Korean J Ophthalmol.
2018 Jun;32(3):228-233. 10.3341/kjo.2017.0064.
Long-term Surgical Outcomes of Initial Postoperative Overcorrection in Adults with Intermittent Exotropia
- Affiliations
-
- 1Department of Ophthalmology, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. hjpaik@gilhospital.com
- KMID: 2412802
- DOI: http://doi.org/10.3341/kjo.2017.0064
Abstract
- PURPOSE
To evaluate the relationship between initial postoperative overcorrection and long-term surgical success in exotropia patients.
METHODS
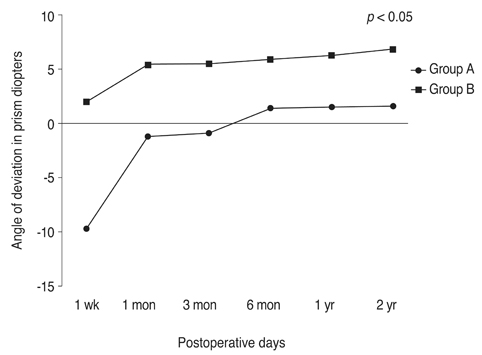
The medical records of 46 patients who underwent surgery for intermittent exotropia after the age of 18 were enrolled. Enrolled patients also had at least 2 years of postoperative follow-up. Based on the initial postoperative deviation at distance measured by prism and the alternating cover test at 1 week, patients were assigned to one of the following groups: group A included patients who demonstrated any esodeviation, while group B included patients who showed orthophoria to exodeviation of 10 prism diopters. The records were analyzed to determine the preoperative deviation with stereoacuity and postoperative deviations with stereoacuity at the follow-up examinations at the following intervals: 1 week; 1, 3, and 6 months; and 1 and 2 years. A comparison between groups for demographic data and preoperative and postoperative angles of deviation was performed using analysis of variance.
RESULTS
Of the 46 patients with intermittent exotropia included in this study, 18 (39%) belonged to group A, while 28 (73%) belonged to group B. The postoperative angle of deviation for distant fixation until 2 years of follow-up showed statistically significant differences in each group (p < 0.003 in all comparisons). The amount of exodrift until 2 years in group A (from −9.7 ± 6.1 to 1.6 ± 3.7) was greater than that in group B (from 2.0 ± 2.7 to 6.8 ± 5.6). The long-term surgical success rate within 2 years of surgery was significantly better in group A than in group B (p = 0.027). The number of patients with intermittent diplopia and the duration of diplopia were greater in group A (n = 8) than in group B (n = 2).
CONCLUSIONS
Long-term surgical success was achieved in 89% of patients who were initially overcorrected. Overcorrection of an average of 10 prism diopters at the first postoperative week was found to be associated with a more favorable long-term surgical outcome.
Figure
Cited by 1 articles
-
Long-term Results of Slanted Recession of Bilateral Lateral Rectus Muscle for Intermittent Exotropia with Convergence Insufficiency
Ji Min Kwon, Soo Jung Lee
Korean J Ophthalmol. 2019;33(4):353-358. doi: 10.3341/kjo.2019.0031.
Reference
-
1. Ing MR, Nishimura J, Okino L. Outcome study of bilateral lateral rectus recession for intermittent exotropia in children. Ophthalmic Surg Lasers. 1999; 30:110–117.
Article2. Jampolsky A. Treatment of exodeviations. Trans New Orleans Acad Ophthalmol. 1986; 34:201–234.3. Beneish R, Flanders M. The role of stereopsis and early postoperative alignment in long-term surgical results of intermittent exotropia. Can J Ophthalmol. 1994; 29:119–124.4. Clarke WN, Noel LP. Surgical results in intermittent exotropia. Can J Ophthalmol. 1981; 16:66–69.5. Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye (Lond). 2006; 20:1268–1272.
Article6. Raab EL, Parks MM. Recession of the lateral recti: early and late postoperative alignments. Arch Ophthalmol. 1969; 82:203–208.7. Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981; 99:1814–1818.
Article8. Schlossman A, Muchnick RS, Stern KS. The surgical management of intermittent exotropia in adults. Ophthalmology. 1983; 90:1166–1171.
Article9. Awadein A, Eltanamly RM, Elshazly M. Intermittent exotropia: relation between age and surgical outcome: a change-point analysis. Eye (Lond). 2014; 28:587–593.
Article10. Wang J, Hatt SR, O'Connor AR, et al. Final version of the Distance Randot Stereotest: normative data, reliability, and validity. J AAPOS. 2010; 14:142–146.
Article11. Astle AT, Foulsham T, Foss AJ, McGraw PV. Is the frequency of adult strabismus surgery increasing? Ophthalmic Physiol Opt. 2016; 36:487–493.
Article12. Cho SC, Yang HK, Hwang JM. Three-year surgical outcome of exotropia. J Korean Ophthalmol Soc. 2012; 53:1674–1679.
Article13. Jung EH, Kim SJ, Yu YS. Factors associated with surgical success in adult patients with exotropia. J AAPOS. 2016; 20:511–514.
Article14. Hatsukawa Y. Short-term and long-term prognosis of recession-resection surgery for exotropia. Nippon Ganka Gakkai Zasshi. 1992; 96:1466–1476.15. Rogers GL, Chazan S, Fellows R, Tsou BH. Strabismus surgery and its effect upon infant development in congenital esotropia. Ophthalmology. 1982; 89:479–483.
Article16. Arthur BW, Smith JT, Scott WE. Long-term stability of alignment in the monofixation syndrome. J Pediatr Ophthalmol Strabismus. 1989; 26:224–231.
Article17. Morris RJ, Scott WE, Dickey CF. Fusion after surgical alignment of longstanding strabismus in adults. Ophthalmology. 1993; 100:135–138.
Article18. Cho YA, Lee DS, Kim EJ. Long-standing adult horizontal strabismus with early childhood onset. J Korean Ophthalmol Soc. 1993; 34:782–787.19. Kushner BJ, Morton GV. Postoperative binocularity in adults with longstanding strabismus. Ophthalmology. 1992; 99:316–319.
Article20. Lal G, Holmes JM. Postoperative stereoacuity following realignment for chronic acquired strabismus in adults. J AAPOS. 2002; 6:233–237.
Article21. Lee KS, Cho YA, Roh GH. Stereopsis after surgery in longstanding adult horizontal strabismus. J Korean Ophthalmol Soc. 1999; 40:1656–1662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors related to Surgical Results of Intermittent Exotropia
- Relationship Between Surgical Result and Alignment on The Day of Surgery in Intermittent Exotropia
- Short-Term Changes of Immediate Postoperative Deviation after Lateral Rectus Recession for Intermittent Exotropia
- The influence of fusional divergence on the surgical results in intermittent exotropia
- Related Factors of Surgical Outcome of Unilateral R and R for Basic Type Intermittent Exotropia in Children