Blood Res.
2018 Mar;53(1):25-34. 10.5045/br.2018.53.1.25.
Improvement of treatment outcome over 2 decades in children with acute myeloid leukemia
- Affiliations
-
- 1Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea. hoonkook@chonnam.ac.kr
- 2Environmental Health Center for Childhood Leukemia and Cancer, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- KMID: 2414361
- DOI: http://doi.org/10.5045/br.2018.53.1.25
Abstract
- BACKGROUND
The prognosis of pediatric acute myeloid leukemia (AML) has recently improved. This study aimed to describe the epidemiology, changes in treatment strategies, and improvement of outcomes in Gwangju-Chonnam children with AML over 2 decades.
METHODS
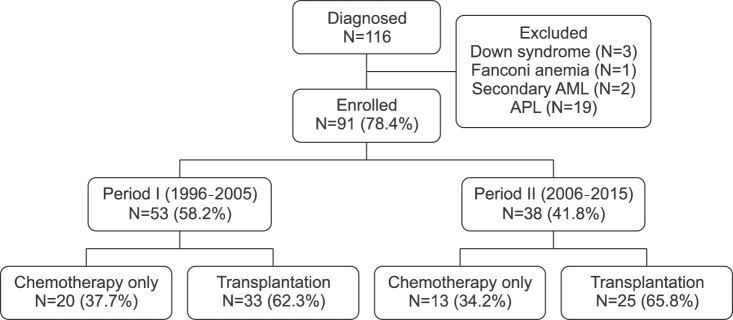
Medical records of 116 children with newly diagnosed AML were retrospectively reviewed for demographic characteristics, prognostic groups including cytogenetic risks, treatment protocols, and survival rates over the periods between 1996 and 2005 (Period I, N=53), and 2006 and 2015 (Period II, N=38).
RESULTS
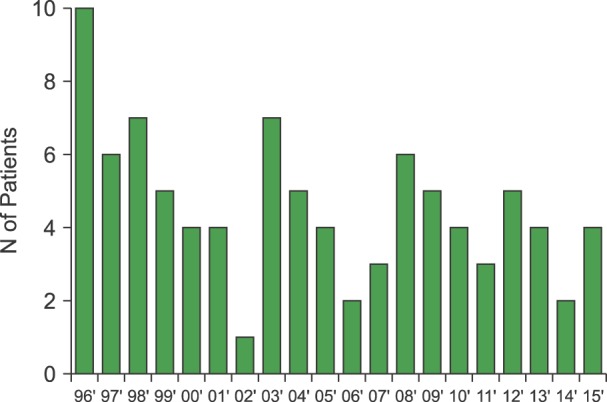
