Clin Nutr Res.
2018 Jul;7(3):189-198. 10.7762/cnr.2018.7.3.189.
Anthropometric Indices from Primary to High School in the West of Iran: Epidemiologic Trends
- Affiliations
-
- 1Administration of Food and Drug, Kermanshah University of Medical Sciences, Kermanshah 6715847141, Iran.
- 2Department of Nutrition, Faculty of Nutrition Sciences and Food Technology, Kermanshah University of Medical Sciences, Kermanshah 6715847141, Iran. Yahya.pasdar@kums.ac.ir
- 3Nutrition Research Center, Faculty of Nutrition, Tabriz University of Medical Sciences, Tabriz 5166614711, Iran.
- 4Students' Research Committee, Tabriz University of Medical Sciences, Tabriz 5166614711, Iran.
- 5Social Development and Health Promotion Research Center, Kermanshah University of Medical Sciences, Kermanshah 6715847141, Iran.
- 6Health and Treatment Network of Eslamabade Gharb, Kermanshah University of Medical Sciences, Kermanshah 6715847141, Iran.
- KMID: 2417715
- DOI: http://doi.org/10.7762/cnr.2018.7.3.189
Abstract
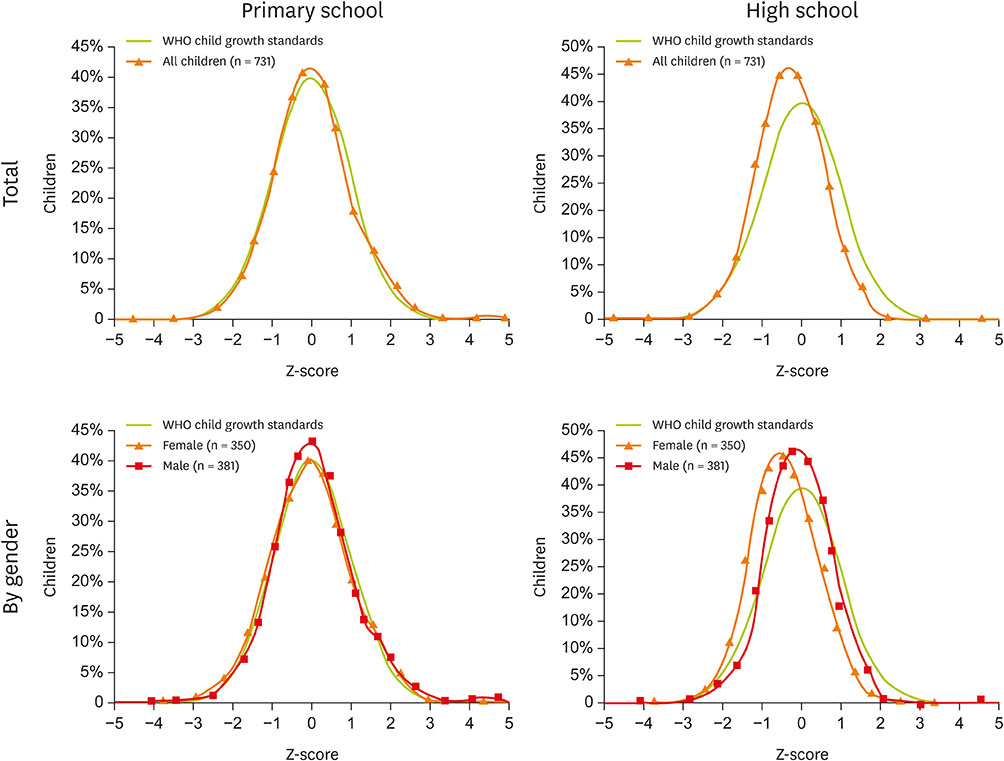
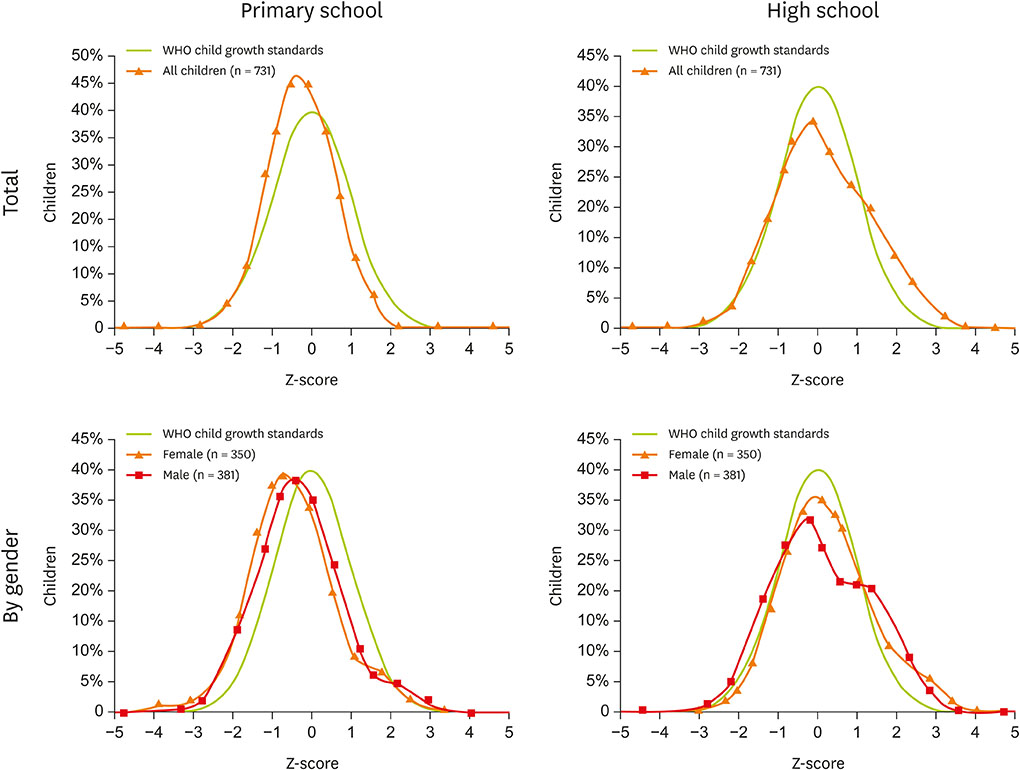
- Examining the trend of anthropometric indices in children and adolescents in each region can be highly beneficial in providing effective strategies to improve the status of their growth. This study was conducted with the aim of determining the trend of anthropometric indices in students from primary to high school in the west of Iran. Data were collected using a demographic questionnaire and health certificates for anthropometric information of primary school students, and current anthropometric measurements with scale for high school students. Then, all