J Korean Neurosurg Soc.
2018 May;61(3):363-375. 10.3340/jkns.2018.0078.
Intraoperative Neurophysiological Monitoring : A Review of Techniques Used for Brain Tumor Surgery in Children
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Neurology, Stanford University, Stanford, CA, USA.
- 3Department of Neurosurgery, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. nsthomas@snu.ac.kr
- KMID: 2417361
- DOI: http://doi.org/10.3340/jkns.2018.0078
Abstract
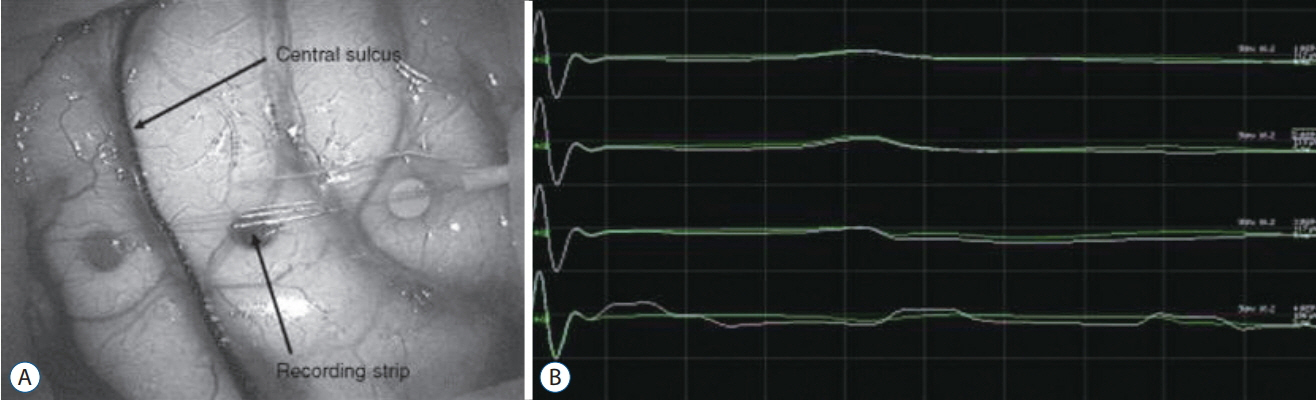
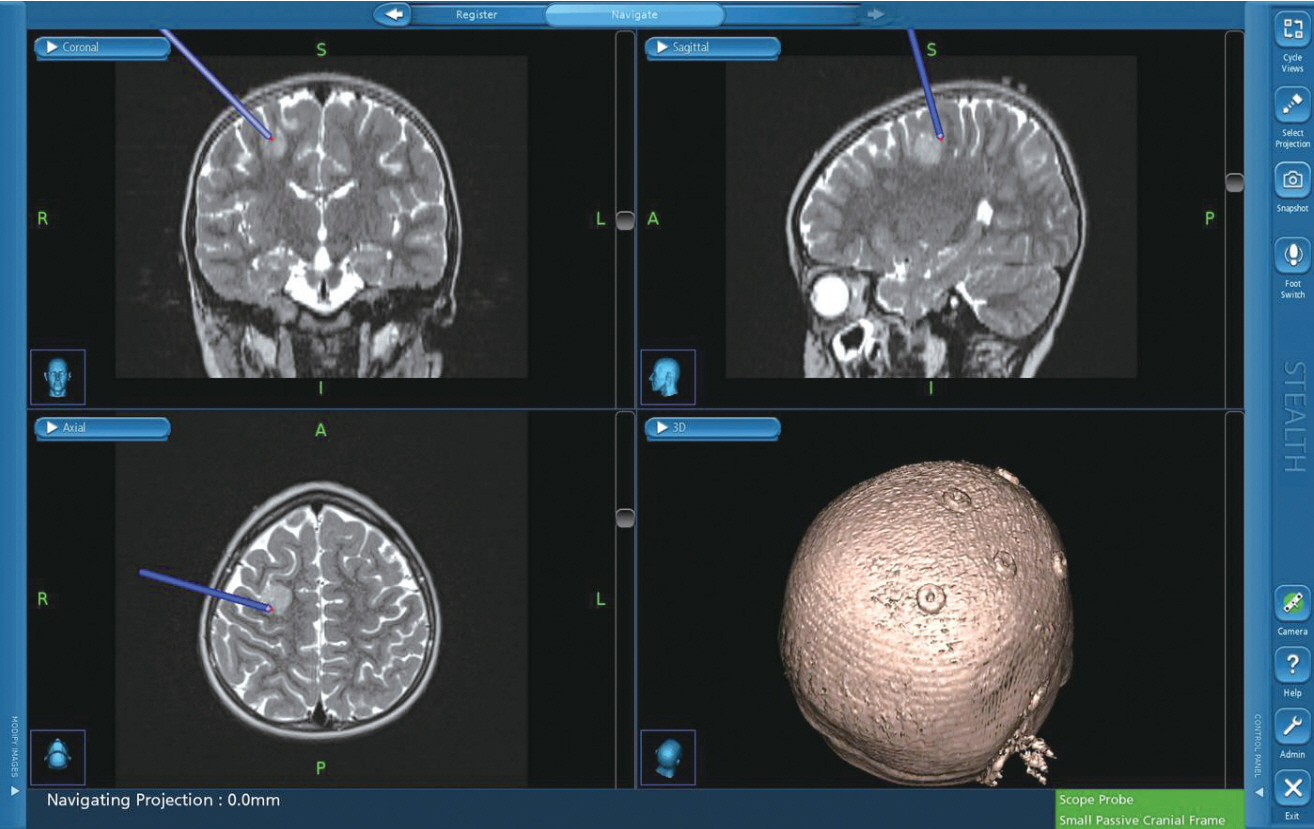
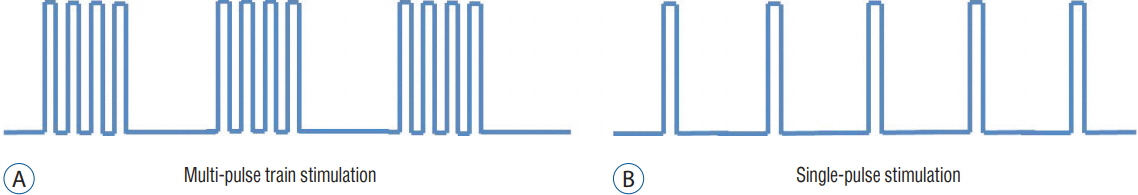
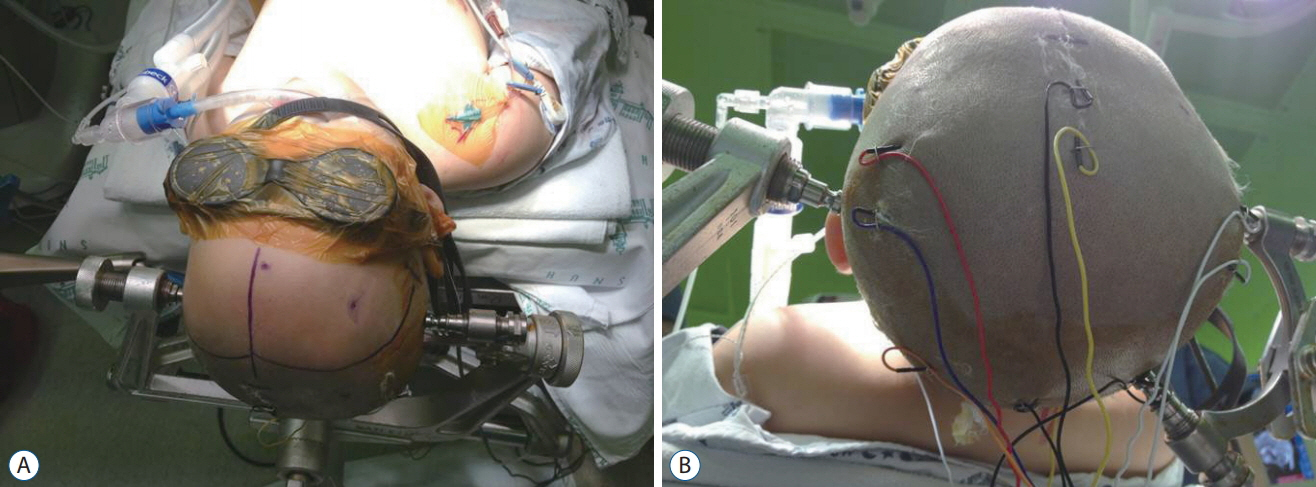
- Intraoperative monitoring (IOM) utilizes electrophysiological techniques as a surrogate test and evaluation of nervous function while a patient is under general anesthesia. They are increasingly used for procedures, both surgical and endovascular, to avoid injury during an operation, examine neurological tissue to guide the surgery, or to test electrophysiological function to allow for more complete resection or corrections. The application of IOM during pediatric brain tumor resections encompasses a unique set of technical issues. First, obtaining stable and reliable responses in children of different ages requires detailed understanding of normal ageadjusted brain-spine development. Neurophysiology, anatomy, and anthropometry of children are different from those of adults. Second, monitoring of the brain may include risk to eloquent functions and cranial nerve functions that are difficult with the usual neurophysiological techniques. Third, interpretation of signal change requires unique sets of normative values specific for children of that