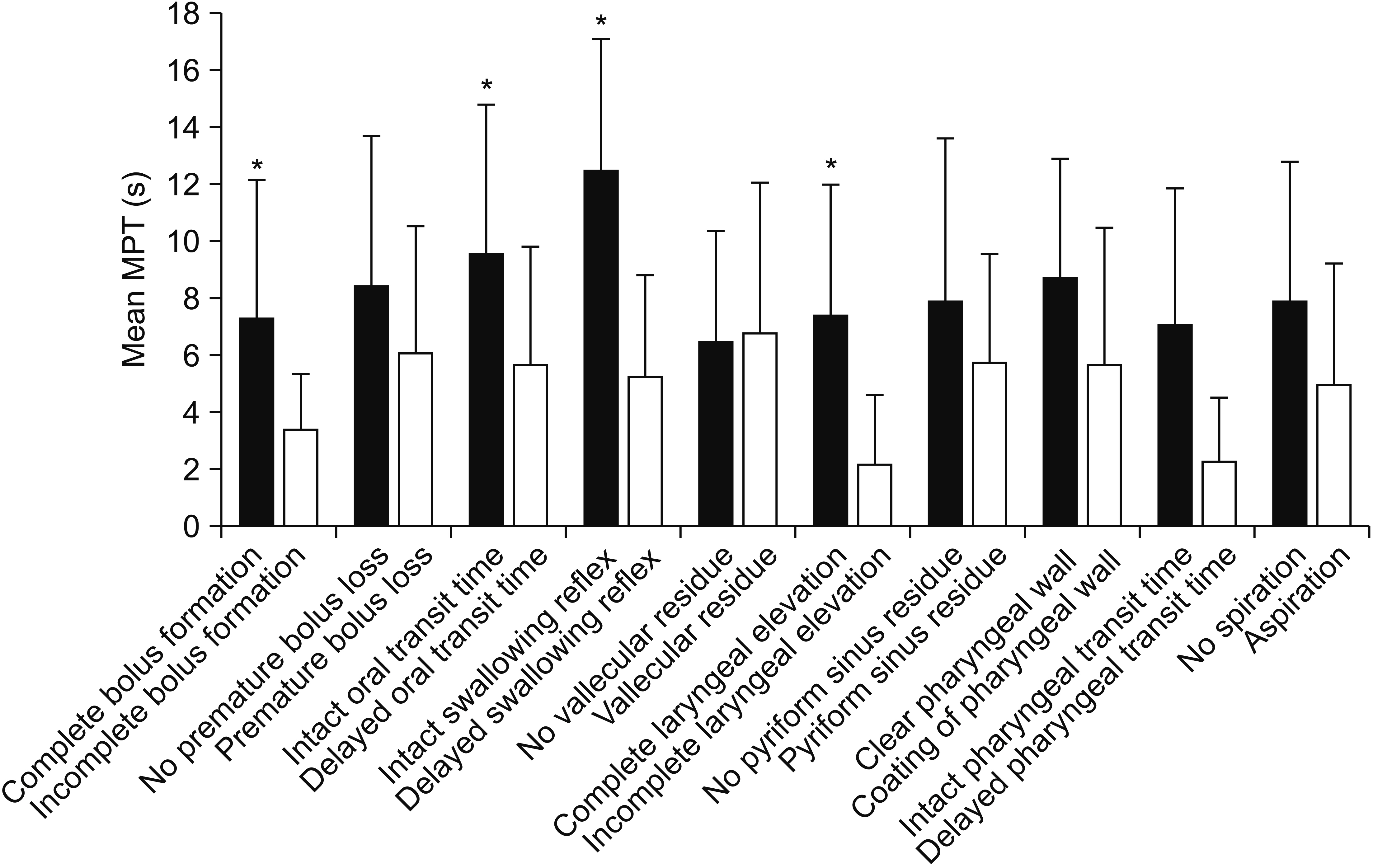
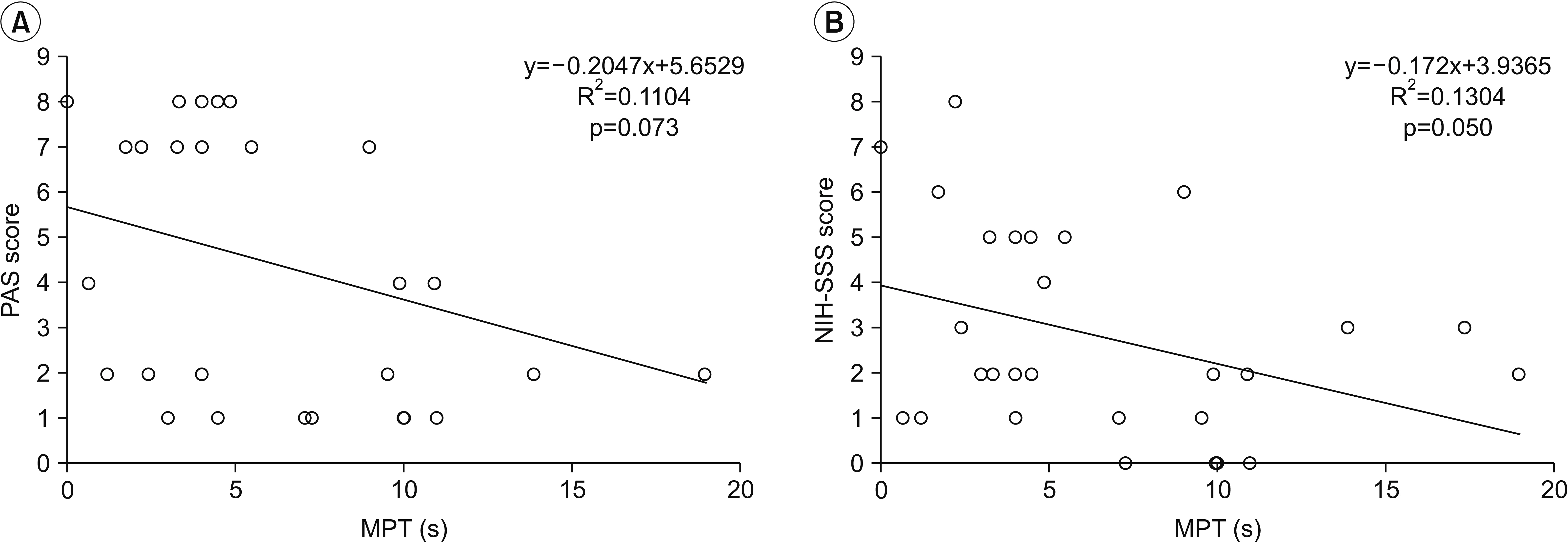
Bolus formation and laryngeal elevation functions were significantly higher in the normal MPT group compared with the impaired group. In the VDS variables, patients with intact bolus formation, oral transit time, pharyngeal swallow triggering, and laryngeal elevation showed significantly longer MPTs compared with the impaired groups. In addition, MPT was significantly correlated with the VDS and modestly correlated with the NIH-SSS, but not the PAS, suggesting that phonatory function is related to the oropharyngeal swallowing function, but not directly to the aspiration itself.
