J Endocr Surg.
2018 Mar;18(1):37-48. 10.16956/jes.2018.18.1.37.
Standards for Intraoperative Neuromonitoring in Thyroid Operations
- Affiliations
-
- 1KUMC Thyroid Center, Korea University Anam Hospital, Seoul, Korea.
- 2Division of Thyroid Surgery, Jilin Provincial Key Laboratory of Surgical Translational Medicine, China Japan Union Hospital of Jilin University, Changchun, China.
- 3Department of Surgery, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 4Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
- 5Department of General, Visceral, and Transplantation Surgery, University Hospital Essen, Essen, Germany.
- 6Division of Endocrine Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital Policlinico G. Martino, University of Messina, Italy. gianlorenzo.dionigi@gmail.com
- KMID: 2414421
- DOI: http://doi.org/10.16956/jes.2018.18.1.37
Abstract
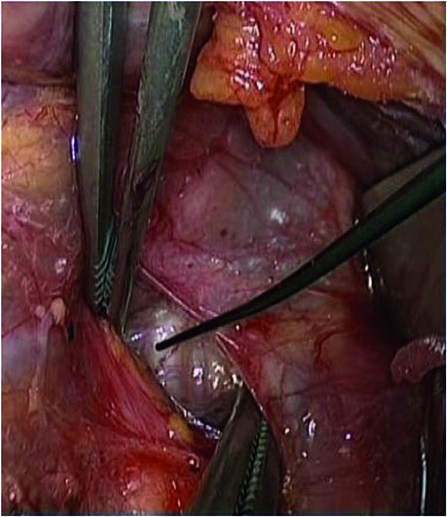
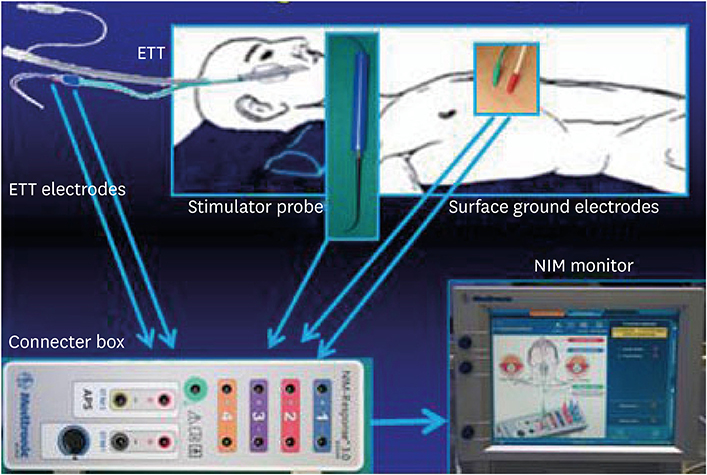
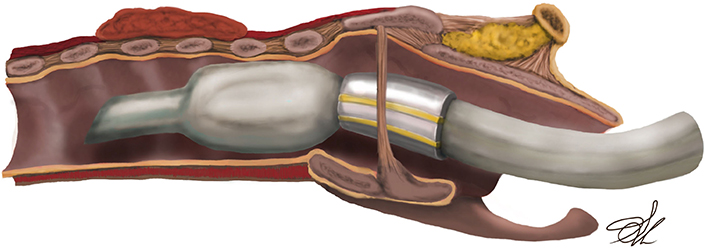
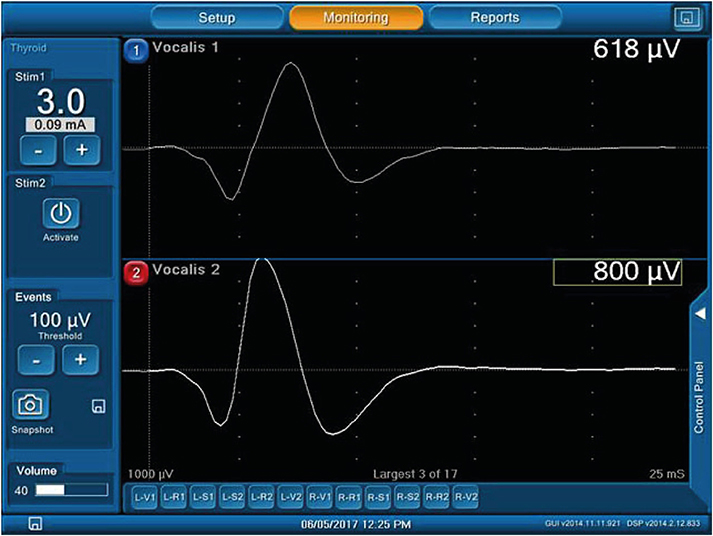
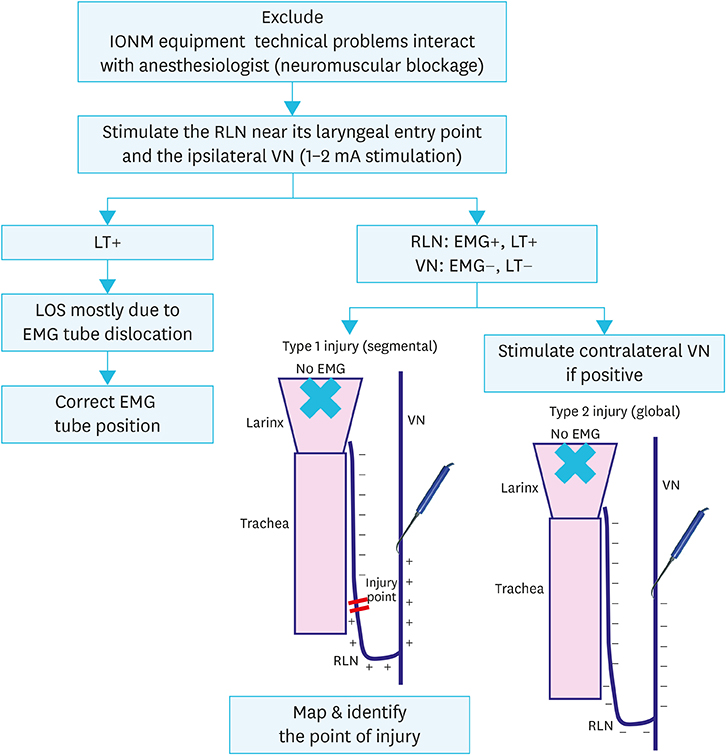
- After the introduction of intraoperative neural monitoring (IONM) of the recurrent laryngeal nerve (RLN) in clinical thyroid practice almost 16 years ago, the procedure has expanded rapidly with an area-wide spread in Asia, Europe, and USA. While the visual nerve presentation with the eye or the magnifying glass technique is capable of assessing the anatomical continuity of the RLN, IONM additionally allows a functional analysis that has a high correlation, i.e., prediction of postoperative vocal motility. Although the predictive value of the IONM is much higher (>97%) in the case of an intact signal than in the case of a signal failure (40%-70%), the prediction is also unequally higher than the visual-anatomical assessment of the nerve. Thus, IONM can be used as a basis for an intraoperative decision-making of a 1-side or 2-side procedure to avoid bilateral RLN palsy in a bilateral procedure. A precondition for the safe application of IONM is the perfect knowledge of the technology and technique, the routine execution of preoperative and postoperative