Infect Chemother.
2018 Jun;50(2):138-143. 10.3947/ic.2018.50.2.138.
Catheter-Related Trichosporon asahii Bloodstream Infection in a Neutropenic Patient with Myelodysplastic Syndrome
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. mdcjk@catholic.ac.kr
- 3Vaccine Bio Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Catholic Hematology Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2415035
- DOI: http://doi.org/10.3947/ic.2018.50.2.138
Abstract
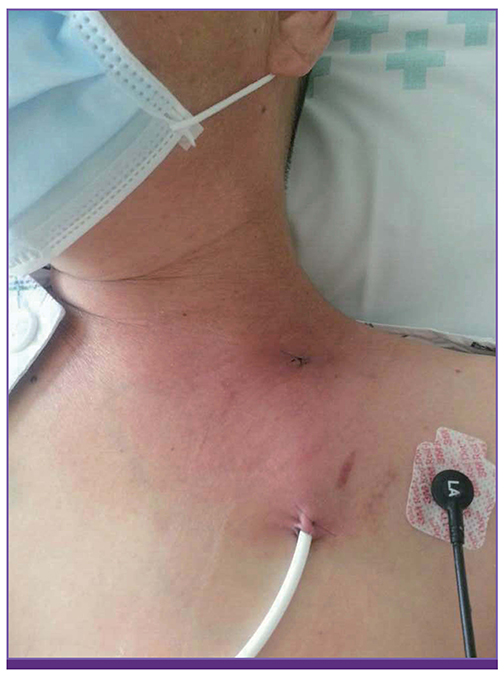
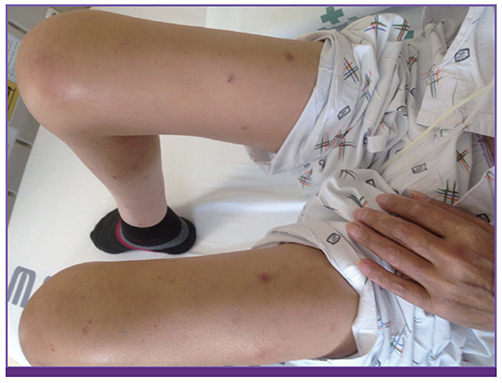
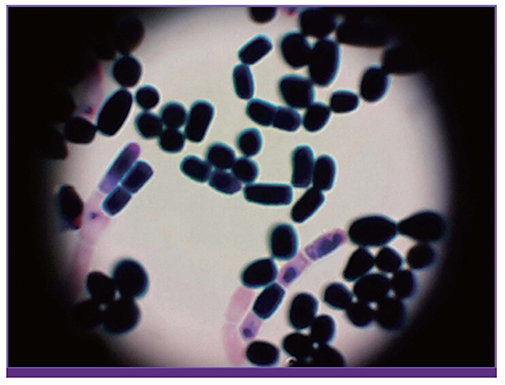
- Because primary antifungal prophylaxis is widely used for immunocompromised hosts, the incidences of unusual fungal infections have increased. Trichosporon asahii has emerged as an important life-threatening opportunistic systemic pathogen because of the increased use of cytotoxic or immunosuppressant agents, along with high mortality rates. Here, we describe a case of catheter-related T. asahii bloodstream infection with multiple septic skin nodules in both the arms and legs of the patient who was in the neutropenic period after allogeneic stem cell transplantation for myelodysplastic syndrome treated with prophylactic ciprofloxacin and itraconazole. We successfully treated her with intravenous voriconazole for more than a month without any complications. Clinicians should consider breakthrough Trichosporon infections when clinical progress in an immunocompromised patient with unexplained infection signs and symptoms does not improve despite proper treatment with antibiotics or various antifungal agents. In addition, voriconazole can be a good treatment choice for achieving better treatment results and prognosis.
Keyword
MeSH Terms
-
Anti-Bacterial Agents
Antifungal Agents
Arm
Catheter-Related Infections
Ciprofloxacin
Fungemia
Humans
Immunocompromised Host
Incidence
Itraconazole
Leg
Mortality
Myelodysplastic Syndromes*
Prognosis
Skin
Stem Cell Transplantation
Trichosporon*
Voriconazole
Anti-Bacterial Agents
Antifungal Agents
Ciprofloxacin
Itraconazole
Voriconazole
Figure
Reference
-
1. Malani AN, Kauffman CA. Changing epidemiology of rare mould infections: implications for therapy. Drugs. 2007; 67:1803–1812.2. Auberger J, Lass-Florl C, Aigner M, Clausen J, Gastl G, Nachbaur D. Invasive fungal breakthrough infections, fungal colonization and emergence of resistant strains in high-risk patients receiving antifungal prophylaxis with posaconazole: real-life data from a single-centre institutional retrospective observational study. J Antimicrob Chemother. 2012; 67:2268–2273.
