Yonsei Med J.
2018 Jul;59(5):624-632. 10.3349/ymj.2018.59.5.624.
Randomized Comparison of Strut Coverage between Ticagrelor and Clopidogrel in Acute Myocardial Infarction at 3-Month Optical Coherence Tomography
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. kimbk@yuhs.ac
- 2Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- 3Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2412653
- DOI: http://doi.org/10.3349/ymj.2018.59.5.624
Abstract
- PURPOSE
This study aimed to compare the effects of ticagrelor and clopidogrel on early neointimal healing assessed with optical coherence tomography (OCT) after drug-eluting stent (DES) implantation in patients with acute myocardial infarction (AMI).
MATERIALS AND METHODS
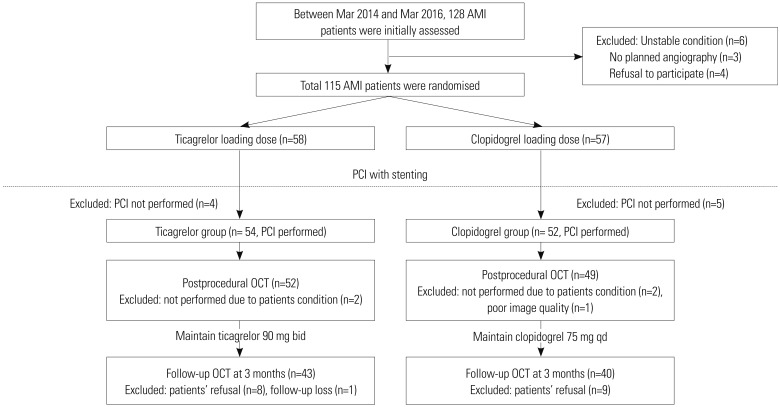
AMI patients were randomly assigned to either the ticagrelor or clopidogrel arm. After DES implantation, OCT was performed to assess the percentages of uncovered struts immediately after procedure and 3 months later.
RESULTS
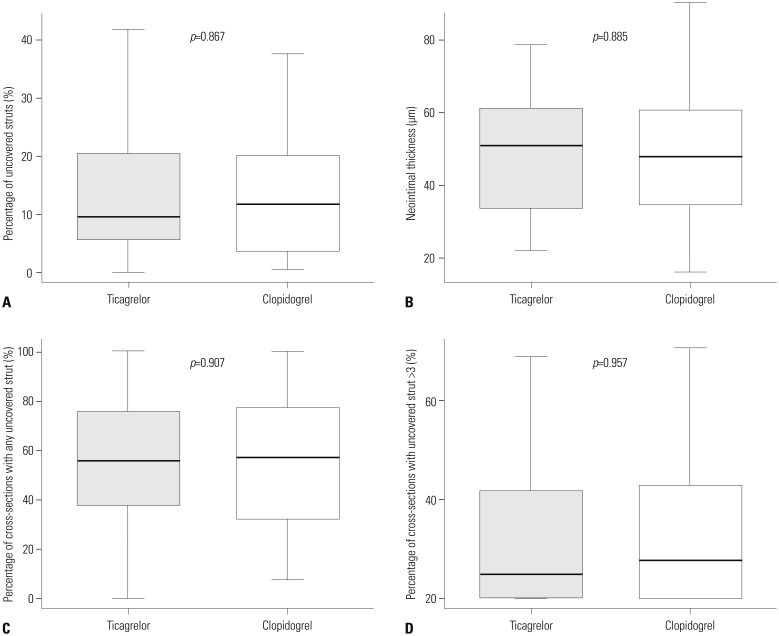
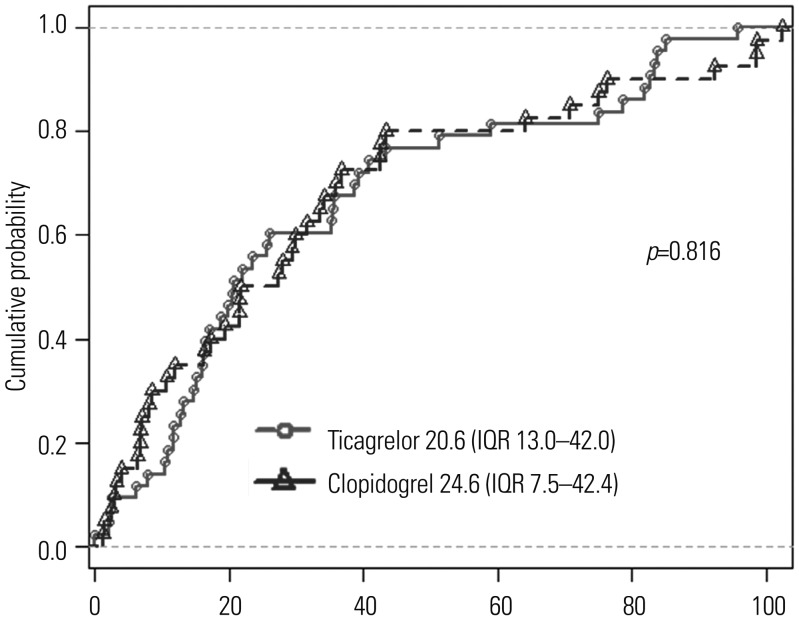
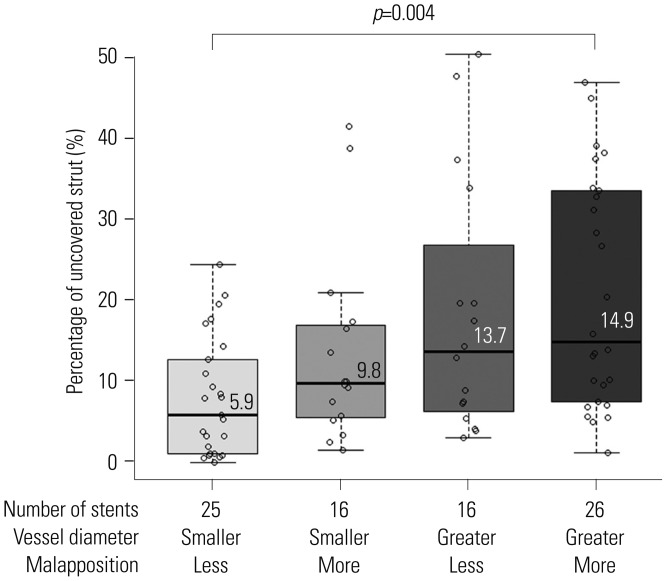
Due to early termination, 83 patients out of 106 initially enrolled patients (24% of planned participants) underwent 3-month OCT. Differences in vascular healing patterns between the two groups, including percentage of uncovered struts on 3-month OCT (9.6% vs. 11.7% in ticagrelor vs. clopidogrel, respectively; p=0.867), neointimal thickness, percentage of malapposed struts, and healing scores did not reach statistical significance. The predictors of uncovered strut on 3-month OCT included greater reference vessel diameter [odds ratio (OR)=1.96, p < 0.001] and more malapposed struts (OR=1.12, p=0.003).
CONCLUSION
The current study did not explore favorable effect of ticagrelor on 3-month vascular healing after DES implantation. Our findings should only be considered for generating hypothesis, due to insufficient power.
MeSH Terms
Figure
Reference
-
1. Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–1057. PMID: 19717846.
Article2. Bonaca MP, Bhatt DL, Cohen M, Steg PG, Storey RF, Jensen EC, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med. 2015; 372:1791–1800. PMID: 25773268.
