Yeungnam Univ J Med.
2018 Jun;35(1):94-98. 10.12701/yujm.2018.35.1.94.
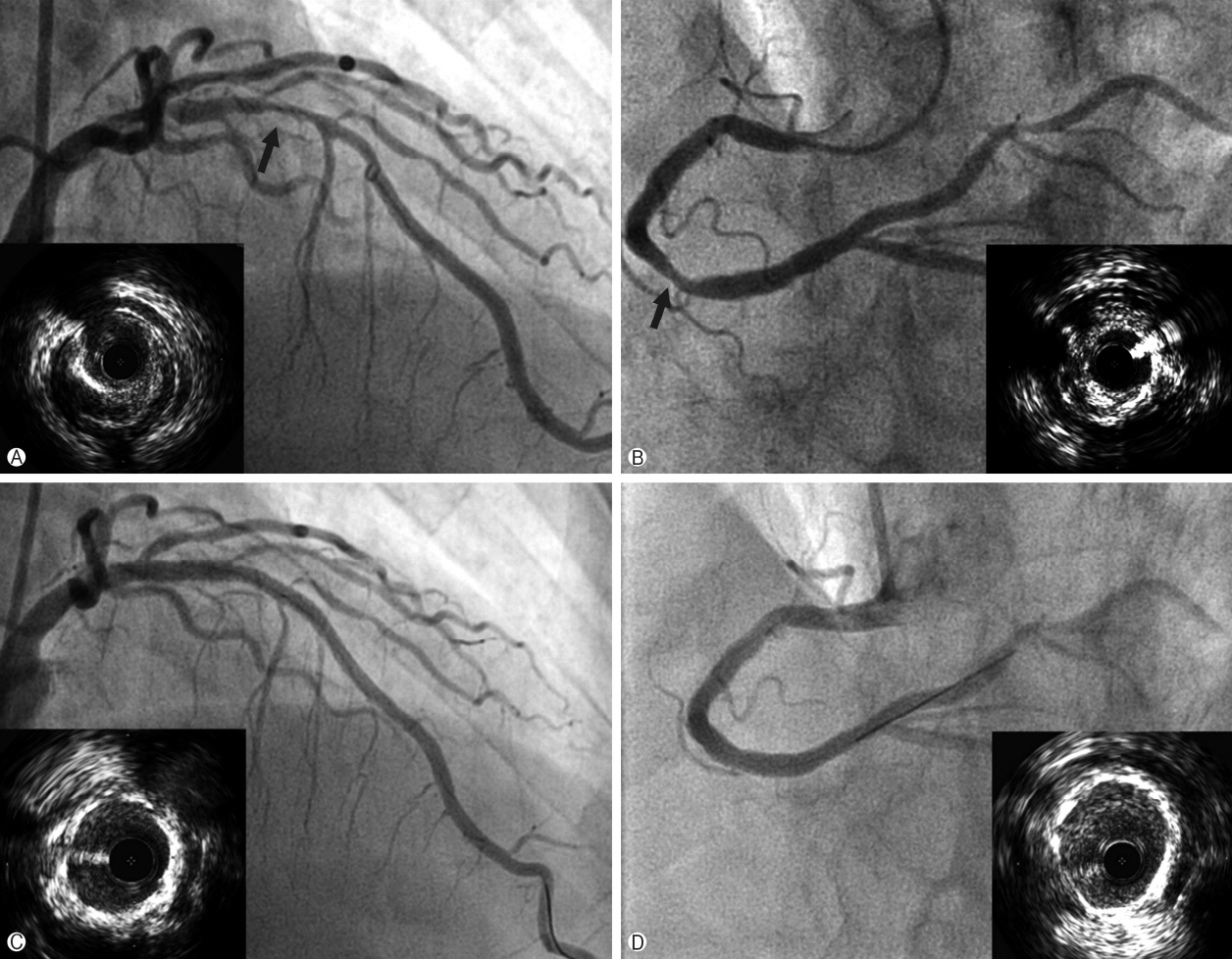
Successful transradial intervention via a radial recurrent artery branch from the radioulnar alpha loop using a sheathless guiding catheter
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Daejeon Veterans Hospital, Daejeon, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. sgahn@yonsei.ac.kr
- KMID: 2415740
- DOI: http://doi.org/10.12701/yujm.2018.35.1.94
Abstract
- The radial artery is generally the preferred access route in coronary angiography and coronary intervention. However, small size, spasm, and anatomical variations concerning the radial artery are major limitations of transradial coronary intervention (TRI). We describe a successful case involving a patient with coronary artery disease who underwent TRI via a well-developed radial recurrent artery branch from the radioulnar alpha loop using a sheathless guiding catheter.
