J Korean Med Sci.
2017 Jan;32(1):124-129. 10.3346/jkms.2017.32.1.124.
Unfavorable Course of Subclinical Hypothyroidism in Children with Hashimoto's Thyroiditis Compared to Those with Isolated Non-Autoimmune Hyperthyrotropinemia
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. nina337@snu.ac.kr
- 2Department of Pediatrics, Kyung Hee University College of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Seoul Metropolitan Government, Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2417594
- DOI: http://doi.org/10.3346/jkms.2017.32.1.124
Abstract
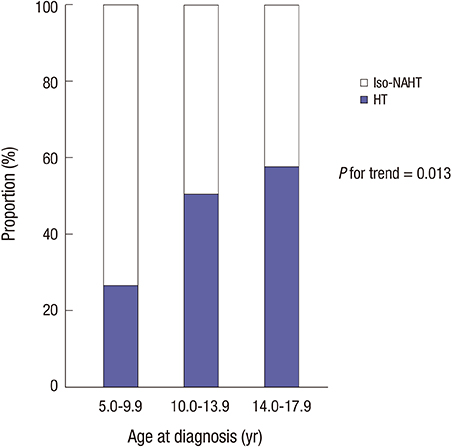
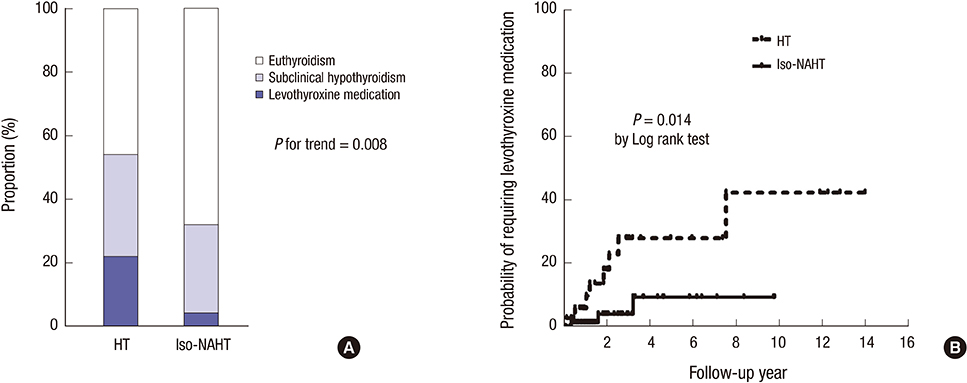
- Subclinical hypothyroidism (SCH) is a common problem in pediatric population, and the natural history of SCH varies depending on its etiology. Whether Hashimoto's thyroiditis (HT) negatively affects the natural course of SCH was investigated in pediatric patients without concomitant diseases. Predictors for levothyroxine medication were also evaluated. Medical records of 109 children with SCH (91 girls, 5−18 years) diagnosed between 2005 and 2014 were retrospectively reviewed. Patients were classified into HT (n = 37) and isolated non-autoimmune hyperthyrotropinemia (iso-NAHT, n = 72). During median 2 years of follow-up, only 10.1% of SCH patients eventually initiated levothyroxine, and HT patients showed a higher probability of requiring levothyroxine medication than iso-NAHT patients (21.6% vs. 4.2%). Underlying HT independently predicted deterioration of thyroid function, leading to levothyroxine medication (hazard ratios [HRs], 4.6 vs. iso-NAHT, P = 0.025). High titers of anti-thyroglobulin antibodies (TGAbs) predicted later medication in the HT group (HRs, 28.2 vs. normal TGAbs, P = 0.013). Most pediatric SCH showed benign and self-remitting courses. Underlying HT significantly increases the risk for levothyroxine medication, especially with high titers of TGAbs.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinol Metab. 2021;36(3):500-513. doi: 10.3803/EnM.2021.1066.Subclinical hypothyroidism in children: updates for pediatricians
Kotb Abbass Metwalley, Hekma Saad Farghaly
Ann Pediatr Endocrinol Metab. 2021;26(2):80-85. doi: 10.6065/apem.2040242.121.
