J Korean Acad Nurs.
2016 Apr;46(2):271-282. 10.4040/jkan.2016.46.2.271.
Adaptation Experience of Living Kidney Donors after Donation
- Affiliations
-
- 1Department of Nursing, Kaya University, Gimhae, Korea.
- 2Department of Nursing·Institute of Health Science, Inje University, Busan, Korea. jhyang@inje.ac.kr
- KMID: 2413157
- DOI: http://doi.org/10.4040/jkan.2016.46.2.271
Abstract
- PURPOSE
This study was done to explore adaptation experience of living kidney donors after donation. Specific aims were to identify challenges donors face in the process of adaptation following surgery and how they interact with recipients and other people.
METHODS
Grounded theory methodology was utilized. Participants were 13 living kidney donors at six months or more after donation. Data were collected by in-depth interviews with individual participants. Data were analyzed using constants comparative method with theoretical saturation.
RESULTS
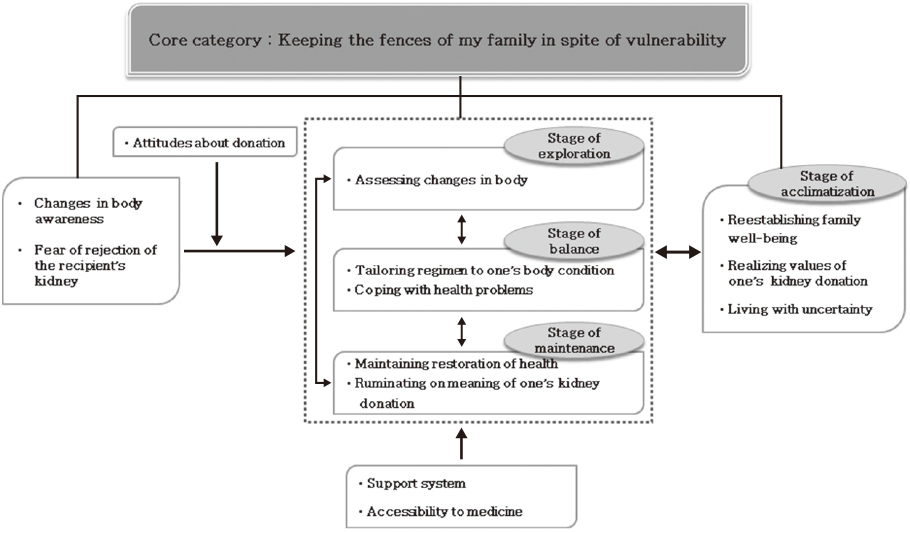
A core category emerged as 'keeping the fences of my family in spite of vulnerability'. The adaptation process after donation was manifested in four phases: exploration, balance, maintenance, and acclimatization. Phenomenon was perception of vulnerability. Strategies to manage the vulnerability were assessing changes of body awareness, tailoring regimen to one's own body condition, coping with health problems, keeping restoration of health, and ruminating on the meaning of one's kidney donation. Consequences were reestablishing family well-being, realizing the values of one's kidney donation, and living with uncertainty.
CONCLUSION
Findings of the study indicate that there is a need for health professionals to understand the vulnerability of living kidney donors and help their family system maintain a healthy and productive life. The results of this study can be used to develop phase-specific, patient-centered, and tailored interventions for living kidney donors.
MeSH Terms
Figure
Cited by 1 articles
-
Experiences of physical complications and sequelae among living liver donors
Sun Ju Jeong, Han Na Kim
Korean J Transplant. 2019;33(2):36-45. doi: 10.4285/jkstn.2019.33.2.36.
Reference
-
1. Okamoto M. Long-term renal function, complications and life expectancy in living kidney donors. World J Transplant. 2012; 2(1):5–8. DOI: 10.5500/wjt.v2.i1.5.2. Ministry of Health & Welfare. Korean Network for Organ Sharing. Annu rep transpl 2012. Seoul: Korean Netword for Organ Sharing;2013.3. Crombie AK, Franklin PM. Family issues implicit in living donation. Mortal. 2006; 11(2):196–210. DOI: 10.1080/13576270600616011.4. Lee BM. Korea is the country of the devoted son and devoted daughter [Internet]. Seoul: Maeil Business News Korea;2013. cited 2014 October 7. Available from: http://news.mk.co.kr/newsRead.php?year=2013&no=356011.5. Park SH. Decision of organ donation by the bucket list [Internet]. Seoul: Newsis;2014. cited 2014 October 7. Available from: http://www.newsis.com/ar_detail/view.html?ar_id=NISX20140820_0013119207&cID=10201&pID=10200.6. Tong A, Chapman JR, Wong G, Kanellis J, McCarthy G, Craig JC. The motivations and experiences of living kidney donors: A thematic synthesis. Am J Kidney Dis. 2012; 60(1):15–26. DOI: 10.1053/j.ajkd.2011.11.043.7. Park MR. Living organ donation [Internet]. Seoul: Medical Observer;2014. cited 2014 November 7. Available from: http://www.monews.co.kr/news/articleView.html?idxno=78873.8. Møjen G, Hallan S, Hartmann A, Foss A, Midtvedt K, Øyen O, et al. Long-term risks for kidney donors. Kidney Int. 2014; 86(1):162–167. DOI: 10.1038/ki.2013.460.9. Tong A, Chapman JR, Wong G, Craig JC. Living kidney donor assessment: challenges, uncertainties and controversies among transplant nephrologists and surgeons. Am J Transplant. 2013; 13(11):2912–2923. DOI: 10.1111/ajt.12411.10. Williams AM, Colefax L, O'Driscoll CT, Dawson S. An exploration of experiences of living renal donors following donation. Nephrol Nurs J. 2009; 36(4):423–427.11. Nagib AM, Refaie AF, Hendy YA, Elfawal MA, Shokeir AA, Bakr MA, et al. Long term prospective assessment of living kidney donors: Single center experience. ISRN Nephrol. 