Is It Better to Enter a Volume CT Dose Index Value before or after Scan Range Adjustment for Radiation Dose Optimization of Pediatric Cardiothoracic CT with Tube Current Modulation?
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. ghw68@hanmail.net
- KMID: 2413698
- DOI: http://doi.org/10.3348/kjr.2018.19.4.692
Abstract
OBJECTIVE
To determine whether the body size-adapted volume computed tomography (CT) dose index (CTD(vol)) in pediatric cardiothoracic CT with tube current modulation is better to be entered before or after scan range adjustment for radiation dose optimization.
MATERIALS AND METHODS
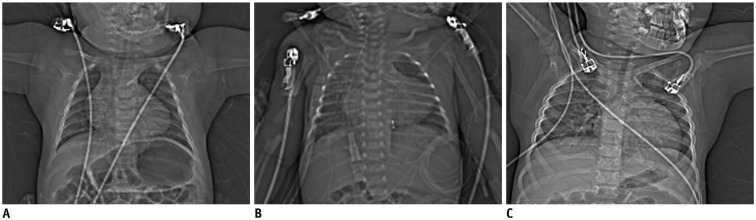
In 83 patients, cardiothoracic CT with tube current modulation was performed with the body size-adapted CTDIvol entered after (group 1, n = 42) or before (group 2, n = 41) scan range adjustment. Patient-related, radiation dose, and image quality parameters were compared and correlated between the two groups.
RESULTS
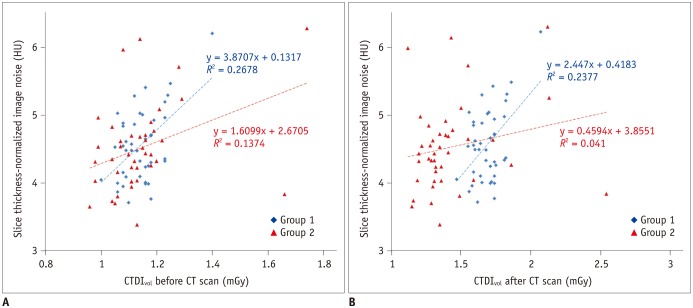
The CTDIvol after the CT scan in group 1 was significantly higher than that in group 2 (1.7 ± 0.1 mGy vs. 1.4 ± 0.3 mGy; p < 0.0001). Image noise (4.6 ± 0.5 Hounsfield units [HU] vs. 4.5 ± 0.7 HU) and image quality (1.5 ± 0.6 vs. 1.5 ± 0.6) showed no significant differences between the two (p > 0.05). In both groups, all patient-related parameters, except body density, showed positive correlations (r = 0.49-0.94; p < 0.01) with the CTDIvol before and after the CT scan. The CTDIvol after CT scan showed modest positive correlation (r = 0.49; p ≤ 0.001) with image noise in group 1 but no significant correlation (p > 0.05) in group 2.
CONCLUSION
In pediatric cardiothoracic CT with tube current modulation, the CTDIvol entered before scan range adjustment provides a significant dose reduction (18%) with comparable image quality compared with that entered after scan range adjustment.
Keyword
Figure
Cited by 5 articles
-
Semiautomatic Three-Dimensional Threshold-Based Cardiac Computed Tomography Ventricular Volumetry in Repaired Tetralogy of Fallot: Comparison with Cardiac Magnetic Resonance Imaging
Hyun Woo Goo
Korean J Radiol. 2019;20(1):102-113. doi: 10.3348/kjr.2018.0237.Computed Tomography Pulmonary Vascular Volume Ratio Can Be Used to Evaluate the Effectiveness of Pulmonary Angioplasty in Peripheral Pulmonary Artery Stenosis
Hyun Woo Goo
Korean J Radiol. 2019;20(10):1422-1430. doi: 10.3348/kjr.2019.0286.User-Friendly Vendor-Specific Guideline for Pediatric Cardiothoracic Computed Tomography Provided by the Asian Society of Cardiovascular Imaging Congenital Heart Disease Study Group: Part 1. Imaging Techniques
Sun Hwa Hong, Hyun Woo Goo, Eriko Maeda, Ki Seok Choo, I-Chen Tsai,
Korean J Radiol. 2019;20(2):190-204. doi: 10.3348/kjr.2018.0571.Changes in Right Ventricular Volume, Volume Load, and Function Measured with Cardiac Computed Tomography over the Entire Time Course of Tetralogy of Fallot
Hyun Woo Goo
Korean J Radiol. 2019;20(6):956-966. doi: 10.3348/kjr.2018.0891.Quantification of Initial Right Ventricular Dimensions by Computed Tomography in Infants with Congenital Heart Disease and a Hypoplastic Right Ventricle
Hyun Woo Goo
Korean J Radiol. 2020;21(2):203-209. doi: 10.3348/kjr.2019.0662.
Reference
-
1. Greenwood TJ, Lopez-Costa RI, Rhoades PD, Ramírez-Giraldo JC, Starr M, Street M, et al. CT dose optimization in pediatric radiology: a multiyear effort to preserve the benefits of imaging while reducing the risks. Radiographics. 2015; 35:1539–1554. PMID: 26267677.
Article2. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012; 13:1–11. PMID: 22247630.
