Ann Pediatr Endocrinol Metab.
2018 Jun;23(2):57-61. 10.6065/apem.2018.23.2.57.
Delayed puberty versus hypogonadism: a challenge for the pediatrician
- Affiliations
-
- 1Department of Internal Medicine and Therapeutics, Unit of Pediatrics and Adolescentology, University of Pavia, Pavia, Italy. mauro.bozzola@unipv.it
- 2Onlus “Il Bambino e il suo pediatraâ€, Galliate, Italy.
- 3Department of Pediatrics, Pediatric and Infectious Diseases Unit, Bambino Gesù Children Hospital IRCCS, Rome, Italy.
- 4Unit of Pediatrics and Neonatology, Ferrari Hospital, Cosenza, Italy.
- 5Institute of Pediatrics, Catholic University, Rome, Italy.
- KMID: 2417760
- DOI: http://doi.org/10.6065/apem.2018.23.2.57
Abstract
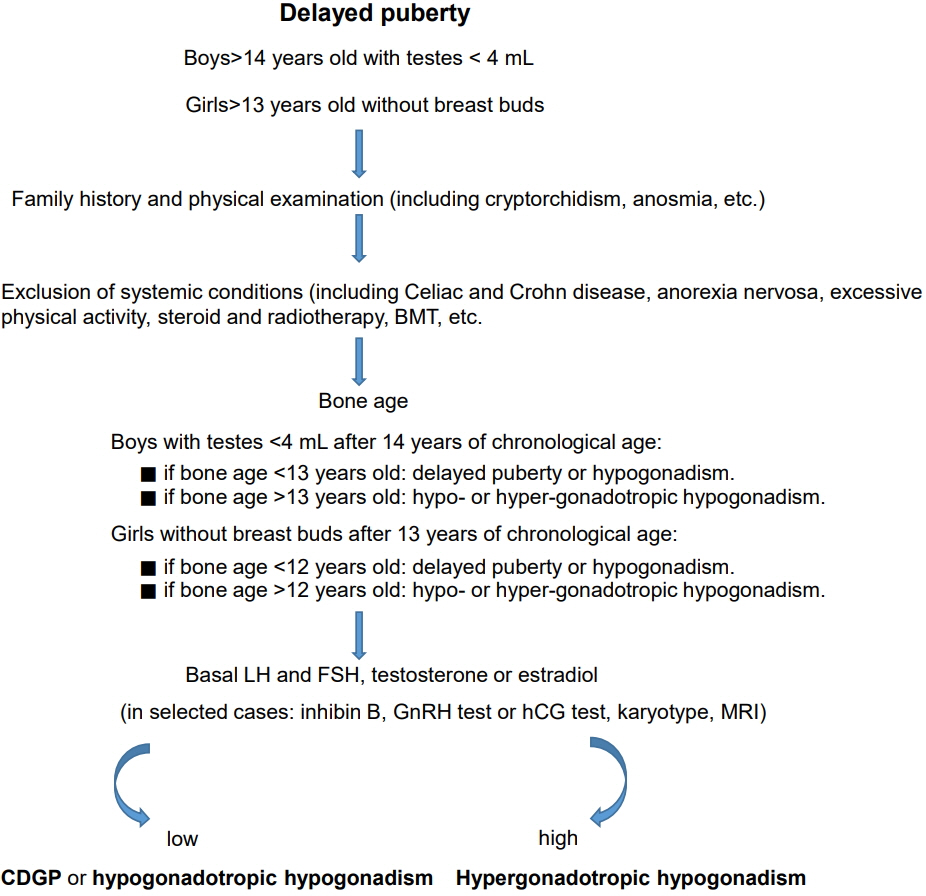
- Constitutional delay of growth and puberty (CDGP) is the most common cause of delayed puberty (DP), is mainly found in males, and is characterized by short stature and delayed skeletal maturation. A family history of the subject comprising the timing of puberty in the parents and physical examination may provide clues regarding the cause of DP. Delayed onset of puberty is rarely considered a disease in either sex. In fact, DP usually represents a common normal variant in pubertal timing, with favorable outcomes for final height and future reproductive capacity. In adolescents with CDGP, a linear growth delay occurs until immediately before the start of puberty, then the growth rate rapidly increases. Bone age is often delayed. CDGP is a diagnosis of exclusion; therefore, alternative causes of DP should be considered. Functional hypogonadotropic hypogonadism may be observed in patients with transient delay in hypothalamic-pituitary-gonadal axis maturation due to associated conditions including celiac disease, inflammatory bowel diseases, kidney insufficiency, and anorexia nervosa. Permanent hypogonadotropic hypogonadism (pHH) showing low serum value of testosterone or estradiol and blunted follicle-stimulating hormones (FSH) and luteinizing hormones (LH) levels may be due to abnormalities in the central nervous system. Therefore, magnetic resonance imaging is necessary to exclude morphological abnormalities and neoplasia. Moreover, pHH may be isolated, as observed in Kallmann syndrome, or associated with other hormone deficiencies, as found in panhypopituitarism. Baseline or gonadotropin-releasing hormone pituitary stimulated gonadotropin level is not sufficient to easily differentiate CDGP from pHH. Low serum testosterone in male patients and low estradiol values in female patients, associated with high serum FSH and LH levels, suggest a diagnosis of hypergonadotropic hypogonadism. A genetic analysis can reveal a chromosomal abnormality (e.g., Turner syndrome or Klinefelter syndrome). In cases where the adolescent with CDGP is experiencing psychological difficulties, treatment should be recommended.