Article3. Cattaneo M, Schulz R, Nylander S. Adenosine-mediated effects of ticagrelor: evidence and potential clinical relevance. J Am Coll Cardiol. 2014; 63:2503–2509. PMID: 24768873.4. Bonello L, Frere C, Cointe S, Laine M, Mancini J, Thuny F, et al. Ticagrelor increases endothelial progenitor cell level compared to clopidogrel in acute coronary syndromes: a prospective randomized study. Int J Cardiol. 2015; 187:502–507. PMID: 25846661.
Article5. Gomez-Lara J, Radu M, Brugaletta S, Farooq V, Diletti R, Onuma Y, et al. Serial analysis of the malapposed and uncovered struts of the new generation of everolimus-eluting bioresorbable scaffold with optical coherence tomography. JACC Cardiovasc Interv. 2011; 4:992–1001. PMID: 21939939.
Article6. Kim BK, Shin DH, Kim JS, Ko YG, Choi D, Jang Y, et al. Randomized comparison of acute stent malapposition between platinumchromium versus cobalt-chromium everolimus-eluting stents. Int J Cardiovasc Imaging. 2015; 31:269–277. PMID: 25345751.
Article7. Matsumoto D, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, et al. Neointimal coverage of sirolimus-eluting stents at 6-month follow-up: evaluated by optical coherence tomography. Eur Heart J. 2007; 28:961–967. PMID: 17135281.
Article8. Karjalainen PP, Varho V, Nammas W, Mikkelsson J, Pietilä M, Ylitalo A, et al. Early neointimal coverage and vasodilator response following biodegradable polymer sirolimus-eluting vs. durable polymer zotarolimus-eluting stents in patients with acute coronary syndrome–HATTRICK-OCT trial. Circ J. 2015; 79:360–367. PMID: 25502167.9. Sabaté M, Windecker S, Iñiguez A, Okkels-Jensen L, Cequier A, Brugaletta S, et al. Everolimus-eluting bioresorbable stent vs. durable polymer everolimus-eluting metallic stent in patients with ST-segment elevation myocardial infarction: results of the randomized ABSORB ST-segment elevation myocardial infarction-TROFI II trial. Eur Heart J. 2016; 37:229–240. PMID: 26405232.
Article10. Kim S, Kim JS, Shin DH, Kim BK, Ko YG, Choi D, et al. Comparison of early strut coverage between zotarolimus- and everolimuseluting stents using optical coherence tomography. Am J Cardiol. 2013; 111:1–5. PMID: 23040589.