Article3. Goo HW. State-of-the-art CT imaging techniques for congenital heart disease. Korean J Radiol. 2010; 11:4–18. PMID: 20046490.
Article4. Greess H, Lutze J, Nömayr A, Wolf H, Hothorn T, Kalender WA, et al. Dose reduction in subsecond multislice spiral CT examination of children by online tube current modulation. Eur Radiol. 2004; 14:995–999. PMID: 15052502.
Article5. Goo HW, Suh DS. Tube current reduction in pediatric non-ECG-gated heart CT by combined tube current modulation. Pediatr Radiol. 2006; 36:344–351. PMID: 16501970.
Article6. Cody DD. Management of auto exposure control during pediatric computed tomography. Pediatr Radiol. 2014; 44(Suppl 3):427–430. PMID: 25304700.
Article7. Söderberg M. Overview, practical tips and potential pitfalls of using automatic exposure control in CT: Siemens CARE Dose 4D. Radiat Prot Dosimetry. 2016; 169:84–91. PMID: 26567324.
Article8. Solomon JB, Li X, Samei E. Relating noise to image quality indicators in CT examinations with tube current modulation. AJR Am J Roentgenol. 2013; 200:592–600. PMID: 23436849.
Article9. Jung YY, Goo HW. The optimal parameter for radiation dose in pediatric low dose abdominal CT: cross-sectional dimensions versus body weight. J Korean Radiol Soc. 2008; 58:169–175.
Article10. Dong F, Davros W, Pozzuto J, Reid J. Optimization of kilovoltage and tube current-exposure time product based on abdominal circumference: an oval phantom study for pediatric abdominal CT. AJR Am J Roentgenol. 2012; 199:670–676. PMID: 22915410.
Article11. Menke J. Comparison of different body size parameters for individual dose adaptation in body CT of adults. Radiology. 2005; 236:565–571. PMID: 16040914.
Article12. Wang J, Duan X, Christner JA, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size specific dose estimation in CT. Part I. Development and validation of methods using the CT image. Med Phys. 2012; 39:6764–6771. PMID: 23127070.
Article13. Wang J, Christner JA, Duan X, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size specific dose estimation in CT. Part II. Implementation on abdomen and thorax phantoms using cross sectional CT images and scanned projection radiograph images. Med Phys. 2012; 39:6772–6778. PMID: 23127071.
Article14. Goo HW. Individualized volume CT dose index determined by cross-sectional area and mean density of the body to achieve uniform image noise of contrast-enhanced pediatric chest CT obtained at variable kV levels and with combined tube current modulation. Pediatr Radiol. 2011; 41:839–847. PMID: 21656275.
Article15. Goo HW, Allmendinger T. Combined electrocardiography- and respiratory-triggered CT of the lung to reduce respiratory misregistration artifacts between imaging slabs in free-breathing children: initial experience. Korean J Radiol. 2017; 18:860–866. PMID: 28860904.
Article16. Kaasalainen T, Palmu K, Reijonen V, Kortesniemi M. Effect of patient centering on patient dose and image noise in chest CT. AJR Am J Roentgenol. 2014; 203:123–130. PMID: 24951205.
Article17. Larson DB, Wang LL, Podberesky DJ, Goske MJ. System for verifiable CT radiation dose optimization based on image quality. part I. Optimization model. Radiology. 2013; 269:167–176. PMID: 23784878.
Article18. Larson DB, Malarik RJ, Hall SM, Podberesky DJ. System for verifiable CT radiation dose optimization based on image quality. part II. Process control system. Radiology. 2013; 269:177–185. PMID: 23784877.
Article19. Li B, Behrman RH, Norbash AM. Comparison of topogram-based body size indices for CT dose consideration and scan protocol optimization. Med Phys. 2012; 39:3456–3465. PMID: 22755725.
Article20. Ikuta I, Warden GI, Andriole KP, Khorasani R, Sodickson A. Estimating patient dose from x-ray tube output metrics: automated measurement of patient size from CT images enables large-scale size-specific dose estimates. Radiology. 2014; 270:472–480. PMID: 24086075.
Article21. Kuo F, Plaza M, Saigal G. Inappropriate arm positioning during scout image acquisition resulting in increased radiation dose while performing a chest CT. Pediatr Radiol. 2012; 42:508–509. PMID: 22322628.
Article22. Goo HW, Suh DS. The influences of tube voltage and scan direction on combined tube current modulation: a phantom study. Pediatr Radiol. 2006; 36:833–840. PMID: 16642311.
Article23. Israel GM, Herlihy S, Rubinowitz AN, Cornfeld D, Brink J. Does a combination of dose modulation with fast gantry rotation time limit CT image quality. AJR Am J Roentgenol. 2008; 191:140–144. PMID: 18562737.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Chest Pain Protocols for Electrocardiography-Gated Dual-Source Cardiothoracic CT in Children and Adults: The Effect of Tube Current Saturation on Radiation Dose Reduction
- Review of the Asian Consortium on Radiation Dose of Pediatric Cardiac CT (ASCI-REDCARD) and Recommendations for a New Edition
- CT radiation dose and radiation reduction strategies
- Method for Automatic Tube Current Selection for Obtaining a Consistent Image Quality and Dose Optimization in a Cardiac Multidetector CT
- Pediatric CT: Understanding of Radiation Dose and Optimization of Imaging Techniques