CONCLUSION
The correlation between MPT and several swallowing-related elements was identified, indicating an interactive correlation between swallowing and phonation. This result justifies voice therapy as a treatment for dysphagia in patients with Parkinsonism.
MeSH Terms
Figure
Cited by 1 articles
-
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Plowman-Prine EK, Sapienza CM, Okun MS, Pollock SL, Jacobson C, Wu SS, et al. The relationship between quality of life and swallowing in Parkinson’s disease. Mov Disord. 2009; 24:1352–8.
Article2. Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015; 386:896–912.
Article3. Potulska A, Friedman A, Krolicki L, Spychala A. Swallowing disorders in Parkinson’s disease. Parkinsonism Relat Disord. 2003; 9:349–53.
Article4. van Hooren MR, Baijens LW, Voskuilen S, Oosterloo M, Kremer B. Treatment effects for dysphagia in Parkinson’s disease: a systematic review. Parkinsonism Relat Disord. 2014; 20:800–7.
Article5. Suttrup I, Warnecke T. Dysphagia in Parkinson’s disease. Dysphagia. 2016; 31:24–32.
Article6. Regan J, Walshe M, Tobin WO. Immediate effects of thermal-tactile stimulation on timing of swallow in idiopathic Parkinson’s disease. Dysphagia. 2010; 25:207–15.
Article7. van Hooren MR, Baijens LW, Vos R, Pilz W, Kuijpers LM, Kremer B, et al. Voice- and swallow-related quality of life in idiopathic Parkinson’s disease. Laryngoscope. 2016; 126:408–14.
Article8. Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010; 25:40–65.
Article9. Stegemoller EL, Radig H, Hibbing P, Wingate J, Sapienza C. Effects of singing on voice, respiratory control and quality of life in persons with Parkinson’s disease. Disabil Rehabil. 2017; 39:594–600.10. Maslan J, Leng X, Rees C, Blalock D, Butler SG. Maximum phonation time in healthy older adults. J Voice. 2011; 25:709–13.
Article11. Speyer R. Effects of voice therapy: a systematic review. J Voice. 2008; 22:565–80.
Article12. Valim MA, Santos RS, Macedo Filho ED, da Silva Abdulmassih EM, Serrato MR. The relationship between the maximum time for phonation, fundamental frequency and protection of the lower airways in patients with neurological dysphagia. Int Arch Otorhinolaryngol. 2007; 11:260–6.13. Kim H. Neurologic speech-language disorders. Seoul: Sigmapress;2012.14. Belafsky PC, Kuhn MA. The clinician’s guide to swallowing fluoroscopy. New York: Springer;2014. p. 59–68.15. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article16. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64.
Article17. El Sharkawi A, Ramig L, Logemann JA, Pauloski BR, Rademaker AW, Smith CH, et al. Swallowing and voice effects of Lee Silverman Voice Treatment (LSVT): a pilot study. J Neurol Neurosurg Psychiatry. 2002; 72:31–6.18. Troche MS, Okun MS, Rosenbek JC, Musson N, Fernandez HH, Rodriguez R, et al. Aspiration and swallowing in Parkinson disease and rehabilitation with EMST: a randomized trial. Neurology. 2010; 75:1912–9.
Article19. Pitts T, Bolser D, Rosenbek J, Troche M, Okun MS, Sapienza C. Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease. Chest. 2009; 135:1301–8.
Article20. Stegemoller EL, Hibbing P, Radig H, Wingate J. Therapeutic singing as an early intervention for swallowing in persons with Parkinson’s disease. Complement Ther Med. 2017; 31:127–33.21. Russell JA, Ciucci MR, Connor NP, Schallert T. Targeted exercise therapy for voice and swallow in persons with Parkinson’s disease. Brain Res. 2010; 1341:3–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study on Phonatory Function of Pre and Post-Operative Condition of Vocal Nodules
- Specially Programmed Respiratory Muscle Training for Singers by Using Respiratory Muscle Training Device (Ultrabreathe (R) )
- Correlations between orbicularis oris and mentalis muscle activity and craniofacial morphology in normal occlusion and Class III malocclusion
- Phonological Characteristics in Parkinson's Disease
- Phonation time and pulmonary function in spinal cord injured patients