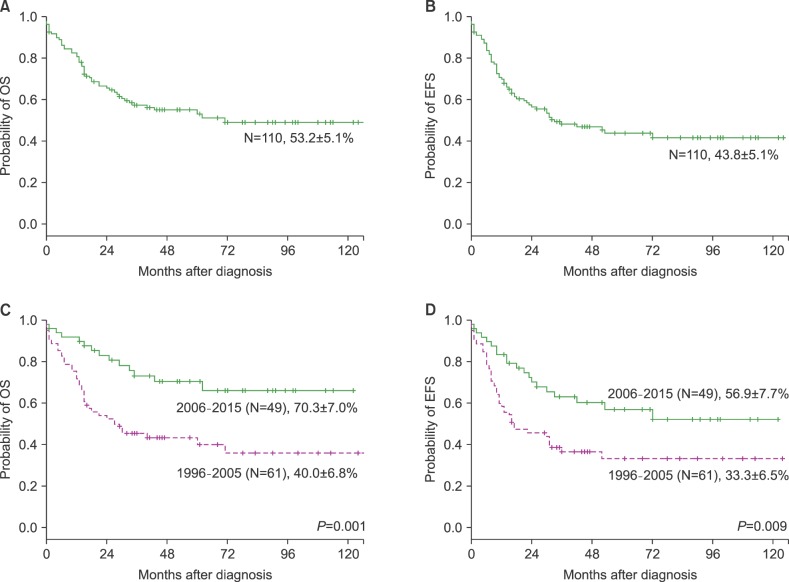
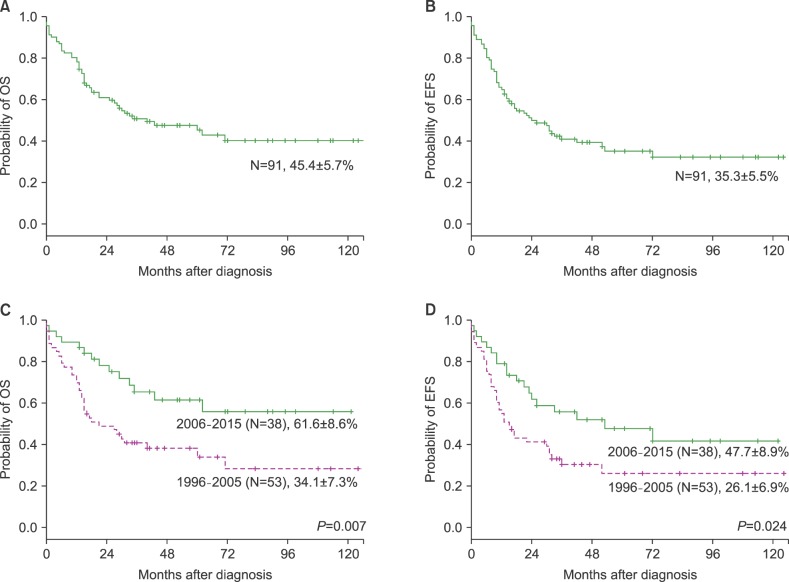
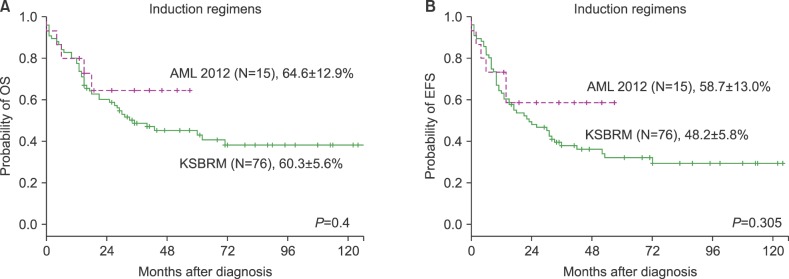
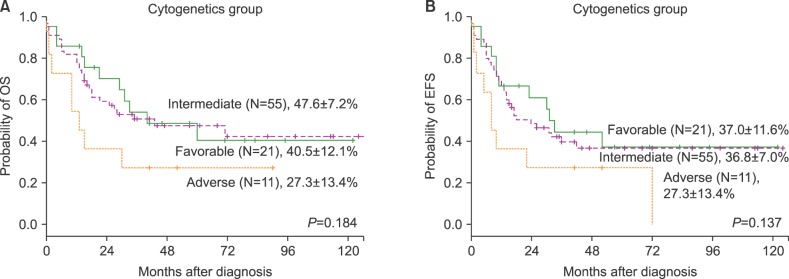
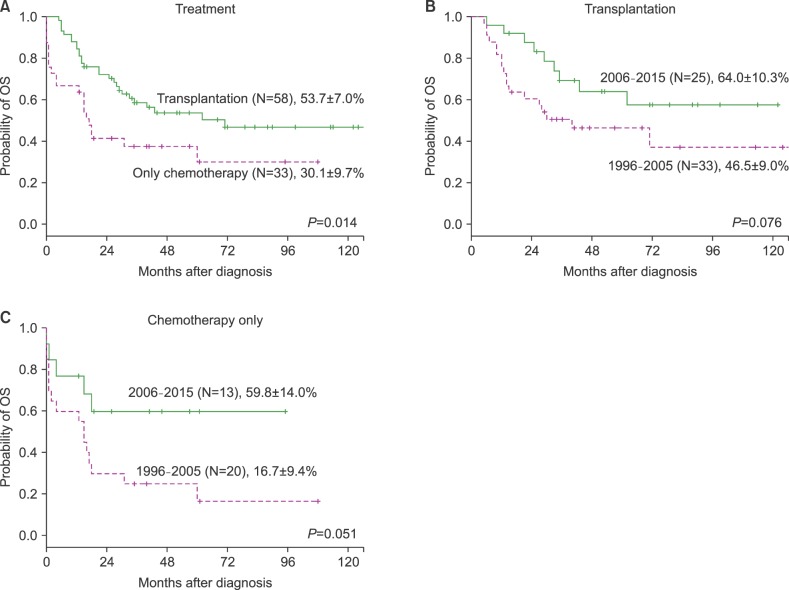
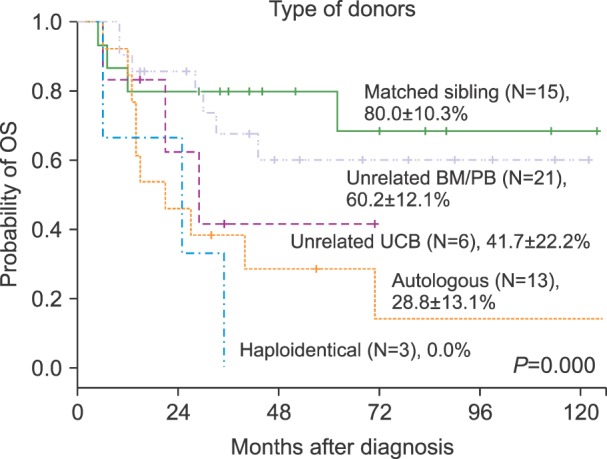
The annual incidence of AML has decreased with reduced pediatric population. The 5-year Kaplan-Meier (K-M) estimated overall survival (OS) and event-free survival (EFS) rates in 110 AML patients were 53.2±5.1% and 43.8±5.1%, respectively. The 5-year OS rate significantly improved during period II (70.3±7.0%) as compared to that during period I (40.0±6.8%) (P =0.001). The 5-year OS was not significantly different among cytogenetic risk groups (P =0.11). Fifty-eight patients underwent hematopoietic stem cell transplantation (HSCT). The K-M 5-year estimated survival for transplanted patients was 53.7±7.0%, while that for chemotherapy-only patients was 30.1±9.1% (P =0.014). Among the prognostic factors, treatment modality was the only independent factor. The chemotherapy-only group had a relative risk of 2.06 for death compared with the transplantation group (P=0.015).
