Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):93-100. 10.14701/ahbps.2018.22.2.93.
Clinical significance of post-hepatectomy hepatic failure in patients with liver metastases from colorectal cancer
- Affiliations
-
- 1Division of Hepatobiliary, Pancreas Surgery and Liver Transplantation, Department of Surgery, Korea University College of Medicine, Seoul, Korea. kimds1@korea.ac.kr
- KMID: 2412423
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.93
Abstract
- BACKGROUNDS/AIMS
This study attempted to identify risk factors for development of post-hepatectomy hepatic failure (PHF) and its effect on long-term survival of patients with liver metastases from colorectal cancer.
METHODS
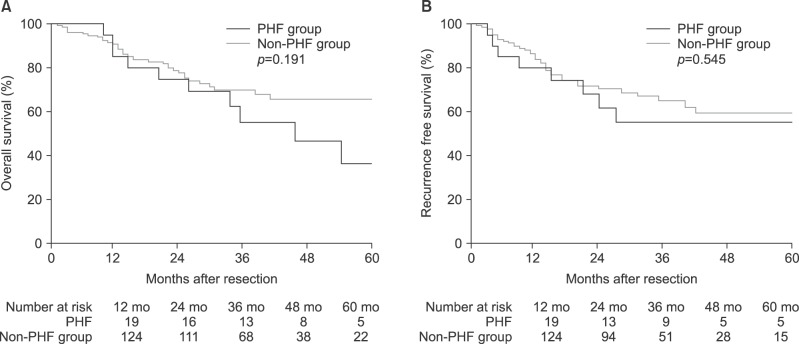
We carried out a retrospective study of 143 patients who had been diagnosed with liver metastases from colorectal cancer and who had undergone hepatectomy between 2003 and 2010. We allocated these patients to PHF and non-PHF groups, using the definition of the International Study Group of Liver Surgery, and compared the clinical factors of the two groups, using Cox regression and Kaplan-Meier analysis to evaluate the differences in overall survival (OS) and recurrence-free survival (RFS) between these groups.
RESULTS
The PHF group comprised 19 patients (13.3%); all had Grade A PHF. Independent risk factors for development of PHF were metachronous liver metastases and major hepatectomy. The differences between the PHF and non-PHF groups in OS or RFS were not statistically significant; however, the PHF group tended to have a worse prognosis. Multivariate analysis revealed significant associations between OS and the factors of poor differentiation of the primary colorectal cancer, major hepatectomy, and positive resection margin.
CONCLUSIONS
Major hepatectomy is an important risk factor for PHF in patients with liver metastases from colorectal cancer. The pathological characteristics of the primary tumor are more important as predictors than is Grade A PHF.
Keyword
MeSH Terms
Figure
Reference
-
1. Spolverato G, Ejaz A, Azad N, Pawlik TM. Surgery for colorectal liver metastases: the evolution of determining prognosis. World J Gastrointest Oncol. 2013; 5:207–221. PMID: 24363829.
Article2. Jones RP, Jackson R, Dunne DF, Malik HZ, Fenwick SW, Poston GJ, et al. Systematic review and meta-analysis of follow-up after hepatectomy for colorectal liver metastases. Br J Surg. 2012; 99:477–486. PMID: 22261895.3. Akgül Ö, Çetinkaya E, Ersöz Ş, Tez M. Role of surgery in colorectal cancer liver metastases. World J Gastroenterol. 2014; 20:6113–6122. PMID: 24876733.
Article4. Khatri VP, Chee KG, Petrelli NJ. Modern multimodality approach to hepatic colorectal metastases: solutions and controversies. Surg Oncol. 2007; 16:71–83. PMID: 17532622.
Article5. Chen JX, Ran HQ, Sun CQ. Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis. Ann Surg Treat Res. 2016; 90:287–291. PMID: 27186574.
Article6. Narita M, Oussoultzoglou E, Bachellier P, Jaeck D, Uemoto S. Post-hepatectomy liver failure in patients with colorectal liver metastases. Surg Today. 2015; 45:1218–1226. PMID: 25628126.
Article7. Fukushima K, Fukumoto T, Kuramitsu K, Kido M, Takebe A, Tanaka M, et al. Assessment of ISGLS definition of posthepatectomy liver failure and its effect on outcome in patients with hepatocellular carcinoma. J Gastrointest Surg. 2014; 18:729–736. PMID: 24297653.