laryngoscopy, the strict standardization of the neurostimulation (electromyography documentation of the vagal nerve stimulation before and after resection), and an adequate management of technically or operationally caused incidents (i.e., systematic application of troubleshooting algorithms). The following review provides a synopsis of the experiences of the Korean Intraoperative Neural Monitoring Society (KINMoS) for the correct use of IONM.
MeSH Terms
Figure
Reference
-
1. Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004; 136:1310–1322.
Article2. Hermann M, Alk G, Roka R, Glaser K, Freissmuth M. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg. 2002; 235:261–268.
Article3. Cho I, Jo MG, Choi SW, Jang JY, Wang SG, Cha W. Some posterior branches of extralaryngeal recurrent laryngeal nerves have motor fibers. Laryngoscope. Forthcoming. 2017.
Article4. Baek SK, Lee K, Oh D, Kang SH, Kwon SY, Woo JS, et al. Efficiency of intraoperative neuromonitoring on voice outcomes after thyroid surgery. Auris Nasus Larynx. 2017; 44:583–589.
Article5. Cha W, Cho I, Jang JY, Cho JK, Wang SG, Park JH. Supramaximal neurostimulation with laryngeal palpation to predict postoperative vocal fold mobility. Laryngoscope. 2016; 126:2863–2868.
Article6. Wu CW, Hao M, Tian M, Dionigi G, Tufano RP, Kim HY, et al. Recurrent laryngeal nerve injury with incomplete loss of electromyography signal during monitored thyroidectomy-evaluation and outcome. Langenbecks Arch Surg. 2017; 402:691–699.
Article7. Lee MS, Lee UY, Lee JH, Han SH. Relative direction and position of recurrent laryngeal nerve for anatomical configuration. Surg Radiol Anat. 2009; 31:649–655.
Article8. Roh JL, Yoon YH, Park CI. Recurrent laryngeal nerve paralysis in patients with papillary thyroid carcinomas: evaluation and management of resulting vocal dysfunction. Am J Surg. 2009; 197:459–465.
Article9. Yun JS, Lee YS, Jung JJ, Nam KH, Chung WY, Chang HS, et al. The Zuckerkandl’s tubercle: a useful anatomical landmark for detecting both the recurrent laryngeal nerve and the superior parathyroid during thyroid surgery. Endocr J. 2008; 55:925–930.
