Investig Clin Urol.
2018 Jul;59(4):246-251. 10.4111/icu.2018.59.4.246.
Intravesical electrical stimulation treatment for overactive bladder: An observational study
- Affiliations
-
- 1Department of Urology, Loma Linda University Medical Center, Loma Linda, CA, USA. maapierce@llu.edu
- 2Division of Female Pelvic Medicine and Reconstructive Surgery, Department of Gynecology and Obstetrics, Loma Linda University Medical Center, Loma Linda University, Loma Linda, CA, USA.
- 3Department of Public Health, Loma Linda University, Loma Linda, CA, USA.
- KMID: 2414757
- DOI: http://doi.org/10.4111/icu.2018.59.4.246
Abstract
- PURPOSE
Intravesical electrical stimulation treatment (IVES) has been successfully used to treat neurogenic bladder. We report the results of an observational study regarding the use of IVES for women with overactive bladder syndrome (OAB) and/or urgency urinary incontinence (UUI).
MATERIALS AND METHODS
IVES was performed in women with OAB (defined by frequency ≥8/day, nocturia ≥2/night, or ≥3 episodes of UUI on 3-day voiding diary) who failed prior medical therapy. Subjects underwent 4 weeks of treatment with an 8-Fr Detruset™ IVES catheter. Primary outcome was Patient Global Impression of Improvement (PGI-I) at 3 months. Secondary outcomes included Visual Analog Scale (VAS), Short Form OAB Questionnaire (OAB-q SF), Pelvic Floor Distress Inventory (PFDI), Pelvic Floor Impact Questionnaire (PFIQ), reduction in frequency and UUI on voiding diary, and adverse effects. Analysis was done with paired t-tests and Wilcoxon signed rank tests.
RESULTS
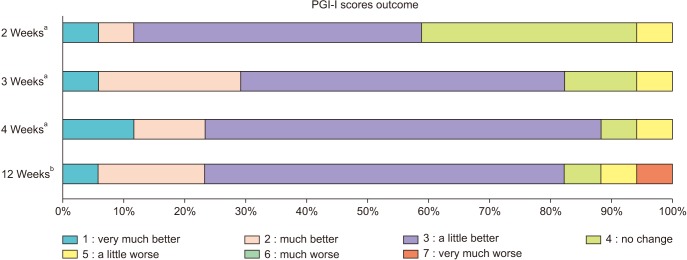
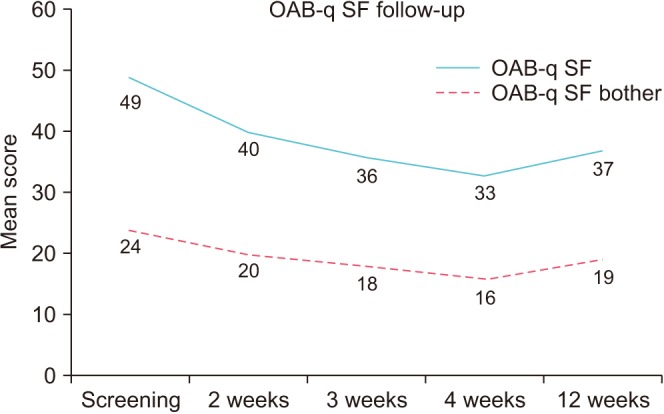
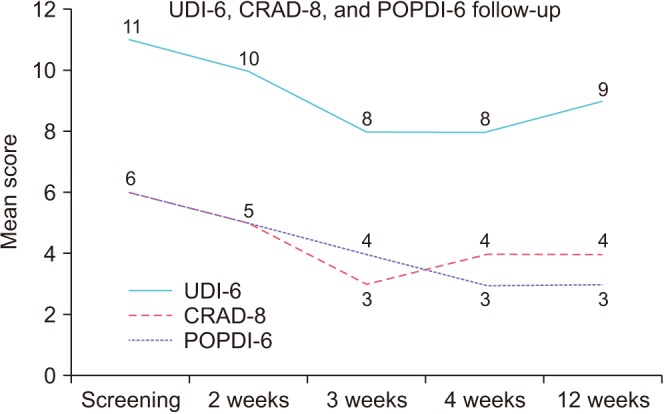
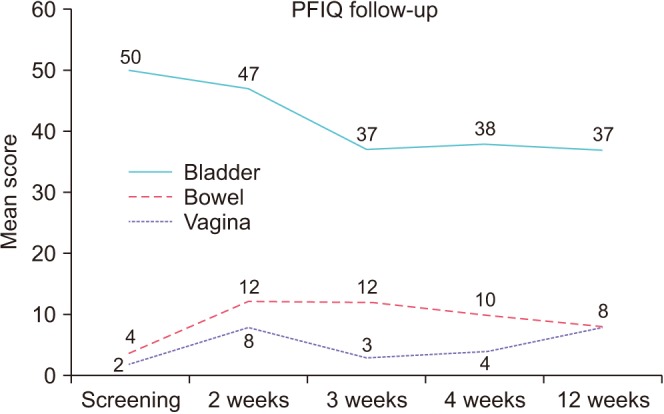
Seventeen subjects completed the study. At 4 weeks post-treatment, 15 improved on PGI-I (11 subjects: "˜a little better', 2: "˜much better', 2: "˜very much better'). There were significant improvements in symptom bother and health-related quality of life as measured by OAB-q SF and pelvic organ prolapse and urinary distress as measured by PFDI. Frequency decreased from 10.3±4.3 at baseline to 8.9±2.3 (p=0.04) at 3 months. No pain was reported during treatment. There was one urinary tract infection during the study period. No other adverse events were reported.