age. Fourth, tumor resection involves multiple considerations including defining tumor type, size, location, pathophysiology that might require maximal removal of lesion or minimal intervention. IOM techniques can be divided into monitoring and mapping. Mapping involves identification of specific neural structures to avoid or minimize injury. Monitoring is continuous acquisition of neural signals to determine the integrity of the full longitudinal path of the neural system of interest. Motor evoked potentials and somatosensory evoked potentials are representative methodologies for monitoring. Free-running electromyography is also used to monitor irritation or damage to the motor nerves in the lower motor neuron level : cranial nerves, roots, and peripheral nerves. For the surgery of infratentorial tumors, in addition to free-running electromyography of the bulbar muscles, brainstem auditory evoked potentials or corticobulbar motor evoked potentials could be combined to prevent injury of the cranial nerves or nucleus. IOM for cerebral tumors can adopt direct cortical stimulation or direct subcortical stimulation to map the corticospinal pathways in the vicinity of lesion. IOM is a diagnostic as well as interventional tool for neurosurgery. To prove clinical evidence of it is not simple. Randomized controlled prospective studies may not be possible due to ethical reasons. However, prospective longitudinal studies confirming prognostic value of IOM are available. Furthermore, oncological outcome has also been shown to be superior in some brain tumors, with IOM. New methodologies of IOM are being developed and clinically applied. This review establishes a composite view of techniques used today, noting differences between adult and pediatric monitoring.