Article11. Kim JS, Jang IK, Kim JS, Kim TH, Takano M, Kume T, et al. Optical coherence tomography evaluation of zotarolimus-eluting stents at 9-month follow-up: comparison with sirolimus-eluting stents. Heart. 2009; 95:1907–1912. PMID: 19535352.
Article12. Kang HJ, Clare RM, Gao R, Held C, Himmelmann A, James SK, et al. Ticagrelor versus clopidogrel in Asian patients with acute coronary syndrome: a retrospective analysis from the Platelet Inhibition and Patient Outcomes (PLATO) Trial. Am Heart J. 2015; 169:899–905. PMID: 26027629.
Article13. Kim C, Shin DH, Ahn CM, Kim JS, Kim BK, Ko YG, et al. The use pattern and clinical impact of new antiplatelet agents including prasugrel and ticagrelor on 30-day outcomes after acute myocardial infarction in Korea: Korean Health Insurance Review and Assessment Data. Korean Circ J. 2017; 47:888–897. PMID: 29035430.
Article14. Kipshidze N, Dangas G, Tsapenko M, Moses J, Leon MB, Kutryk M, et al. Role of the endothelium in modulating neointimal formation: vasculoprotective approaches to attenuate restenosis after percutaneous coronary interventions. J Am Coll Cardiol. 2004; 44:733–739. PMID: 15312851.15. Hayashi K, Nakamura S, Morishita R, Moriguchi A, Aoki M, Matsumoto K, et al. In vivo transfer of human hepatocyte growth factor gene accelerates re-endothelialization and inhibits neointimal formation after balloon injury in rat model. Gene Ther. 2000; 7:1664–1671. PMID: 11083475.
Article16. Patil SB, Jackman LE, Francis SE, Judge HM, Nylander S, Storey RF. Ticagrelor effectively and reversibly blocks murine platelet P2Y12-mediated thrombosis and demonstrates a requirement for sustained P2Y12 inhibition to prevent subsequent neointima. Arterioscler Thromb Vasc Biol. 2010; 30:2385–2391. PMID: 21071697.17. Sürer S, Toktas F, Ay D, Eris C, Yavuz S, Turk T, et al. Effect of the P2Y12 antagonist ticagrelor on neointimal hyperplasia in a rabbit carotid anastomosis model. Interact Cardiovasc Thorac Surg. 2014; 19:198–204. PMID: 24876217.18. Guagliumi G, Sirbu V, Musumeci G, Gerber R, Biondi-Zoccai G, Ikejima H, et al. Examination of the in vivo mechanisms of late drug-eluting stent thrombosis: findings from optical coherence tomography and intravascular ultrasound imaging. JACC Cardiovasc Interv. 2012; 5:12–20. PMID: 22230145.19. Won H, Shin DH, Kim BK, Mintz GS, Kim JS, Ko YG, et al. Optical coherence tomography derived cut-off value of uncovered stent struts to predict adverse clinical outcomes after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2013; 29:1255–1263. PMID: 23615849.
Article20. Forrester JS, Fishbein M, Helfant R, Fagin J. A paradigm for restenosis based on cell biology: clues for the development of new preventive therapies. J Am Coll Cardiol. 1991; 17:758–769. PMID: 1993798.
Article21. Hara T, Ughi GJ, McCarthy JR, Erdem SS, Mauskapf A, Lyon SC, et al. Intravascular fibrin molecular imaging improves the detection of unhealed stents assessed by optical coherence tomography in vivo. Eur Heart J. 2017; 38:447–455. PMID: 26685129.22. Padfield GJ, Newby DE, Mills NL. Understanding the role of endothelial progenitor cells in percutaneous coronary intervention. J Am Coll Cardiol. 2010; 55:1553–1565. PMID: 20378071.
Article23. Finn AV, Nakazawa G, Ladich E, Kolodgie FD, Virmani R. Does underlying plaque morphology play a role in vessel healing after drug-eluting stent implantation? JACC Cardiovasc Imaging. 2008; 1:485–488. PMID: 19356471.
Article24. Cayla G, Montalescot G, Collet JP. Ticagrelor to prevent restenosis: new drug for an old hypothesis? Arterioscler Thromb Vasc Biol. 2010; 30:2320–2322. PMID: 21084699.25. Joner M, Finn AV, Farb A, Mont EK, Kolodgie FD, Ladich E, et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol. 2006; 48:193–202. PMID: 16814667.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Infarct Size between the Loading of Ticagrelor and Clopidogrel in Patients with Acute Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention
- Hypersensitivity to ticagrelor and low response to clopidogrel: a case report
- Clinical Outcomes of Ticagrelor in Korean Patients with Acute Myocardial Infarction without High Bleeding Risk
- Successful Primary Percutaneous Coronary Intervention without Stenting: Insight from Optimal Coherence Tomography
- New Oral Antiplatelet Agents