of the data were analyzed in AnthroPlus and SPSS software. Of the 731 students, 350 were female and 381 were male. Mean height Z-score to age showed a significant reduction from primary to high school (from +0.0386 to −0.27416), and mean body mass index Z-score to age showed a significant increase (from −0.3916 to +0.1826). Prevalence of stunting and overweight/obesity in high school was 1.4 and 2.5 times higher than primary school, respectively, but the prevalence of wasting reduced by 2.3 fold. Girls were more affected by the increased trend of obesity and stunting compared to boys. Nutritional transition was evident in students. Healthcare policy-makers should design and implement a comprehensive health strategy to deal with this situation, especially in girls.
Keyword
MeSH Terms
Figure
Reference
-
1. Ministry of Health, Treatment and Medical Education (IR). Health map of Islamic Republic of Iran in 5th economic, social and cultural development program 2010–2014. Tehran: Ministry of Health, Treatment and Medical Education;2009.2. Mahan LK, Escott-Stump S, Raymond JL, Krause MV. Krause's food & the nutrition care process. Philadelphia, PA: Elsevier Health Sciences;2012.3. National Exceptional Education Organization, Health and Prevention Office. Nourishment and physical exercises assistance. Identity student health card: 3-6. 2005.4. World Health Organization. Growth charts: 5 to 19 years 2007. 2007. cited 2007 July 18. Available from http://www.who.int/growthref/tools/en.5. Florentino RF. The double burden of malnutrition in Asia: a phenomenon not to be dismissed. J ASEAN Fed Endocr Soc. 2014; 26:133.
