Ann Surg Treat Res.
2018 Jul;95(1):22-28. 10.4174/astr.2018.95.1.22.
Transduodenal ampullectomy for ampullary tumors - single center experience of consecutive 26 patients
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. mtsong21c@amc.seoul.kr
- KMID: 2414449
- DOI: http://doi.org/10.4174/astr.2018.95.1.22
Abstract
- PURPOSE
Transduodenal ampullectomy (TDA) has been reported in a limited number of cases and in a small number of case series. The aim of this study was to analyze perioperative and long-term oncological outcomes of patients with ampullary tumors who underwent TDA in a single large-volume center.
METHODS
Through a retrospective review of data from 2004 to 2016, we identified 26 patients who underwent TDA at Asan Medical Center.
RESULTS
Eleven of 26 patients underwent TDA for T1 and carcinoma in situ (high-grade dysplasia) cancer; these patients are still alive without recurrence. A major in-hospital complication (3.8%) occurred in 1 case, but there was no case of 90-day mortality. In addition, none of the patients was diagnosed as having newly developed diabetes mellitus after TDA. No significant differences were found between open and laparoscopic-TDA in terms of operation time, painkiller use, and hospital stay.
CONCLUSION
TDA is a feasible and effective surgical procedure for the treatment of selected patients with ampullary tumors. It is an alternative treatment option in cases of ampullary tumors not amenable to endoscopic papillectomy or pancreaticoduodenectomy.
MeSH Terms
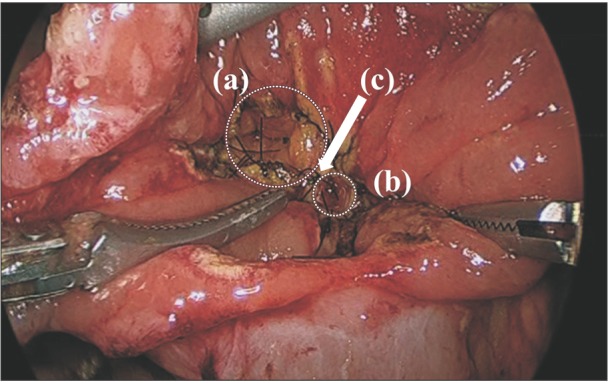
Figure
Cited by 2 articles
-
Retroduodenal resection of the extrahepatic common bile duct with in situ re-implantation of the main pancreatic duct: A report of two cases
Shin Hwang, Dong-Hwan Jung, Tae-Yong Ha
Ann Hepatobiliary Pancreat Surg. 2020;24(3):373-380. doi: 10.14701/ahbps.2020.24.3.373.Robotic transduodenal ampullectomy: Case report and review of the literature
Yun Le Linn, Zhongkai Wang, Brian K. P. Goh
Ann Hepatobiliary Pancreat Surg. 2021;25(1):150-154. doi: 10.14701/ahbps.2021.25.1.150.
Reference
-
1. Takashima M, Ueki T, Nagai E, Yao T, Yamaguchi K, Tanaka M, et al. Carcinoma of the ampulla of Vater associated with or without adenoma: a clinicopathologic analysis of 198 cases with reference to p53 and Ki-67 immunohistochemical expressions. Mod Pathol. 2000; 13:1300–1307. PMID: 11144926.
Article2. Ahmad SR, Adler DG. Cancer of the ampulla of vater: current evaluation and therapy. Hosp Pract (1995). 2014; 42:45–61. PMID: 25485917.
Article3. Ahn DH, Bekaii-Saab T. Ampullary cancer: an overview. Am Soc Clin Oncol Educ Book. 2014; 112–115. PMID: 24857067.
Article4. Hernandez LV, Catalano MF. Endoscopic papillectomy. Curr Opin Gastroenterol. 2008; 24:617–622. PMID: 19122504.
Article5. De Palma GD. Endoscopic papillectomy: indications, techniques, and results. World J Gastroenterol. 2014; 20:1537–1543. PMID: 24587629.6. Kobayashi A, Konishi M, Nakagohri T, Takahashi S, Kinoshita T. Therapeutic approach to tumors of the ampulla of Vater. Am J Surg. 2006; 192:161–164. PMID: 16860623.
Article7. Dixon E, Vollmer CM Jr, Sahajpal A, Cattral MS, Grant DR, Taylor BR, et al. Transduodenal resection of periampullary lesions. World J Surg. 2005; 29:649–652. PMID: 15827855.