2014; 2014:502414. DOI: 10.1155/2014/502414.12. Kim MH, Kwon OJ, Kang CM. The quality of life for living donors after kidney transplantation. J Korean Soc Transplant. 2012; 26(1):15–22. DOI: 10.4285/jkstn.2012.26.1.15.13. Yi M. Decision-making process for living kidney donors. J Nurs Scholarsh. 2003; 35(1):61–66. DOI: 10.1111/j.1547-5069.2003.00061.x.14. Yi M. Psychosocial adjustment after kidney transplantation. J Korean Acad Nurs. 1998; 28(2):291–302.15. Brown JB, Karley ML, Boudville N, Bullas R, Garg AX, Muirhead N. Living kidney donors' experiences with the health care system. Soc Work Health Care. 2008; 46(3):53–68. DOI: 10.1300/J010v46n03_03.16. Agerskov H, Bistrup C, Ludvigsen MS, Pedersen BD. Living kidney donation: Considerations and decision-making. J Ren care. 2014; 40(2):88–95. DOI: 10.1111/jorc.12071.17. Fujita M, Akabayashi A, Slingsby BT, Kosugi S, Fujimoto Y, Tanaka K. A model of donors' decision-making in adult-to-adult living donor liver transplantation in Japan: Having no choice. Liver Transplant. 2006; 12(5):768–774. DOI: 10.1002/lt.20689.18. Adams-Leander S. The experiences of African-American living kidney donors. Nephrol Nurs J. 2011; 38(6):499–508.19. Langenbach M, Stippel A, Stippel D. Kidney donors' quality of life and subjective evaluation at 2 years after donation. Transplant Proc. 2009; 41(6):2512–2514. DOI: 10.1016/j.transproceed.2009.06.122.20. Corbin J, Strauss A. Basic of qualitative research: Techniques and procedures for developing grounded theory. 3rd ed. Thousand Oaks, CA: Sage;2008.21. Ingram RE, Miranda J, Segal ZV. Cognitive vulnerability to depression. New York, NY: Guilford Press;2000.22. Schipper K, Abma TA, Koops C, Bakker I, Sanderman R, Schroevers MJ. Sweet and sour after renal transplantation: A qualitative study about the positive and negative consequences of renal transplantation. Br J Health Psychol. 2014; 19(3):580–591. DOI: 10.1111/bjhp.12057.23. Andersen MH, Bruserud F, Mathisen L, Wahl AK, Hanestad BR, Fosse E. Follow-up interviews of 12 living kidney donors one yr after open donor nephrectomy. Clin Transplant. 2007; 21(6):702–709. DOI: 10.1111/j.1399-0012.2007.00726.x.24. Korea Ministry of Government Legislation. Internal organs. Transplant act [Internet]. Sejong: Author;2013. cited 2014 October 7. Available from: http://www.law.go.kr/lsSc.do?menuId=0&subMenu=1&query=%EC%9E%A5%EA%B8%B0%EC%9D%B4%EC%8B%9D#undefined.25. Lee HK, Park JH, Chung SY, Choi SJ. Long term outcomes for living renal donors. J Korean Soc Transplant. 2012; 26(1):10–14. DOI: 10.4285/jkstn.2012.26.1.10.26. Choi SB. 'Sharing of sublime life' support system is 'poor' [Internet]. Seoul: Able News;2014. cited 2014 October 7. Available from: http://www.ablenews.co.kr/News/NewsContent.aspx?CategoryCode=0014&NewsCode=001420141126192323370676.27. Tong A, Craig JC, Wong G, Morton J, Armstrong S, Schollum J, et al. "It was just an unconditional gift". Self reflections of non-directed living kidney donors. Clin Transplant. 2012; 26(4):589–599. DOI: 10.1111/j.1399-0012.2011.01578.x.28. Weng LC, Huang HL, Wang YW, Chang CL, Tsai CH, Lee WC. The coping experience of Taiwanese male donors in living donor liver transplantation. Nurs Res. 2012; 61(2):133–139. DOI: 10.1097/NNR.0b013e3182475688.29. Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Scholarsh. 1990; 22(4):256–262. DOI: 10.1111/j.1547-5069.1990.tb00225.x.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experiences of living organ donors about advocator in Korea
- Machine learning based prediction model for renal adaptation in living kidney donors
- Long-term follow-up of over 600 living-related kidney donors: single center experience
- The Phenomenological Study of Kidney Donors' Experiences
- The Quality of Life for Living Donors after Kidney Transplantation