MeSH Terms
-
Adult
Anesthesia, General
Anthropometry
Brain Neoplasms*
Brain*
Child*
Cranial Nerves
Electromyography
Evoked Potentials, Auditory, Brain Stem
Evoked Potentials, Motor
Evoked Potentials, Somatosensory
Humans
Infratentorial Neoplasms
Intraoperative Neurophysiological Monitoring*
Longitudinal Studies
Monitoring, Intraoperative
Motor Neurons
Muscles
Neurophysiology
Neurosurgery
Peripheral Nerves
Prospective Studies
Figure
Reference
-
References
1. Anderson S, Loughnan B, Hetreed M. A technique for monitoring evoked potentials during scoliosis and brachial plexus surgery. Ann R Coll Surg Engl. 72:321–323. 1990.2. Angel A, GRATTON DA. The effect of anaesthetic agents on cerebral cortical responses in the rat. Br J Pharmacol. 76:541–549. 1982.
Article3. Brell M, Ibáñez J, Caral L, Ferrer E. Factors influencing surgical complications of intra-axial brain tumours. Acta Neurochir (Wien). 142:739–750. 2000.
Article4. Burke D, Hicks R, Stephen J, Woodforth I, Crawford M. Assessment of corticospinal and somatosensoty conduction simultaneously during scoliosis surgery. Electroencephalogr Clin Neurophysiol. 85:388–396. 1992.
Article5. Calancie B, Harris W, Broton JG, Alexeeva N, Green BA. “Threshold-level” multipulse transcranial electrical stimulation of motor cortex for intraoperative monitoring of spinal motor tracts: description of method and comparison to somatosensory evoked potential monitoring. J Neurosurg. 88:457–470. 1998.
Article6. Chang SD, López JR, Steinberg GK. Intraoperative electrical stimulation for identification of cranial nerve nuclei. Muscle Nerve. 22:1538–1543. 1999.