Article6. Ghassemi H, Harrison G, Mohammad K. An accelerated nutrition transition in Iran. Public Health Nutr. 2002; 5:149–155.
Article7. Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: a critical review. Food Nutr Bull. 2014; 35:230–243.
Article8. Zhu H, Zhang X, Li MZ, Xie J, Yang XL. Prevalence of Type 2 diabetes and pre-diabetes among overweight or obese children in Tianjin, China. Diabet Med. 2013; 30:1457–1465.
Article9. Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes. 2012; 36:1–11.
Article10. Munger KL, Bentzen J, Laursen B, Stenager E, Koch-Henriksen N, Sørensen TI, Baker JL. Childhood body mass index and multiple sclerosis risk: a long-term cohort study. Mult Scler. 2013; 19:1323–1329.
Article11. Calder PC, Jackson AA. Undernutrition, infection and immune function. Nutr Res Rev. 2000; 13:3–29.
Article12. Jones KD, Thitiri J, Ngari M, Berkley JA. Childhood malnutrition: toward an understanding of infections, inflammation, and antimicrobials. Food Nutr Bull. 2014; 35:S64–70.
Article13. Asao K, Kao WH, Baptiste-Roberts K, Bandeen-Roche K, Erlinger TP, Brancati FL. Short stature and the risk of adiposity, insulin resistance, and type 2 diabetes in middle age: the Third National Health and Nutrition Examination Survey (NHANES III), 1988-1994. Diabetes Care. 2006; 29:1632–1637.
Article14. El Taguri A, Besmar F, Abdel Monem A, Betilmal I, Ricour C, Rolland-Cachera MF. Stunting is a major risk factor for overweight: results from national surveys in 5 Arab countries. East Mediterr Health J. 2009; 15:549–562.
Article15. Paajanen TA, Oksala NK, Kuukasjärvi P, Karhunen PJ. Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis. Eur Heart J. 2010; 31:1802–1809.
Article16. Kermanshah University of Medical Sciences (KUMS). Research priorities of KUMS, row 7, no 140: 8. 2012. cited 2014 October 20. Available fromhttp://vc-research.kums.ac.ir/fa/link1.17. Conde WL, Monteiro CA. Nutrition transition and double burden of undernutrition and excess of weight in Brazil. Am J Clin Nutr. 2014; 100:1617S–1622S.
Article18. Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014; 168:561–566.
Article19. Savva SC, Kourides YA, Hadjigeorgiou C, Tornaritis MJ. Overweight and obesity prevalence and trends in children and adolescents in Cyprus 2000–2010. Obes Res Clin Pract. 2014; 8:e426–34.
Article20. Stamatakis E, Zaninotto P, Falaschetti E, Mindell J, Head J. Time trends in childhood and adolescent obesity in England from 1995 to 2007 and projections of prevalence to 2015. J Epidemiol Community Health. 2010; 64:167–174.
Article21. Kelishadi R, Haghdoost AA, Sadeghirad B, Khajehkazemi R. Trend in the prevalence of obesity and overweight among Iranian children and adolescents: a systematic review and meta-analysis. Nutrition. 2014; 30:393–400.
Article22. World Health Organization. WHO AnthroPlus software. Geneva: World Health Organization;2007.23. Sahargahi B, Pormehr R, Rezaei M, Naderi MR, Mohammadi S, Moradi A. The comparison of height for age index with normal distribution in Eslamabade-Gharb students (2007–8). J Kermanshah Univ Med Sci. 2012; 16:375–379.24. Urke HB, Mittelmark MB, Valdivia M. Trends in stunting and overweight in Peruvian pre-schoolers from 1991 to 2011: findings from the Demographic and Health Surveys. Public Health Nutr. 2014; 17:2407–2418.