MeSH Terms
Figure
Reference
-
1. Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009; 157:132–40.
Article2. Pristipino C, Trani C, Nazzaro MS, Berni A, Patti G, Patrizi R, et al. Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterization: results from the PREVAIL study. Heart. 2009; 95:476–82.
Article3. Saito S, Miyake S, Hosokawa G, Tanaka S, Kawamitsu K, Kaneda H, et al. Transradial coronary intervention in Japanese patients. Catheter Cardiovasc Interv. 1999; 46:37–41.
Article4. Franchi E, Marino P, Biondi-Zoccai GG, De Luca G, Vassanelli C, Agostoni P. Transradial versus transfemoral approach for percutaneous coronary procedures. Curr Cardiol Rep. 2009; 11:391–7.
Article5. Youn YJ, Yoon J, Han SW, Lee JW, Sung JK, Ahn SG, et al. Feasibility of transradial coronary intervention using a sheathless guiding catheter in patients with small radial artery. Korean Circ J. 2011; 41:143–8.
Article6. Mamas M, D'Souza S, Hendry C, Ali R, Iles-Smith H, Palmer K, et al. Use of the sheathless guide catheter during routine transradial percutaneous coronary intervention: a feasibility study. Catheter Cardiovasc Interv. 2010; 75:596–602.
Article7. Stella PR, Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. Incidence and outcome of radial artery occlusion following transradial artery coronary angioplasty. Cathet Cardiovasc Diagn. 1997; 40:156–8.
Article8. Dahm JB, Vogelgesang D, Hummel A, Staudt A, Völzke H, Felix SB. A randomized trial of 5 vs. 6 French transradial percutaneous coronary interventions. Catheter Cardiovasc Interv. 2002; 57:172–6.
Article9. Yoo BS, Yoon J, Ko JY, Kim JY, Lee SH, Hwang SO, et al. Anatomical consideration of the radial artery for transradial coronary procedures: arterial diameter, branching anomaly and vessel tortuosity. Int J Cardiol. 2005; 101:421–7.
Article10. Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc Interv. 1999; 46:173–8.
Article11. Yokoyama N, Takeshita S, Ochiai M, Koyama Y, Hoshino S, Isshiki T, et al. Anatomic variations of the radial artery in patients undergoing transradial coronary intervention. Catheter Cardiovasc Interv. 2000; 49:357–62.
Article12. Numasawa Y, Kawamura A, Kohsaka S, Takahashi M, Endo A, Arai T, et al. Anatomical variations affect radial artery spasm and procedural achievement of transradial cardiac catheterization. Heart Vessels. 2014; 29:49–57.
Article13. Lo TS, Nolan J, Fountzopoulos E, Behan M, Butler R, Hetherington SL, et al. Radial artery anomaly and its influence on transradial coronary procedural outcome. Heart. 2009; 95:410–5.
Article14. Valsecchi O, Vassileva A, Musumeci G, Rossini R, Tespili M, Guagliumi G, et al. Failure of transradial approach during coronary interventions: anatomic considerations. Catheter Cardiovasc Interv. 2006; 67:870–8.
Article15. Louvard Y, Lefèvre T. Loops and transradial approach in coronary diagnosis and intervention. Catheter Cardiovasc Interv. 2000; 51:250–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sheathless Transradial Coronary Intervention for Complex Coronary Lesions with a Standard Guiding Catheter
- Feasibility of Transradial Coronary Intervention Using a Sheathless Guiding Catheter in Patients With Small Radial Artery
- Simple Management of Radial Artery Perforation during Transradial Percutaneous Coronary Intervention
- Broken Guidewire Fragment in the Radio-brachial Artery During Transradial Sheath Placement: Percutaneous Retrieval via Femoral Approach
- Feasibility and Problems in Transradial Coronary Angiography and Intervention