Intest Res.
2018 Jul;16(3):445-457. 10.5217/ir.2018.16.3.445.
Magnetic resonance enterography predicts the prognosis of Crohn's disease
- Affiliations
-
- 1Department of Internal Medicine and Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea. GENIUSHEE@yuhs.ac
- 2Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. JSLIM1@yuhs.ac
- 3Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2417657
- DOI: http://doi.org/10.5217/ir.2018.16.3.445
Abstract
- BACKGROUND/AIMS
Magnetic resonance enterography (MRE) has emerged as an important tool in the diagnosis and follow-up of Crohn's disease (CD). The aim of this study was to evaluate whether MRE findings could predict the prognosis of CD.
METHODS
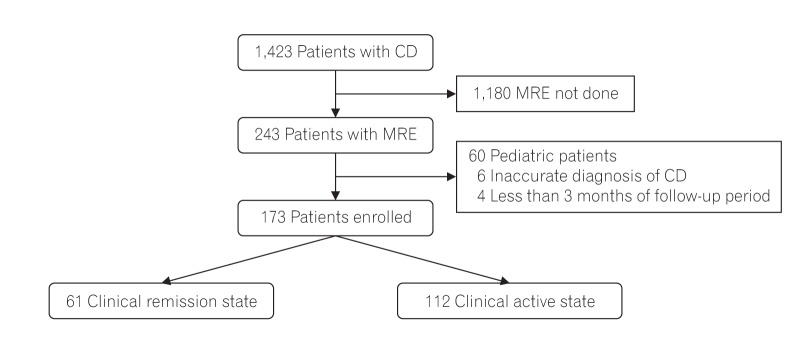
In this retrospective study, a total of 173 patients with clinical remission of CD (n=61) or active CD (n=112) were identified. The outcomes of clinical relapse, admission, surgery, and need for other medications according to the MRE findings were evaluated.
RESULTS
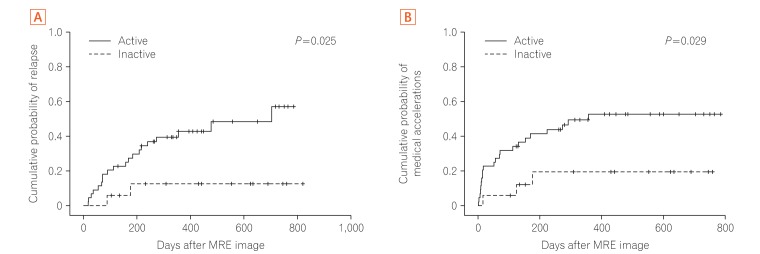
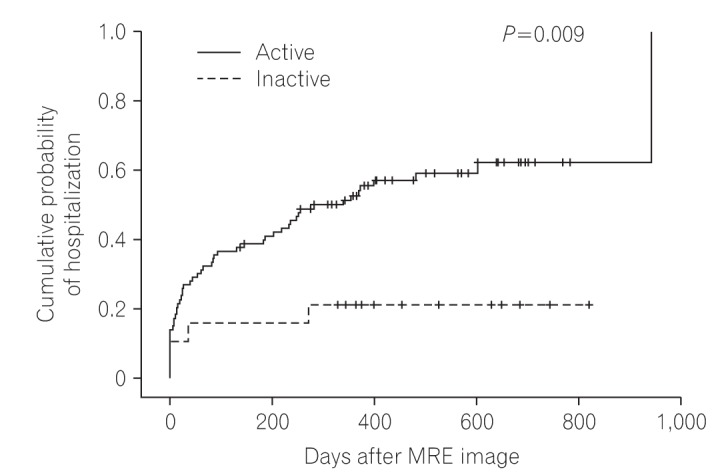
The presence of active inflammation on MRE was observed in 93 (83%) patients with clinically active CD and in 44 (72.1%) patients with clinical remission of CD, without a statistically significant difference (P=0.091). In multivariate analysis, active inflammation on MRE increased the risk for clinical relapse (hazard ratio [HR], 6.985; 95% confidence interval [CI], 1.024-47.649) in patients with clinical remission of CD. In patients with clinically active CD, active inflammation on MRE increased the risk for CD-related hospitalization (HR, 2.970; 95% CI, 1.006-8.772).