Article10. Hong KH, Kim YK. Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg. 1997; 117:399–404.
Article11. Lamadé W, Renz K, Willeke F, Klar E, Herfarth C. Effect of training on the incidence of nerve damage in thyroid surgery. Br J Surg. 1999; 86:388–391.
Article12. Randolph GW, Kobler JB, Wilkins J. Recurrent laryngeal nerve identification and assessment during thyroid surgery: laryngeal palpation. World J Surg. 2004; 28:755–760.
Article13. Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998; 228:320–330.
Article14. Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009; 96:240–246.
Article15. Dralle H, Lorenz K. Intraoperative neuromonitoring of thyroid gland operations: surgical standards and aspects of expert assessment. Chirurg. 2010; 81:612–619.16. Schneider R, Randolph GW, Barczynski M, Dionigi G, Wu CW, Chiang FY, et al. Continuous intraoperative neural monitoring of the recurrent nerves in thyroid surgery: a quantum leap in technology. Gland Surg. 2016; 5:607–616.
Article17. Schneider R, Sekulla C, Machens A, Lorenz K, Thanh PN, Dralle H. Dynamics of loss and recovery of the nerve monitoring signal during thyroidectomy predict early postoperative vocal fold function. Head Neck. 2016; 38:Suppl 1. 37144–51.
Article18. Phelan E, Schneider R, Lorenz K, Dralle H, Kamani D, Potenza A, et al. Continuous vagal IONM prevents recurrent laryngeal nerve paralysis by revealing initial EMG changes of impending neuropraxic injury: a prospective, multicenter study. Laryngoscope. 2014; 124:1498–1505.
Article19. Schneider R, Bures C, Lorenz K, Dralle H, Freissmuth M, Hermann M. Evolution of nerve injury with unexpected EMG signal recovery in thyroid surgery using continuous intraoperative neuromonitoring. World J Surg. 2013; 37:364–368.
Article20. Schneider R, Randolph GW, Sekulla C, Phelan E, Thanh PN, Bucher M, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck. 2013; 35:1591–1598.
Article21. Schneider R, Sekulla C, Machens A, Lorenz K, Nguyen Thanh P, Dralle H. Postoperative vocal fold palsy in patients undergoing thyroid surgery with continuous or intermittent nerve monitoring. Br J Surg. 2015; 102:1380–1387.
Article22. Dralle H, Sekulla C, Lorenz K, Nguyen Thanh P, Schneider R, Machens A. Loss of the nerve monitoring signal during bilateral thyroid surgery. Br J Surg. 2012; 99:1089–1095.
Article23. Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004; 389:499–503.
Article24. Randolph GW, Dralle H; International Intraoperative Monitoring Study Group. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; 121:Suppl 1. S1–16.
Article25. Marusch F, Hussock J, Haring G, Hachenberg T, Gastinger I. Influence of muscle relaxation on neuromonitoring of the recurrent laryngeal nerve during thyroid surgery. Br J Anaesth. 2005; 94:596–600.
Article26. Melin M, Schwarz K, Lammers BJ, Goretzki PE. IONM-guided goiter surgery leading to two-stage thyroidectomy--indication and results. Langenbecks Arch Surg. 2013; 398:411–418.
Article27. Périé S, Aït-Mansour A, Devos M, Sonji G, Baujat B, St Guily JL. Value of recurrent laryngeal nerve monitoring in the operative strategy during total thyroidectomy and parathyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis. 2013; 130:131–136.
Article28. Dionigi G, Frattini F. Staged thyroidectomy: time to consider intraoperative neuromonitoring as standard of care. Thyroid. 2013; 23:906–908.
Article29. Fontenot TE, Randolph GW, Setton TE, Alsaleh N, Kandil E. Does intraoperative nerve monitoring reliably aid in staging of total thyroidectomies? Laryngoscope. 2015; 125:2232–2235.
Article30. Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A; German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008; 32:1358–1366.
Article31. Casella C, Pata G, Nascimbeni R, Mittempergher F, Salerni B. Does extralaryngeal branching have an impact on the rate of postoperative transient or permanent recurrent laryngeal nerve palsy? World J Surg. 2009; 33:261–265.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Neuromonitoring during Thyroid Surgery
- The Present and Future of Intraoperative Neuromonitoring in Thyroid Surgery
- Efficiency of Intraoperative Recurrent Laryngeal Nerve Monitoring Using Electromyography Tube in Reoperative Thyroid Surgery
- The effect of intraoperative neuromonitoring on the number of lymph nodes excised and recurrence when applied during neck dissection in cases of papillary thyroid cancer
- Effectiveness of Intraoperative Neuromonitoring According to the Mechanism of Recurrent Laryngeal Nerve Injury During Thyroid Surgery