CONCLUSION
The survival of Korean children with AML has improved to a level comparable with that of developed countries over 2 decades, owing to a change in induction strategy, better supportive care with economic growth, refinement of HSCT techniques including a better selection of patients based on prognostic groups, and stem cell donor selection.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
국내 혈액암 질환의 증가 양상: 2005년부터 2015년까지 국민건강보험 빅데이터에 근거하여
Yujin Han, Young Jin Kim, Min Jin Kim, Ja Min Byun, Taemi Youk, Hoi Soo Yoon, Jae Hee Lee, Woo-In Lee, Tae Sung Park, Jongha Yoo
Lab Med Online. 2020;10(2):144-151. doi: 10.3343/lmo.2020.10.2.144.Outcomes of pediatric acute myeloid leukemia patients with FLT3-ITD mutations in the pre-FLT3 inhibitor era
Sujin Choi, Bo Kyung Kim, Hong Yul Ahn, Kyung Taek Hong, Jung Yoon Choi, Hee Young Shin, Hyoung Jin Kang
Blood Res. 2020;55(4):217-224. doi: 10.5045/br.2020.2020127.Current treatment for pediatric acute myeloid leukemia
Ho Joon Im
Blood Res. 2018;53(1):1-2. doi: 10.5045/br.2018.53.1.1.
Reference
-
1. Gamis AS, Alonzo TA, Perentesis JP, Meshinchi S. COG Acute Myeloid Leukemia Committee. Children's Oncology Group's 2013 blueprint for research: acute myeloid leukemia. Pediatr Blood Cancer. 2013; 60:964–971. PMID: 23255301.
Article2. Horibe K, Saito AM, Takimoto T, et al. Incidence and survival rates of hematological malignancies in Japanese children and adolescents (2006-2010): based on registry data from the Japanese Society of Pediatric Hematology. Int J Hematol. 2013; 98:74–88. PMID: 23702913.
Article3. Park HJ, Moon EK, Yoon JY, et al. Incidence and survival of childhood cancer in Korea. Cancer Res Treat. 2016; 48:869–882. PMID: 26790965.
Article4. Kömür M, Erbey F, Bayram I, Tanyeli A. Incidence and prognostic importance of molecular genetic defects in children with acute myeloblastic leukemia. Asian Pac J Cancer Prev. 2010; 11:1393–1395. PMID: 21198299.5. Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998; 92:2322–2333. PMID: 9746770.6. Kim G, Lee HO, Choi JS, Baek HJ, Kook H. Characteristics and therapeutic outcomes of acute promyelocytic leukemia in children and adolescents. Clin Pediatr Hematol Oncol. 2016; 23:105–115.
Article7. ter Bals E, Kaspers GJ. Treatment of childhood acute myeloid leukemia. Expert Rev Anticancer Ther. 2005; 5:917–929. PMID: 16221060.
Article8. Gupta V. Alternative donor transplants for high-risk acute myeloid leukemia. Curr Opin Hematol. 2008; 15:115–120. PMID: 18300757.
Article9. Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014; 64:83–103. PMID: 24488779.
Article10. Dama E, Pastore G, Mosso ML, et al. Time trends and prognostic factors for survival from childhood cancer: a report from the Childhood Cancer Registry of Piedmont (Italy). Eur J Pediatr. 2006; 165:240–249. PMID: 16411094.
Article11. Kang KS, Park JH, Lee JT, Lee KB. Survival rates of acute leukemia patients by FAB classification. Korean J Hematol. 1992; 27:239–247.12. Lee DH, Chung NG, Cho B, et al. Idarubicin plus behenoyl cytarabine and 6-thioguanine compares favorably with idarubicin plus cytarabine-based regimen for children with previously untreated acute myeloid leukemia: 10-year retrospective, multicenter study in Korea. J Korean Med Sci. 2010; 25:9–15. PMID: 20052341.