Article8. Iguchi K, Hatano E, Yamanaka K, Tanaka S, Taura K, Uemoto S. The impact of posthepatectomy liver failure on the recurrence of hepatocellular carcinoma. World J Surg. 2014; 38:150–158. PMID: 24132820.
Article9. Shi JH, Huitfeldt HS, Suo ZH, Line PD. Growth of hepatocellular carcinoma in the regenerating liver. Liver Transpl. 2011; 17:866–874. PMID: 21542129.
Article10. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011; 149:713–724. PMID: 21236455.
Article11. Couinaud C. Liver lobes and segments: notes on the anatomical architecture and surgery of the liver. Presse Med. 1954; 62:709–712. PMID: 13177441.12. Kim SH, Kang DR, Lee JG, Kim DY, Ahn SH, Han KH, et al. Early predictor of mortality due to irreversible posthepatectomy liver failure in patients with hepatocellular carcinoma. World J Surg. 2013; 37:1028–1033. PMID: 23423450.
Article13. Cescon M, Vetrone G, Grazi GL, Ramacciato G, Ercolani G, Ravaioli M, et al. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg. 2009; 249:995–1002. PMID: 19474679.14. Schreckenbach T, Liese J, Bechstein WO, Moench C. Posthepatectomy liver failure. Dig Surg. 2012; 29:79–85. PMID: 22441624.
Article15. Nakamura N, Hatano E, Iguchi K, Seo S, Taura K, Uemoto S. Posthepatectomy liver failure affects long-term function after resection for hepatocellular carcinoma. World J Surg. 2016; 40:929–936. PMID: 26589593.
Article16. Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005; 242:824–828. discussion 828-829. PMID: 16327492.17. Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007; 204:854–862. discussion 862-864. PMID: 17481498.
Article18. Skrzypczyk C, Truant S, Duhamel A, Langlois C, Boleslawski E, Koriche D, et al. Relevance of the ISGLS definition of posthepatectomy liver failure in early prediction of poor outcome after liver resection: study on 680 hepatectomies. Ann Surg. 2014; 260:865–870. discussion 870. PMID: 25243550.19. Bilimoria MM, Lauwers GY, Doherty DA, Nagorney DM, Belghiti J, Do KA, et al. Underlying liver disease, not tumor factors, predicts long-term survival after resection of hepatocellular carcinoma. Arch Surg. 2001; 136:528–535. PMID: 11343543.
Article20. van den Broek MA, Olde Damink SW, Dejong CH, Lang H, Malagó M, Jalan R, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int. 2008; 28:767–780. PMID: 18647141.
Article21. Harun N, Nikfarjam M, Muralidharan V, Christophi C. Liver regeneration stimulates tumor metastases. J Surg Res. 2007; 138:284–290. PMID: 17254608.
Article22. Vibert E, Pittau G, Gelli M, Cunha AS, Jamot L, Faivre J, et al. Actual incidence and long-term consequences of posthepatectomy liver failure after hepatectomy for colorectal liver metastases. Surgery. 2014; 155:94–105. PMID: 24694360.
Article23. Ribeiro HS, Costa WL Jr, Diniz AL, Godoy AL, Herman P, Coudry RA, et al. Extended preoperative chemotherapy, extent of liver resection and blood transfusion are predictive factors of liver failure following resection of colorectal liver metastasis. Eur J Surg Oncol. 2013; 39:380–385. PMID: 23351680.
Article24. Arru M, Aldrighetti L, Castoldi R, Di Palo S, Orsenigo E, Stella M, et al. Analysis of prognostic factors influencing long-term survival after hepatic resection for metastatic colorectal cancer. World J Surg. 2008; 32:93–103. PMID: 18027020.
Article25. Mbah NA, Scoggins C, McMasters K, Martin R. Impact of hepatectomy margin on survival following resection of colorectal metastasis: the role of adjuvant therapy and its effects. Eur J Surg Oncol. 2013; 39:1394–1399. PMID: 24084087.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver Metastases in Colorectal Cancer
- Management of Colorectal Cancer Liver Metastasis
- Factors Affecting Survival Rate Following Hepatic Resection for Metastatic Colorectal Cancer
- Hepatic Resection in Patients with Liver Metastasis from Gastric Cancer
- Parenchymal-sparing hepatectomy for multiple bilobar colorectal liver metastases in a Jehovah’s witness: a case report