Article7. De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol. 30:2559–2565. 2012.
Article8. Debatisse D, Pralong E, Guerit J, Bisdorff A. Recording click-evoked myogenic potentials (CEMPs) with a setup for brainstem auditory evoked potentials (BAEPs). Neurophysiol Clin. 35:109–117. 2005.
Article9. Deletis V, Shils J. Neurophysiology in neurosurgery. New York: Elsevier;2002. p. 25–51.10. Deletis V, Rodi Z, Amassian VE. Neurophysiological mechanisms underlying motor evoked potentials in anesthetized humans. Part 2. relationship between epidurally and muscle recorded MEPs in man. Clin Neurophysiol. 112:445–452. 2001.
Article11. Deletis V, Rogić M, Fernández-Conejero I, Gabarrós A, Jerončić A. Neurophysiologic markers in laryngeal muscles indicate functional anatomy of laryngeal primary motor cortex and premotor cortex in the caudal opercular part of inferior frontal gyrus. Clin Neurophysiol. 125:1912–1922. 2014.
Article12. Deletis V, Sala F. Intraoperative neurophysiological monitoring of the spinal cord during spinal cord and spine surgery: a review focus on the corticospinal tracts. Clin Neurophysiol. 119:248–264. 2008.
Article13. Dong CC, MacDonald DB, Akagami R, Westerberg B, AlKhani A, Kanaan I, et al. Intraoperative facial motor evoked potential monitoring with transcranial electrical stimulation during skull base surgery. Clin Neurophysiol. 116:588–596. 2005.
Article14. Dubois MY, Sato S, Chassy J, Macnamara TE. Effects of enflurane on brainstem auditory evoked responses in humans. Anesth Analg. 61:898–902. 1982.
Article15. Duffau H, Lopes M, Gatignol P, Mandonnet E, Taillandier L, Leroy M, et al. 745 contribution of intraoperative corticosubcortical stimulations in surgery of low-grade gliomas: a comparative study between two series without and with functional mapping. Neurosurgery. 55:467. 2004.
Article16. Eggermont J. Physiology of the developing auditory system. In : Sandra E Trehub, Bruce Schneider, editors. Auditory development in infancy. New York: Springer;1985. p. 21–45.17. Eisner W, Schmid UD, Reulen HJ, Oeckler R, Olteanu-Nerbe V, Gall C, et al. The mapping and continuous monitoring of the intrinsic motor nuclei during brain stem surgery. Neurosurgery. 37:255–265. 1995.
Article18. Ferber-Viart C, Dubreuil C, Duclaux R. Vestibular evoked myogenic potentials in humans: a review. Acta Otolaryngol. 119:6–15. 1999.
Article19. Ferber-Viart C, Duclaux R, Colleaux B, Dubreuil C. Myogenic vestibularevoked potentials in normal subjects: a comparison between responses obtained from sternomastoid and trapezius muscles. Acta Otolaryngol. 117:472–481. 1997.
Article20. Frei FJ, Ryhult SE, Duitmann E, Hasler CC, Luetschg J, Erb TO. Intraoperative monitoring of motor-evoked potentials in children undergoing spinal surgery. Spine (Phila Pa 1976). 32:911–917. 2007.
Article21. Fulkerson DH, Satyan KB, Wilder LM, Riviello JJ, Stayer SA, Whitehead WE, et al. Intraoperative monitoring of motor evoked potentials in very young children. J Neurosurg Pediatr. 7:331–337. 2011.
Article22. Goldring S. A method for surgical management of focal epilepsy, especially as it relates to children. J Neurosurg. 49:344–356. 1978.
Article23. Goldring S, Gregorie EM. Surgical management of epilepsy using epidural recordings to localize the seizure focus: review of 100 cases. J Neurosurg. 60:457–466. 1984.
Article24. Gunnarsson T, Krassioukov AV, Sarjeant R, Fehlings MG. Real-time continuous intraoperative electromyographic and somatosensory evoked potential recordings in spinal surgery: correlation of clinical and electrophysiologic findings in a prospective, consecutive series of 213 cases. Spine (Phila Pa 1976). 29:677–684. 2004.