CONCLUSIONS
The presence of active inflammation on MRE was significantly associated with poor prognosis both in patients with clinical remission of CD and in those with active CD.
MeSH Terms
Figure
Cited by 1 articles
-
Crohn’s disease at radiological imaging: focus on techniques and intestinal tract
Giuseppe Cicero, Silvio Mazziotti
Intest Res. 2021;19(4):365-378. doi: 10.5217/ir.2020.00097.
Reference
-
1. Martin DR, Lauenstein T, Sitaraman SV. Utility of magnetic resonance imaging in small bowel Crohn's disease. Gastroenterology. 2007; 133:385–390. PMID: 17681157.
Article2. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015; 110:1324–1338. PMID: 26303131.3. Peyrin-Biroulet L, Reinisch W, Colombel JF, et al. Clinical disease activity, C-reactive protein normalisation and mucosal healing in Crohn's disease in the SONIC trial. Gut. 2014; 63:88–95. PMID: 23974954.
Article4. Maglinte DD, Chernish SM, Kelvin FM, O'Connor KW, Hage JP. Crohn disease of the small intestine: accuracy and relevance of enteroclysis. Radiology. 1992; 184:541–545. PMID: 1620862.
Article5. Sinha R, Verma R, Verma S, Rajesh A. MR enterography of Crohn disease: part 1, rationale, technique, and pitfalls. AJR Am J Roentgenol. 2011; 197:76–79. PMID: 21701013.
Article6. Ohtsuka K, Takenaka K, Kitazume Y, et al. Magnetic resonance enterography for the evaluation of the deep small intestine in Crohn's disease. Intest Res. 2016; 14:120–126. PMID: 27175112.
Article7. Fornasa F, Benassuti C, Benazzato L. Role of magnetic resonance enterography in differentiating between fibrotic and active inflammatory small bowel stenosis in patients with Crohn's disease. J Clin Imaging Sci. 2011; 1:35. PMID: 21966632.
Article8. Koh DM, Miao Y, Chinn RJ, et al. MR imaging evaluation of the activity of Crohn's disease. AJR Am J Roentgenol. 2001; 177:1325–1332. PMID: 11717076.
Article9. Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008; 247:64–79. PMID: 18372465.
Article10. Takenaka K, Ohtsuka K, Kitazume Y, et al. Comparison of magnetic resonance and balloon enteroscopic examination of the small intestine in patients with Crohn's disease. Gastroenterology. 2014; 147:334–342. PMID: 24732015.
Article11. Fiorino G, Bonifacio C, Peyrin-Biroulet L, et al. Prospective comparison of computed tomography enterography and magnetic resonance enterography for assessment of disease activity and complications in ileocolonic Crohn's disease. Inflamm Bowel Dis. 2011; 17:1073–1080. PMID: 21484958.
Article12. Deepak P, Fletcher JG, Fidler JL, et al. Radiological response is associated with better long-term outcomes and is a potential treatment target in patients with small bowel Crohn's disease. Am J Gastroenterol. 2016; 111:997–1006. PMID: 27166131.
Article13. Best WR, Becktel JM, Singleton JW. Rederived values of the eight coefficients of the Crohn's disease activity index (CDAI). Gastroenterology. 1979; 77(4 Pt 2):843–846. PMID: 467941.
Article14. Costa F, Mumolo MG, Ceccarelli L, et al. Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn's disease. Gut. 2005; 54:364–368. PMID: 15710984.
Article15. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19(Suppl A):5A–36A.
Article16. Masselli G, Gualdi G. MR imaging of the small bowel. Radiology. 2012; 264:333–348. PMID: 22821694.