Article13. Korean Statistical Information Service. The population census by age in Gwangju and Chonnam province of Korea (1996-2015). Daejeon, Korea: Korean Statistical Information Service;2015. Accessed February 2, 2016. at http://kosis.kr/eng/statisticsList/statisticsList_01List.jsp?vwcd=MT_ETITLE&parentId=A#SubCont.14. Bennett JM, Catovsky D, Daniel MT, et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985; 103:620–625. PMID: 3862359.15. O'Donnell MR, Abboud CN, Altman J, et al. NCCN Clinical Practice Guidelines acute myeloid leukemia. J Natl Compr Canc Netw. 2012; 10:984–1021. PMID: 22878824.16. Burnett AK, Wheatley K, Goldstone AH, et al. The value of allogeneic bone marrow transplant in patients with acute myeloid leukaemia at differing risk of relapse: results of the UK MRC AML 10 trial. Br J Haematol. 2002; 118:385–400. PMID: 12139722.
Article17. Economic Statistics System. Annual gross national income per capita (1996-2015). Seoul, Korea: the Bank of Korea;2015. Accessed December 31, 2016. at http://ecos.bok.or.kr/jsp/vis/keystat/#/detail.18. Park EH, Lee H, Won YJ, et al. Nationwide statistical analysis of myeloid malignancies in Korea: incidence and survival rate from 1999 to 2012. Blood Res. 2015; 50:204–217. PMID: 26770948.
Article19. Hjalgrim LL, Rostgaard K, Schmiegelow K, et al. Age- and sex-specific incidence of childhood leukemia by immunophenotype in the Nordic countries. J Natl Cancer Inst. 2003; 95:1539–1544. PMID: 14559876.
Article20. Viana MB, Cunha KC, Ramos G, Murao M. Acute myeloid leukemia in childhood: 15-year experience in a single institution. J Pediatr (Rio J). 2003; 79:489–496. PMID: 14685445.21. Imamura T, Iwamoto S, Kanai R, et al. Outcome in 146 patients with paediatric acute myeloid leukaemia treated according to the AML99 protocol in the period 2003-06 from the Japan Association of Childhood Leukaemia Study. Br J Haematol. 2012; 159:204–210. PMID: 22924344.
Article22. Creutzig U, Zimmermann M, Ritter J, et al. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005; 19:2030–2042. PMID: 16304570.
Article23. Klein K, Kaspers G, Harrison CJ, et al. Clinical impact of additional cytogenetic aberrations, cKIT and ras mutations, and treatment elements in pediatric t(8;21)-AML: results from an International Retrospective Study by the International Berlin-Frankfurt-Münster Study Group. J Clin Oncol. 2015; 33:4247–4258. PMID: 26573082.
Article24. Park HS, Kim DW, Kim CC, et al. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen--a prospective, cooperative multicenter study. Semin Hematol. 1996; 33(4 Suppl 3):24–29.25. Woods WG, Neudorf S, Gold S, et al. A comparison of allogeneic bone marrow transplantation, autologous bone marrow transplantation, and aggressive chemotherapy in children with acute myeloid leukemia in remission. Blood. 2001; 97:56–62. PMID: 11133742.26. Gupta V, Tallman MS, He W, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010; 116:1839–1848. PMID: 20538804.
Article27. Zheng C, Zhu X, Tang B, et al. Comparative analysis of unrelated cord blood transplantation and HLA-matched sibling hematopoietic stem cell transplantation in children with high-risk or advanced acute leukemia. Ann Hematol. 2015; 94:473–480. PMID: 25217231.
Article28. Xu XJ, Tang YM, Song H, Yang SL, Shi SW, Wei J. Long-term outcome of childhood acute myeloid leukemia in a developing country: experience from a children's hospital in China. Leuk Lymphoma. 2010; 51:2262–2269. PMID: 20929322.
Article29. Wiangnon S, Veerakul G, Nuchprayoon I, et al. Childhood cancer incidence and survival 2003-2005, Thailand: study from the Thai Pediatric Oncology Group. Asian Pac J Cancer Prev. 2011; 12:2215–2220. PMID: 22296359.30. Chow EJ, Puumala SE, Mueller BA, et al. Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer. 2010; 116:3045–3053. PMID: 20564410.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatments for children and adolescents with AML
- Current treatment for pediatric acute myeloid leukemia
- Acute Myeloid Leukemia after Chemotherapy for Osteosarcoma: A Case Report
- Acute Myeloid Leukemia with Intracardiac Thrombus Presenting as Acute Limb Ischemia
- Recent advances in the treatment of pediatric acute leukemia