Article25. Halonen JP, Jones SJ, Edgar MA, Ransford AO. Conduction properties of epidurally recorded spinal cord potentials following lower limb stimulation in man. Electroencephalogr Clin Neurophysiol. 74:161–174. 1989.
Article26. Helmers SL, Hall JE. Intraoperative somatosensory evoked potential monitoring in pediatrics. J Pediatr Orthop. 14:592–598. 1994.
Article27. Hicks RG, Burke DJ, Stephen JP. Monitoring spinal cord function during scoliosis surgery with Cotrel-Dubousset instrumentation. Med J Aust. 154:82–86. 1991.
Article28. Hwang H, Wang KC, Bang MS, Shin HI, Kim SK, Phi JH, et al. Optimal stimulation parameters for intraoperative bulbocavernosus reflex in infants. J Neurosurg Pediatr. 20:464–470. 2017.
Article29. James MFM, Thornton C, Jones JG. Halothane anaesthesia changes the early components of the auditory evoked response in man. Br J Anaesth. 54:787. 1982.30. Jasper H. Electrocorticograms in man. Electroencephalogr Clin Neurophysiol. 2:16–29. 1949.31. Jimenez JC, Sani S, Braverman B, Deutsch H, Ratliff JK. Palsies of the fifth cervical nerve root after cervical decompression: prevention using continuous intraoperative electromyography monitoring. J Neurosurg Spine. 3:92–97. 2005.
Article32. Jones S, Harrison R, Koh K, Mendoza N, Crockard H. Motor evoked potential monitoring during spinal surgery: responses of distal limb muscles to transcranial cortical stimulation with pulse trains. Electroencephalogr Clin Neurophysiol. 100:375–383. 1996.
Article33. Kalkman CJ, Drummond JC, Ribberink AA. Low concentrations of isoflurane abolish motor evoked responses to transcranial electrical stimulation during nitrous oxide/opioid anesthesia in humans. Anesth Analg. 73:410–415. 1991.
Article34. Levy SR. Somatosensory Evoked Potentials. In : Chiappa KH, editor. Evoked potentials in clinical medicine. ed 3. Philadelphia: Lippincott-Raven;1997. p. 453–466.35. Lo YL, Dan YF, Tan YE, Nurjannah S, Tan SB, Tan CT, et al. Intraoperative motor-evoked potential monitoring in scoliosis surgery: comparison of desflurane/nitrous oxide with propofol total intravenous anesthetic regimens. J Neurosurg Anesthesiol. 18:211–214. 2006.
Article36. Maguire J, Wallace S, Madiga R, Leppanen R, Draper V. Evaluation of intrapedicular screw position using intraoperative evoked electromyography. Spine (Phila Pa 1976). 20:1068–1074. 1995.
Article37. Manninen PH, Patterson S, Lam AM, Gelb AW, Nantau WE. Evoked potential monitoring during posterior fossa aneurysm surgery: a comparison of two modalities. Can J Anaesth. 41:92–97. 1994.
Article38. Marshall C, walker ae. Electrocorticography. Bull Johns Hopkins Hosp. 85:344–359. 1949.39. Matthies C, Samii M. Management of vestibular schwannomas (acoustic neuromas): the value of neurophysiology for intraoperative monitoring of auditory function in 200 cases. Neurosurgery . 40:459–466. discussion 466-468. 1997.
Article40. Merton P, Morton H. Stimulation of the cerebral cortex in the intact human subject. Nature. 285:227. 1980.
Article41. Møller MB, Møller AR. Loss of auditory function in microvascular decompression for hemifacial spasm: results in 143 consecutive cases. J Neurosurg. 63:17–20. 1985.
Article42. Morota N, Deletis V, Constantini S, Kofler M, Cohen H, Epstein FJ. The role of motor evoked potentials during surgery for intramedullary spinal cord tumors. Neurosurgery. 41:1327–1336. 1997.
Article43. Morota N, Deletis V, Epstein FJ, Kofler M, Abbott R, Lee M, et al. Brain stem mapping: neurophysiological localization of motor nuclei on the floor of the fourth ventricle. Neurosurgery. 37:922–929. discussion 929-930. 1995.44. Nash CL Jr, Brodkey J. Clinical application of spinal-cord monitoring for operative treatment of spinal disease. Cleveland: Case Western Reserve University;1977. p. 140.45. Nash CL Jr, Lorig RA, Schatzinger LA, Brown RH. Spinal cord monitoring during operative treatment of the spine. Clin Orthop Relat Res. (126):100–105. 1977.