CONCLUSIONS
IVES appears to be a safe and effective novel treatment for OAB. Larger comparative studies are needed to investigate its potential for long-term treatment.
MeSH Terms
Figure
Reference
-
1. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314. PMID: 17049716.
Article2. Gormley EA, Lightner DJ, Faraday M, Vasavada SP. American Urological Association. Society of Urodynamics, Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol. 2015; 193:1572–1580. PMID: 25623739.
Article3. Peters KM, Carrico DJ, Perez-Marrero RA, Khan AU, Wooldridge LS, Davis GL, et al. Randomized trial of percutaneous tibial nerve stimulation versus Sham efficacy in the treatment of overactive bladder syndrome: results from the SUmiT trial. J Urol. 2010; 183:1438–1443. PMID: 20171677.
Article4. Peters KM, Macdiarmid SA, Wooldridge LS, Leong FC, Shobeiri SA, Rovner ES, et al. Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: results from the overactive bladder innovative therapy trial. J Urol. 2009; 182:1055–1061. PMID: 19616802.
Article5. Siegel S, Noblett K, Mangel J, Griebling TL, Sutherland SE, Bird ET, et al. Results of a prospective, randomized, multicenter study evaluating sacral neuromodulation with InterStim therapy compared to standard medical therapy at 6-months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn. 2015; 34:224–230. PMID: 24415559.
Article6. Choi EK, Hong CH, Kim MJ, Im YJ, Jung HJ, Han SW. Effects of intravesical electrical stimulation therapy on urodynamic patterns for children with spina bifida: a 10-year experience. J Pediatr Urol. 2013; 9:798–803. PMID: 23177928.
Article7. Gladh G, Mattsson S, Lindström S. Intravesical electrical stimulation in the treatment of micturition dysfunction in children. Neurourol Urodyn. 2003; 22:233–242. PMID: 12707874.
Article8. Lombardi G, Musco S, Celso M, Ierardi A, Nelli F, Del Corso F, et al. Intravesical electrostimulation versus sacral neuromodulation for incomplete spinal cord patients suffering from neurogenic non-obstructive urinary retention. Spinal Cord. 2013; 51:571–578. PMID: 23628893.
Article9. de Groat WC, Yoshimura N. Changes in afferent activity after spinal cord injury. Neurourol Urodyn. 2010; 29:63–76. PMID: 20025033.
Article10. Hong CH, Kim JH, Noh JY, Gil YC, Lee HY, Lee WH, et al. Sensory neuronal change after intravesical electrical stimulation in spinailized rat. Yonsei Med J. 2002; 43:652–656. PMID: 12402380.
Article11. Gregorini F, Knüpfer SC, Liechti MD, Schubert M, Curt A, Kessler TM, et al. Sensory evoked potentials of the bladder and urethra in middle-aged women: the effect of age. BJU Int. 2015; 115(Suppl 6):18–25. PMID: 25626360.
Article12. Hong CH, Lee HY, Jin MH, Noh JY, Lee BH, Han SW. The effect of intravesical electrical stimulation on bladder function and synaptic neurotransmission in the rat spinal cord after spinal cord injury. BJU Int. 2009; 103:1136–1141. PMID: 19021629.
Article13. Cheng EY, Richards I, Balcom A, Steinhardt G, Diamond M, Rich M, et al. Bladder stimulation therapy improves bladder compliance: results from a multi-institutional trial. J Urol. 1996; 156:761–764. PMID: 8683778.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transcutaneous Electrical Stimulation of the Abdomen, Ear, and Tibial Nerve Modulates Bladder Contraction in a Rat Detrusor Overactivity Model: A Pilot Study
- Electrical Stimulation for Refractory Overactive Bladder
- Effects of Intravesical Instillation of Cyclooxygenase-2 Inhibitor on Cyclophosphamide-induced Overactive Bladder
- Current opinion of the treatment of female voiding dysfunction
- Inhibitory Effect and Possible Mechanism of Intraurethral Stimulation on Overactive Bladder in Female Rats