Reference
-
1. Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012; 379:1142–1154.2. Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH, Franklyn JA, Hershman JM, Burman KD, Denke MA, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004; 291:228–238.3. Wu T, Flowers JW, Tudiver F, Wilson JL, Punyasavatsut N. Subclinical thyroid disorders and cognitive performance among adolescents in the United States. BMC Pediatr. 2006; 6:12.4. Lazar L, Frumkin RB, Battat E, Lebenthal Y, Phillip M, Meyerovitch J. Natural history of thyroid function tests over 5 years in a large pediatric cohort. J Clin Endocrinol Metab. 2009; 94:1678–1682.5. Rapa A, Monzani A, Moia S, Vivenza D, Bellone S, Petri A, Teofoli F, Cassio A, Cesaretti G, Corrias A, et al. Subclinical hypothyroidism in children and adolescents: a wide range of clinical, biochemical, and genetic factors involved. J Clin Endocrinol Metab. 2009; 94:2414–2420.6. Radetti G, Maselli M, Buzi F, Corrias A, Mussa A, Cambiaso P, Salerno M, Cappa M, Baiocchi M, Gastaldi R, et al. The natural history of the normal/mild elevated TSH serum levels in children and adolescents with Hashimoto’s thyroiditis and isolated hyperthyrotropinaemia: a 3-year follow-up. Clin Endocrinol (Oxf). 2012; 76:394–398.7. Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014; 3:76–94.8. Wasniewska M, Salerno M, Cassio A, Corrias A, Aversa T, Zirilli G, Capalbo D, Bal M, Mussa A, De Luca F. Prospective evaluation of the natural course of idiopathic subclinical hypothyroidism in childhood and adolescence. Eur J Endocrinol. 2009; 160:417–421.9. Bona G, Prodam F, Monzani A. Subclinical hypothyroidism in children: natural history and when to treat. J Clin Res Pediatr Endocrinol. 2013; 5:Suppl 1. 23–28.10. Aversa T, Valenzise M, Corrias A, Salerno M, De Luca F, Mussa A, Rezzuto M, Lombardo F, Wasniewska M. Underlying Hashimoto’s thyroiditis negatively affects the evolution of subclinical hypothyroidism in children irrespective of other concomitant risk factors. Thyroid. 2015; 25:183–187.11. Monzani A, Prodam F, Rapa A, Moia S, Agarla V, Bellone S, Bona G. Endocrine disorders in childhood and adolescence. Natural history of subclinical hypothyroidism in children and adolescents and potential effects of replacement therapy: a review. Eur J Endocrinol. 2012; 168:R1–11.12. Korea Center for Disease Control and Prevention. The Korean Pediatric Society. The Committee for the Development of Growth Standard for Korean Children and Adolescents. 2007 Korean children and adolescents growth standard. accessed on 10 July 2015. Available at www.cdc.go.kr/CDC/.13. World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring their Elimination: a Guide for Programme Manager. 3rd ed. Geneva: World Health Organization;2007. p. 24–46.14. Calebiro D, Gelmini G, Cordella D, Bonomi M, Winkler F, Biebermann H, de Marco A, Marelli F, Libri DV, Antonica F, et al. Frequent TSH receptor genetic alterations with variable signaling impairment in a large series of children with nonautoimmune isolated hyperthyrotropinemia. J Clin Endocrinol Metab. 2012; 97:E156–60.15. O’Grady MJ, Cody D. Subclinical hypothyroidism in childhood. Arch Dis Child. 2011; 96:280–284.16. Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008; 29:76–131.17. Radetti G, Gottardi E, Bona G, Corrias A, Salardi S, Loche S; Study Group for Thyroid Diseases of the Italian Society for Pediatric Endocrinology and Diabetes (SIEDP/ISPED). The natural history of euthyroid Hashimoto’s thyroiditis in children. J Pediatr. 2006; 149:827–832.18. Helfand M; U.S. Preventive Services Task Force. Screening for subclinical thyroid dysfunction in nonpregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004; 140:128–141.19. Fleury Y, Van Melle G, Woringer V, Gaillard RC, Portmann L. Sex-dependent variations and timing of thyroid growth during puberty. J Clin Endocrinol Metab. 2001; 86:750–754.20. Kim SY, Lee YA, Jung HW, Kim HY, Lee HJ, Shin CH, Yang SW. Pediatric goiter: Can thyroid disorders be predicted at diagnosis and in follow-up? J Pediatr. 2016; 170:253–259.e1-2.21. Kaplowitz PB. Subclinical hypothyroidism in children: normal variation or sign of a failing thyroid gland? Int J Pediatr Endocrinol. 2010; 2010:281453.22. Gawlik A, Such K, Dejner A, Zachurzok A, Antosz A, Malecka-Tendera E. Subclinical hypothyroidism in children and adolescents: is it clinically relevant? Int J Endocrinol. 2015; 2015:691071.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Hyperthyroidism Following Postpartum Thyroiditis in a Woman with Hashimoto's Thyroiditis
- A Case of Hashimoto's Thyroiditis Presented with Severe Hypertension and Thyrotoxicosis
- Association Kikuchi disease with Hashimoto thyroiditis: a case report and literature review
- Clinical Update in Aspects of the Management of Autoimmune Thyroid Diseases
- Autoimmune Thyroid Diseases