Article3. Kang SH, Kim HS, Bae MN, Kim J, Yoo JY, Lee KY, Lee DG. Fatal breakthrough mucormycosis in an acute myelogenous leukemia patient while on posaconazole prophylaxis. Infect Chemother. 2015; 47:49–54.
Article4. Bayramoglu G, Sonmez M, Tosun I, Aydin K, Aydin F. Breakthrough Trichosporon asahii fungemia in neutropenic patient with acute leukemia while receiving caspofungin. Infection. 2008; 36:68–70.
Article5. Asada N, Uryu H, Koseki M, Takeuchi M, Komatsu M, Matsue K. Successful treatment of breakthrough Trichosporon asahii fungemia with voriconazole in a patient with acute myeloid leukemia. Clin Infect Dis. 2006; 43:e39–41.6. Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeast; 4th informational supplement, M27-S4. Wayne, PA: CLSI;2012.7. Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011; 24:682–700.
Article8. Arendrup MC, Boekhout T, Akova M, Meis JF, Cornely OA, Lortholary O. European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group. European Confederation of Medical Mycology. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of rare invasive yeast infections. Clin Microbiol Infect. 2014; 20:Suppl 3. 76–98.
Article9. Dua V, Yadav SP, Oberoi J, Sachdeva A. Successful treatment of Trichosporon asahii infection with voriconazole after bone marrow transplant. J Pediatr Hematol Oncol. 2013; 35:237–238.
Article10. Ruan SY, Chien JY, Hsueh PR. Invasive trichosporonosis caused by Trichosporon asahii and other unusual Trichosporon species at a medical center in Taiwan. Clin Infect Dis. 2009; 49:e11–e17.11. Liao Y, Hartmann T, Ao JH, Yang RY. Serum glucuronoxylomannan may be more appropriate for the diagnosis and therapeutic monitoring of Trichosporon fungemia than serum β -D-glucan. Int J Infect Dis. 2012; 16:e638.12. Suzuki K, Nakase K, Kyo T, Kohara T, Sugawara Y, Shibazaki T, Oka K, Tsukada T, Katayama N. Fatal Trichosporon fungemia in patients with hematologic malignancies. Eur J Haematol. 2010; 84:441–447.13. Menezes EA, Marinho JA, Angelo MR, Cunha Mda C, Cunha FA, Vasconcelos Júnior AA. Isolation and antifungal susceptibility testing of Trichosporon asahii in Ceará, Brazil. Rev Inst Med Trop São Paulo. 2012; 54:1–3.
Article14. Nachbaur D, Angelova O, Orth-Höller D, Ditlbacher A, Lackner M, Auberger J, Lass-Flörl C. Primary antifungal prophylaxis with micafungin in patients with haematological malignancies: real-life data from a retrospective single-centre observational study. Eur J Haematol. 2015; 94:258–264.
Article15. Chen J, Chen F, Wang Y, Yang LY, Miao M, Han Y, Wu DP. Use of combination therapy to successfully treat breakthrough Trichosporon asahii infection in an acute leukemia patient receiving voriconazole. Med Mycol Case Rep. 2014; 6:55–57.
Article16. Kim YJ, Kim SI, Kim YR, Park YM, Park YJ, Kang MW. Successful treatment of septic shock with purpura fulminans caused by Trichosporon asahii in an immunocompetent patient. Ann Clin Lab Sci. 2007; 37:366–369.17. Rieger C, Geiger S, Herold T, Nickenig C, Ostermann H. Breakthrough infection of Trichosporon asahii during posaconazole treatment in a patient with acute myeloid leukaemia. Eur J Clin Microbiol Infect Dis. 2007; 26:843–845.
Article18. Jang MJ, Lee YK, Han KC, Hong SG, Kang MS, Oh D, Chong SY. A case of Trichosporon beigelii fungemia treated with mphotericin B and fluconazole in a patient with acute myelogenous leukemia. Korean J Hematol. 2004; 39:109–112.19. Shimono J, Tsutsumi Y, Ohigashi H. Acute renal tubular damage caused by disseminated Trichosporon infection in primary myelofibrosis. Rinsho Ketsueki. 2015; 56:21–24.20. Matsue K, Uryu H, Koseki M, Asada N, Takeuchi M. Breakthrough trichosporonosis in patients with hematologic malignancies receiving micafungin. Clin Infect Dis. 2006; 42:753–757.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Disseminated Trichosporon asahii Infection in an Immunocompromised Patient
- A Case of Trichosporon asahii Fungemia with Urinary Tract Infection as a Primary Focus
- White Piedra of Scalp Hair Caused by Trichosporon asahii
- Peritonitis due to Trichosporon asahii in a continuous ambulatory peritoneal dialysis patient
- Clinical Evalution of the Incidence and Outcome of Patient with Fungemia