Article25. de Onis M, Blössner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990-2020. Public Health Nutr. 2012; 15:142–148.
Article26. Salehi-Abargouei A, Abdollahzad H, Bameri Z, Esmaillzadeh A. Underweight, overweight and obesity among zaboli adolescents: a comparison between international and iranians' national criteria. Int J Prev Med. 2013; 4:523–530.27. Mirmohammadi SJ, Hafezi R, Mehrparvar AH, Rezaeian B, Akbari H. Prevalence of overweight and obesity among Iranian school children in different ethnicities. Iran J Pediatr. 2011; 21:514–520.28. Sheikholeslam R, Naghavi M, Abdollahi Z, Zarati M, Vaseghi S, Sadeghi Ghotbabadi F, Kolahdooz F, Samadpour K, Minaei M, Arabshahi S. Current status and the 10 years trend in the malnutrition indexes of children under 5 years in Iran. Iran J Epidemiol. 2008; 4:21–28.29. Kroker-Lobos MF, Pedroza-Tobías A, Pedraza LS, Rivera JA. The double burden of undernutrition and excess body weight in Mexico. Am J Clin Nutr. 2014; 100:1652S–1658S.
Article30. Shafique S, Akhter N, Stallkamp G, de Pee S, Panagides D, Bloem MW. Trends of under- and overweight among rural and urban poor women indicate the double burden of malnutrition in Bangladesh. Int J Epidemiol. 2007; 36:449–457.
Article31. Sharma J, Mondal N. Prevalence of double nutrition burden among adolescent girls of assam, northeast India. J Nepal Paediatr Soc. 2014; 34:132–137.
Article32. Severi C, Moratorio X. Double burden of undernutrition and obesity in Uruguay. Am J Clin Nutr. 2014; 100:1659S–1662S.
Article33. Rahmanian M, Kelishadi R, Qorbani M, Motlagh ME, Shafiee G, Aminaee T, Ardalan G, Taslimi M, Poursafa P, Asayesh H, Larijani B, Heshmat R. Dual burden of body weight among Iranian children and adolescents in 2003 and 2010: the CASPIAN-III study. Arch Med Sci. 2014; 10:96–103.
Article34. Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010; 91:1499S–1505S.
Article35. Sheiner E, Levy A, Katz M, Mazor M. Short stature--an independent risk factor for Cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2005; 120:175–178.
Article36. Motlagh ME, Kelishadi R, Amirkhani MA, Ziaoddini H, Dashti M, Aminaee T, Ardalan G, Mirmoghtadaee P, Keshavarz S, Poursafa P. Double burden of nutritional disorders in young Iranian children: findings of a nationwide screening survey. Public Health Nutr. 2011; 14:605–610.
Article37. Senbanjo IO, Oshikoya KA, Odusanya OO, Njokanma OF. Prevalence of and risk factors for stunting among school children and adolescents in Abeokuta, southwest Nigeria. J Health Popul Nutr. 2011; 29:364–370.
Article38. Rezazadeh K, Dorosty Motlagh A, Omidvar N, Rashidkhani B. Prevalence of stunting-cum-overweight and its association with socio-demographic characteristics of parents in school-age children in Khoy City, Iran. Iran J Nutr Sci Food Technol. 2009; 4:35–46.39. Said-Mohamed R, Allirot X, Sobgui M, Pasquet P. Determinants of overweight associated with stunting in preschool children of Yaounde, Cameroon. Ann Hum Biol. 2009; 36:146–161.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Report of Health Related Anthropometric Indices in 2–5 Years Old Children of Golestan Province of Iran in 2015
- Effect of rheumatoid arthritis on periodontitis: a historical cohort study
- Association of multiple anthropometric indices with in 944,760 elderly Chinese people
- Association between Changes in Anthropometric Indices and in Fasting Insulin Levels among Healthy Korean Adolescents: The JS High School Study
- Indices/Indicators Developed to Evaluate the “Creating Supportive Environments” Mechanism of the Ottawa Charter for Health Promotion: A Setting-Based Review on Healthy Environment Indices/ Indicators