Article46. Nash CL Jr, Schatzinger L, Lorig R. Intraoperative monitoring of spinal cord function during scoliosis spine surgery. J Bone Joint Surg Am. 56:765. 1974.47. Neu M, Strauss C, Romstöck J, Bischoff B, Fahlbusch R. The prognostic value of intraoperative BAEP patterns in acoustic neurinoma surgery. Clin Neurophysiol. 110:1935–1941. 1999.
Article48. Nguyen BH, Javel E, Levine SC. Physiologic identification of eighth nerve subdivisions: direct recordings with bipolar and monopolar electrodes. Am J Otol. 20:522–534. 1999.49. Nuwer M, Dawson E. Intraoperative evoked potential monitoring of the spinal cord: enhanced stability of cortical recordings. Electroencephalogr Clin Neurophysiol. 59:318–327. 1984.
Article50. Nuwer MR, Aminoff M, Desmedt J, Eisen AA, Goodin D, Matsuoka S, et al. IFCN recommended standards for short latency somatosensory evoked potentials. Report of an IFCN committee. International federation of clinical neurophysiology. Electroencephalogr Clin Neurophysiol. 91:6–11. 1994.
Article51. Nuwer MR, Dawson EG, Carlson LG, Kanim LE, Sherman JE. Somatosensory evoked potential spinal cord monitoring reduces neurologic deficits after scoliosis surgery: results of a large multicenter survey. Electroencephalogr Clin Neurophysiol. 96:6–11. 1995.
Article52. Nuwer MR, Emerson RG, Galloway G, Legatt AD, Lopez J, Minahan R, et al. Evidence-based guideline update: intraoperative spinal monitoring with somatosensory and transcranial electrical motor evoked potentials report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology and the American Clinical Neurophysiology Society. Neurology. 78:585–589. 2012.
Article53. Ohue S, Kohno S, Inoue A, Yamashita D, Harada H, Kumon Y, et al. Accuracy of diffusion tensor magnetic resonance imaging-based tractography for surgery of gliomas near the pyramidal tract: a significant correlation between subcortical electrical stimulation and postoperative tractography. Neurosurgery. 70:283–293. discussion 294. 2012.54. Sawaya R, Hammoud M, Schoppa D, Hess KR, Wu SZ, Shi WM, et al. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery. 42:1044–1055. discussion 1055-1056. 1998.
Article55. Pechstein U, Cedzich C, Nadstawek J, Schramm J. Transcranial highfrequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery. 39:335–343. discussion 343-344. 1996.
Article56. Penfield W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain. 60:389–443. 1937.
Article57. Prell J, Rampp S, Romstöck J, Fahlbusch R, Strauss C. Train time as a quantitative electromyographic parameter for facial nerve function in patients undergoing surgery for vestibular schwannoma. J Neurosurg. 106:826–832. 2007.
Article58. Purdon PL, Sampson A, Pavone KJ, Brown EN. Clinical electroencephalography for anesthesiologists: part I: background and basic signatures. Anesthesiology. 123:937–960. 2015.59. Raabe A, Beck J, Schucht P, Seidel K. Continuous dynamic mapping of the corticospinal tract during surgery of motor eloquent brain tumors: evaluation of a new method. J Neurosurg. 120:1015–1024. 2014.
Article60. Radtke RA, Erwin CW, Wilkins RH. Intraoperative brainstem auditory evoked potentials: significant decrease in postoperative morbidity. Neurology. 39(2 Pt 1):187–191. 1989.
Article61. Romstöck J, Strauss C, Fahlbusch R. Continuous electromyography monitoring of motor cranial nerves during cerebellopontine angle surgery. J Neurosurg. 93:586–593. 2000.
Article62. Saito T, Tamura M, Muragaki Y, Maruyama T, Kubota Y, Fukuchi S, et al. Intraoperative cortico-cortical evoked potentials for the evaluation of language function during brain tumor resection: initial experience with 13 cases. J Neurosurg. 121:827–838. 2014.