Article8. Mathur A, Paul H, Ross S, Luberice K, Hernandez J, Vice M, et al. Transduodenal ampullectomy for ampullary adenomas: a safe and effective procedure with long-term salutary outcomes. Am Surg. 2014; 80:185–190. PMID: 24480221.
Article9. Song J, Liu H, Li Z, Yang C, Sun Y, Wang C. Long-term prognosis of surgical treatment for early ampullary cancers and implications for local ampullectomy. BMC Surg. 2015; 15:32. PMID: 25888004.
Article10. Sauvanet A, Dokmak S, Cros J, Cazals-Hatem D, Ponsot P, Palazzo M. Surgical ampullectomy with complete resection of the common bile duct: a new procedure for radical resection of non-invasive ampulloma with biliary extension. J Gastrointest Surg. 2017; 21:1533–1539. PMID: 28560704.
Article11. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.12. Woo SM, Ryu JK, Lee SH, Lee WJ, Hwang JH, Yoo JW, et al. Feasibility of endoscopic papillectomy in early stage ampulla of Vater cancer. J Gastroenterol Hepatol. 2009; 24:120–124. PMID: 19032444.
Article13. Ceppa EP, Burbridge RA, Rialon KL, Omotosho PA, Emick D, Jowell PS, et al. Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. Ann Surg. 2013; 257:315–322. PMID: 23059497.14. Kim J, Choi SH, Choi DW, Heo JS, Jang KT. Role of transduodenal ampullectomy for tumors of the ampulla of Vater. J Korean Surg Soc. 2011; 81:250–256. PMID: 22111080.
Article15. Mansukhani VM, Desai GS, Mouli S, Shirodkar K, Shah RC, Palepu J. Transduodenal ampul lectomy for ampullary tumors. Indian J Gastroenterol. 2017; 36:62–65. PMID: 28054258.16. Panzeri F, Crippa S, Castelli P, Aleotti F, Pucci A, Partelli S, et al. Management of ampullary neoplasms: a tailored approach between endoscopy and surgery. World J Gastroenterol. 2015; 21:7970–7987. PMID: 26185369.
Article17. Meneghetti AT, Safadi B, Stewart L, Way LW. Local resection of ampullary tumors. J Gastrointest Surg. 2005; 9:1300–1306. PMID: 16332486.
Article18. Roggin KK, Yeh JJ, Ferrone CR, Riedel E, Gerdes H, Klimstra DS, et al. Limitations of ampullectomy in the treatment of nonfamilial ampullary neoplasms. Ann Surg Oncol. 2005; 12:971–980. PMID: 16244798.
Article19. Lee H, Park JY, Kwon W, Heo JS, Choi DW, Choi SH. Transduodenal ampullectomy for the treatment of early-stage ampulla of vater cancer. World J Surg. 2016; 40:967–973. PMID: 26546182.
Article20. Gao Y, Zhu Y, Huang X, Wang H, Huang X, Yuan Z. Transduodenal ampullectomy provides a less invasive technique to cure early ampullary cancer. BMC Surg. 2016; 16:36. PMID: 27251044.
Article21. Kwon JH, Kim SC, Shim IK, Song KB, Lee JH, Hwang DW, et al. Factors affecting the development of diabetes mellitus after pancreatic resection. Pancreas. 2015; 44:1296–1303. PMID: 26390413.
Article22. Falconi M, Mantovani W, Crippa S, Mascetta G, Salvia R, Pederzoli P. Pancreatic insufficiency after different resections for benign tumours. Br J Surg. 2008; 95:85–91. PMID: 18041022.
Article23. Huang JJ, Yeo CJ, Sohn TA, Lillemoe KD, Sauter PK, Coleman J, et al. Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg. 2000; 231:890–898. PMID: 10816633.
Article24. Brown GC, Brown MM, Sharma S, Brown H, Gozum M, Denton P. Quality of life associated with diabetes mellitus in an adult population. J Diabetes Complications. 2000; 14:18–24. PMID: 10925062.
Article25. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727. PMID: 18948798.26. Velanovich V. Laparoscopic vs open surgery: a preliminary comparison of quality-of-life outcomes. Surg Endosc. 2000; 14:16–21. PMID: 10653229.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic transduodenal ampullectomy: Case report and review of the literature
- Role of transduodenal ampullectomy for tumors of the ampulla of Vater
- Hand Assisted Laparoscopic Transduodenal Ampullary Mass Excision
- Transduodenal Ampullectomy in Ampullary Neoplasm
- Endoscopic Ampullectomy for Tumors of the Ampulla of Vater: Long-term Follow-up Results