Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):159-163. 10.14701/ahbps.2018.22.2.159.
Long term recurrence in primary liver neuroendocrine tumor: Report of a single case and review of literature
- Affiliations
-
- 1General and Emergency Surgery Department, Angelo Hospital, Venice, Italy. giovanni.pirozzolo@gmail.com
- 2University of Padua, Padova, Italy.
- 3General Surgery Department, Regional Hospital Peja, Peja, Kosovo.
- KMID: 2412432
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.159
Abstract
- Primary liver neuroendocrine tumors (PLNETs) are rare tumors of the liver. They share some common characteristics with neuroendocrine tumors (NETs) of the extrahepatic bile ducts, such as slow rise, hormonal, and histological features. Nevertheless, they possess some peculiarities and the major feature is the difference in the metastatic potential between PLNETs and NETs. PLNETs have less metastatic potential compared with NETs, which is the main factor based on which differential diagnosis between the two groups is achieved. There exists few reports disease's long-term outcome, especially about the recurrences management. We report the case of a 52-year-old woman admitted to hospital for jaundice and presence of liver mass. She underwent extended right hepatectomy and subsequently, PLNET was revealed. After 9 years, a new mass was discovered in the remnant liver, far from the resection line, and was surgically removed. Histological examination confirmed a PLNET recurrence. The patient is alive and doing well after a year of surgery. We conducted a review of the literature on recurrent PLNETS. Five papers followed our inclusion criteria and included 10 patients. Clinical presentation was mostly nonspecific in included cases and no carcinoid syndrome was reported. Median overall survival and median disease-free survival periods were 22 and 5 months, respectively. The primary disease was treated with surgical resection in all the included cases and recurrent diseases were mostly treated with non-surgical techniques (mainly transarterial chemoembolization). In conclusion, more studies should be conducted in order to have significant data about this uncommon neoplasm. Finally, considering the lack of data on long-term outcome, a long and accurate follow-up should be considered.
MeSH Terms
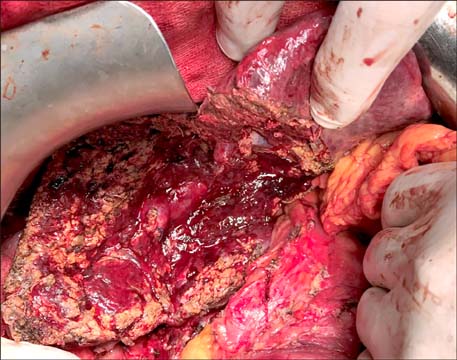
Figure
Reference
-
1. Caplin ME, Buscombe JR, Hilson AJ, Jones AL, Watkinson AF, Burroughs AK. Carcinoid tumour. Lancet. 1998; 352:799–805.
Article2. Yamashita Y, Takahashi M, Tsuji A, Korogi Y, Uozumi H, Kimura Y. Primary carcinoid tumor of the liver: a case report. J Comput Tomogr. 1986; 10:313–317.
Article3. Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011; 40:1–18. vii
Article4. Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008; 9:61–72.
Article5. Hirabayashi K, Zamboni G, Nishi T, Tanaka A, Kajiwara H, Nakamura N. Histopathology of gastrointestinal neuroendocrine neoplasms. Front Oncol. 2013; 3:2.
Article6. Gravante G, De Liguori Carino N, Overton J, Manzia TM, Orlando G. Primary carcinoids of the liver: a review of symptoms, diagnosis and treatments. Dig Surg. 2008; 25:364–368.
Article7. Zhang A, Xiang J, Zhang M, Zheng S. Primary hepatic carcinoid tumours: clinical features with an emphasis on carcinoid syndrome and recurrence. J Int Med Res. 2008; 36:848–859.
Article8. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. Geneva: World Health Organization;2010.9. Kano Y, Kakinuma S, Goto F, Azuma S, Nishimura-Sakurai Y, Itsui Y, et al. Primary hepatic neuroendocrine carcinoma with a cholangiocellular carcinoma component in one nodule. Clin J Gastroenterol. 2014; 7:449–454.
Article10. Ichiki M, Nishida N, Furukawa A, Kanasaki S, Ohta S, Miki Y. Imaging findings of primary hepatic carcinoid tumor with an emphasis on MR imaging: case study. SpringerPlus. 2014; 3:607.
Article11. Yalav O, Ülkü A, Akçam TA, Demiryürek H, Doran F. Primary hepatic neuroendocrine tumor: five cases with different preoperative diagnoses. Turk J Gastroenterol. 2012; 23:272–278.
Article12. Gao J, Hu Z, Wu J, Bai L, Chai X. Primary hepatic carcinoid tumor. World J Surg Oncol. 2011; 9:151.
Article13. Huang YQ, Xu F, Yang JM, Huang B. Primary hepatic neuroendocrine carcinoma: clinical analysis of 11 cases. Hepatobiliary Pancreat Dis Int. 2010; 9:44–48.14. Onaitis MW, Kirshbom PM, Hayward TZ, Quayle FJ, Feldman JM, Seigler HF, et al. Gastrointestinal carcinoids: characterization by site of origin and hormone production. Ann Surg. 2000; 232:549–556.
Article15. Akerström G, Hellman P, Hessman O, Osmak L. Management of midgut carcinoids. J Surg Oncol. 2005; 89:161–169.16. Fenwick SW, Wyatt JI, Toogood GJ, Lodge JP. Hepatic resection and transplantation for primary carcinoid tumors of the liver. Ann Surg. 2004; 239:210–219.
Article17. Park CH, Chung JW, Jang SJ, Chung MJ, Bang S, Park SW, et al. Clinical features and outcomes of primary hepatic neuroendocrine carcinomas. J Gastroenterol Hepatol. 2012; 27:1306–1311.
Article18. Sioutos N, Virta S, Kessimian N. Primary hepatic carcinoid tumor. An electron microscopic and immunohistochemical study. Am J Clin Pathol. 1991; 95:172–175.
Article19. Kehagias D, Moulopoulos L, Smirniotis V, Pafiti A, Ispanopoulos S, Vlahos L. Imaging findings in primary carcinoid tumour of the liver with gastrin production. Br J Radiol. 1999; 72:207–209.
Article20. Nishimori H, Tsuji K, Miyamoto N, Sakurai Y, Mitsui S, Kang JH, et al. Recurrence of primary hepatic carcinoid tumor in the remnant liver 13 yr after resection. Int J Gastrointest Cancer. 2005; 35:147–151.
Article21. Knox CD, Anderson CD, Lamps LW, Adkins RB, Pinson CW. Long-term survival after resection for primary hepatic carcinoid tumor. Ann Surg Oncol. 2003; 10:1171–1175.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Small Cell Neuroendocrine Carcinoma of the Breast: A Case Report With Literature Review
- A Case of Primary Small Cell Neuroendocrine Carcinoma in the Stomach
- Primary Hepatic Neuroendocrine Tumor Arising at a Young Age: Rare Case Report and Literature Review
- Primary Neuroendocrine Carcinoma of the Breast: A Case Report and Literature Review
- Primary multifocal cystic signet ring neuroendocrine tumor of liver: a case report