Article63. Schucht P, Seidel K, Beck J, Murek M, Jilch A, Wiest R, et al. Intraoperative monopolar mapping during 5-ALA-guided resections of glioblastomas adjacent to motor eloquent areas: evaluation of resection rates and neurological outcome. Neurosurg focus. 37:E16. 2014.
Article64. Sharbrough FW, Messick JM Jr, Sundt TM Jr. Correlation of continuous electroencephalograms with cerebral blood flow measurements during carotid endarterectomy. Stroke. 4:674–683. 1973.
Article65. Simon MV, Chiappa KH, Borges LF. Phase reversal of somatosensory evoked potentials triggered by gracilis tract stimulation: case report of a new technique for neurophysiologic dorsal column mapping. Neurosurgery. 70:E783–E788. 2012.
Article66. Slimp JC. Electrophysiologic intraoperative monitoring for spine procedures. Phys Med Rehabil Clin N Am. 15:85–105. 2004.
Article67. Sloan T. Anesthesia and intraoperative neurophysiological monitoring in children. Childs Nerv Syst. 26:227–235. 2010.
Article68. Stone JL, Ghaly RF, Levy WJ, Kartha R, Krinsky L, Roccaforte P. A comparative analysis of enflurane anesthesia on primate motor and somatosensory evoked potentials. Electroencephalogr Clin Neurophysiol. 84:180–187. 1992.
Article69. Strauss C, Romstöck J, Nimsky C, Fahlbusch R. Intraoperative identification of motor areas of the rhomboid fossa using direct stimulation. J Neurosurg. 79:393–399. 1993.
Article70. Szelényi A, Joksimovic B, Seifert V. Intraoperative risk of seizures associated with transient direct cortical stimulation in patients with symptomatic epilepsy. J Clin Neurophysiol. 24:39–43. 2007.
Article71. Szelényi A, Senft C, Jardan M, Forster M, Franz K, Seifert V, et al. Intraoperative subcortical electrical stimulation : a comparison of two methods. Clin Neurophysiol. 122:1470–1475. 2011.
Article72. Tanaka Y, Kawaguchi M, Noguchi Y, Yoshitani K, Kawamata M, Masui K, et al. Systematic review of motor evoked potentials monitoring during thoracic and thoracoabdominal aortic aneurysm open repair surgery: a diagnostic meta-analysis. J Anesth. 30:1037–1050. 2016.
Article73. Taniguchi M, Cedzich C, Schramm J. Modification of cortical stimulation for motor evoked potentials under general anesthesia: technical description. Neurosurgery. 32:219–226. 1993.
Article74. Taniguchi M, Nadstawek J, Pechstein U, Schramm J. Total intravenous anesthesia for improvement of intraoperative monitoring of somatosensory evoked potentials during aneurysm surgery. Neurosurgery. 31:891–897. discussion 897. 1992.
Article75. Thompson JE. Surgery for cerebrovascular insufficiency (stroke): with special emphasis on carotid endarterectomy. Springfie: Thomas;1968.76. Wood CC, Spencer DD, Allison T, McCarthy G, Williamson PD, Goff WR. Localization of human sensorimotor cortex during surgery by cortical surface recording of somatosensory evoked potentials. J Neurosurg. 68:99–111. 1988.
Article77. Wylie EJ, Ehrenfeld WK. Extracranial occlusive cerebrovascular disease: diagnosis and management. Philadelphia: WB Saunders Company;1970.78. Yanni DS, Ulkatan S, Deletis V, Barrenechea IJ, Sen C, Perin NI. Utility of neurophysiological monitoring using dorsal column mapping in intramedullary spinal cord surgery. J Neurosurg Spine. 12:623–628. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical practice guidelines for intraoperative neurophysiological monitoring: 2020 update
- Mechanisms underlying brain monitoring during anesthesia: limitations, possible improvements, and perspectives
- Intraoperative Neurophysiologic Monitoring: Basic Principles and Recent Update
- Intraoperative Neurophysiological Monitoring during Microvascular Decompression Surgery for Hemifacial Spasm
- Intraoperative Neurophysiological Monitoring for Spinal Cord Tumor Surgery: Comparison of Motor and Somatosensory Evoked Potentials According to Tumor Types