MeSH Terms
-
Adolescent
Anorexia Nervosa
Celiac Disease
Central Nervous System
Chromosome Aberrations
Diagnosis
Estradiol
Female
Gonadotropin-Releasing Hormone
Gonadotropins
Humans
Hypogonadism*
Inflammatory Bowel Diseases
Kallmann Syndrome
Lutein
Magnetic Resonance Imaging
Male
Parents
Physical Examination
Puberty
Puberty, Delayed*
Renal Insufficiency
Testosterone
Turner Syndrome
Estradiol
Gonadotropin-Releasing Hormone
Gonadotropins
Lutein
Testosterone
Figure
Reference
-
References
1. Wu FC, Butler GE, Kelnar CJ, Huhtaniemi I, Veldhuis JD. Ontogeny of pulsatile gonadotropin releasing hormone secretion from midchildhood, through puberty, to adulthood in the human male: a study using deconvolution analysis and an ultrasensitive immunofluorometric assay. J Clin Endocrinol Metab. 1996; 81:1798–805.
Article2. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970; 45:13–23.
Article3. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969; 44:291–303.
Article4. Wehkalampi K, Widén E, Laine T, Palotie A, Dunkel L. Patterns of inheritance of constitutional delay of growth and puberty in families of adolescent girls and boys referred to specialist pediatric care. J Clin Endocrinol Metab. 2008; 93:723–8.
Article5. LaFranchi S, Hanna CE, Mandel SH. Constitutional delay of growth: expected versus final adult height. Pediatrics. 1991; 87:82–7.
Article6. Rohani F, Alai MR, Moradi S, Amirkashani D. Evaluation of near final height in boys with constitutional delay in growth and puberty. Endocr Connect. 2018; 7:456–9.
Article7. Hayes FJ, Seminara SB, Crowley WF Jr. Hypogonadotropic hypogonadism. Endocrinol Metab Clin North Am. 1998; 27:739–63.
Article8. Bhagavath B, Podolsky RH, Ozata M, Bolu E, Bick DP, Kulharya A, et al. Clinical and molecular characterization of a large sample of patients with hypogonadotropic hypogonadism. Fertil Steril. 2006; 85:706–13.
Article9. Bianco SD, Kaiser UB. The genetic and molecular basis of idiopathic hypogonadotropic hypogonadism. Nat Rev Endocrinol. 2009; 5:569–76.
Article10. Gajdos ZK, Henderson KD, Hirschhorn JN, Palmert MR. Genetic determinants of pubertal timing in the general population. Mol Cell Endocrinol. 2010; 324:21–9.
Article11. Copeland KC, Chernausek S. Mini-puberty and growth. pediatrics. 2016; 138:e20161301.
Article12. Lanes R, Gunczler P, Osuna JA, Palacios A, Carrillo E, Ramirez X, et al. Effectiveness and limitations of the use of the gonadotropin-releasing hormone agonist leuprolide acetate in the diagnosis of delayed puberty in males. Horm Res. 1997; 48:1–4.
Article13. Odink RJ, Schoemaker J, Schoute E, Herdes E, Delemarrevan de Waal HA. Predictive value of serum folliclestimulating hormone levels in the differentiation between hypogonadotropic hypogonadism and constitutional delay of puberty. Horm Res. 1998; 49:279–87.
Article14. Smals AG, Hermus AR, Boers GH, Pieters GF, Benraad TJ, Kloppenborg PW. Predictive value of luteinizing hormone releasing hormone (LHRH) bolus testing before and after 36-hour pulsatile LHRH administration in the differential diagnosis of constitutional delay of puberty and male hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 1994; 78:602–8.
Article15. Kletter GB, Rolfes-Curl A, Goodpasture JC, Solish SB, Scott L, Henzl MR, et al. Gonadotropin-releasing hormone agonist analog (nafarelin): a useful diagnostic agent for the distinction of constitutional growth delay from hypogonadotropic hypogonadism. J Pediatr Endocrinol Metab. 1996; 9:9–19.
Article16. Zamboni G, Antoniazzi F, Tatò L. Use of the gonadotropinreleasing hormone agonist triptorelin in the diagnosis of delayed puberty in boys. J Pediatr. 1995; 126(5 Pt 1):756–8.
Article17. Wilson DA, Hofman PL, Miles HL, Unwin KE, McGrail CE, Cutfield WS. Evaluation of the buserelin stimulation test in diagnosing gonadotropin deficiency in males with delayed puberty. J Pediatr. 2006; 148:89–94.
Article18. Puett D, Li Y, DeMars G, Angelova K, Fanelli F. A functional transmembrane complex: the luteinizing hormone receptor with bound ligand and G protein. Mol Cell Endocrinol. 2007; 260-262:126–36.
Article19. Dunkel L, Perheentupa J, Virtanen M, Mäenpää J. GnRH and HCG tests are both necessary in differential diagnosis of male delayed puberty. Am J Dis Child. 1985; 139:494–8.
Article20. Coutant R, Biette-Demeneix E, Bouvattier C, Bouhours-Nouet N, Gatelais F, Dufresne S, et al. Baseline inhibin B and anti-Mullerian hormone measurements for diagnosis of hypogonadotropic hypogonadism (HH) in boys with delayed puberty. J Clin Endocrinol Metab. 2010; 95:5225–32.
Article21. Dwyer AA, Raivio T, Pitteloud N. Management of endocrine disease: reversible hypogonadotropic hypogonadism. Eur J Endocrinol. 2016; 174:R267–74.
Article