Article17. Tolan DJ, Greenhalgh R, Zealley IA, Halligan S, Taylor SA. MR enterographic manifestations of small bowel Crohn disease. Radiographics. 2010; 30:367–384. PMID: 20228323.
Article18. Grand DJ, Beland M, Harris A. Magnetic resonance enterography. Radiol Clin North Am. 2013; 51:99–112. PMID: 23182510.
Article19. Steward MJ, Punwani S, Proctor I, et al. Non-perforating small bowel Crohn's disease assessed by MRI enterography: derivation and histopathological validation of an MR-based activity index. Eur J Radiol. 2012; 81:2080–2088. PMID: 21924572.
Article20. Rimola J, Rodriguez S, García-Bosch O, et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn's disease. Gut. 2009; 58:1113–1120. PMID: 19136510.
Article21. Singleton JW. Clinical activity assessment in inflammatory bowel disease. Dig Dis Sci. 1987; 32(12 Suppl):42S–45S. PMID: 3319457.
Article22. Carter MJ, Lobo AJ, Travis SP. IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004; 53(Suppl 5):V1–V16. PMID: 15306569.
Article23. Kim DH, Cheon JH. Intestinal Behçet's disease: a true inflammatory bowel disease or merely an intestinal complication of systemic vasculitis? Yonsei Med J. 2016; 57:22–32. PMID: 26632379.
Article24. Lichtenstein GR, Hanauer SB, Sandborn WJ. Practice Parameters Committee of American College of Gastroenterology. Management of Crohn's disease in adults. Am J Gastroenterol. 2009; 104:465–483. PMID: 19174807.
Article25. Lémann M, Mary JY, Colombel JF, et al. A randomized, double-blind, controlled withdrawal trial in Crohn's disease patients in long-term remission on azathioprine. Gastroenterology. 2005; 128:1812–1818. PMID: 15940616.
Article26. Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010; 362:1383–1395. PMID: 20393175.
Article27. Rutgeerts P, Diamond RH, Bala M, et al. Scheduled maintenance treatment with infliximab is superior to episodic treatment for the healing of mucosal ulceration associated with Crohn's disease. Gastrointest Endosc. 2006; 63:433–442. PMID: 16500392.
Article28. Colombel JF, Rutgeerts PJ, Sandborn WJ, et al. Adalimumab induces deep remission in patients with Crohn's disease. Clin Gastroenterol Hepatol. 2014; 12:414–422.e5. PMID: 23856361.
Article29. Colombel JF, Louis E, Peyrin-Biroulet L, Sandborn WJ, Panaccione R. Deep remission: a new concept? Dig Dis. 2012; 30(Suppl 3):107–111. PMID: 23295700.
Article30. Makanyanga JC, Taylor SA. Current and future role of MR enterography in the management of Crohn disease. AJR Am J Roentgenol. 2013; 201:56–64. PMID: 23789658.
Article31. Fowler KJ, Dassopoulos T, Raptis C. Magnetic resonance enterography in the evaluation of Crohn's disease: a primer for the gastroenterologist. Inflamm Bowel Dis. 2014; 20:2179–2188. PMID: 25054338.32. Greenup AJ, Bressler B, Rosenfeld G. Medical imaging in small bowel Crohn's disease-computer tomography enterography, magnetic resonance enterography, and ultrasound: “Which One Is the Best for What?”. Inflamm Bowel Dis. 2016; 22:1246–1261. PMID: 27070909.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed Tomography Enterography and Magnetic Resonance Enterography in the Diagnosis of Crohn's Disease
- Role of Computed Tomography Enterography/Magnetic Resonance Enterography: Is It in Prime Time?
- Pediatric Magnetic Resonance Enterography: Focused on Crohn's Disease
- Preparation, Technique, and Imaging of Computed Tomography/Magnetic Resonance Enterography
- A Look into the Small Bowel in Crohn's Disease