J Korean Soc Radiol.
2018 Jun;78(6):389-403. 10.3348/jksr.2018.78.6.389.
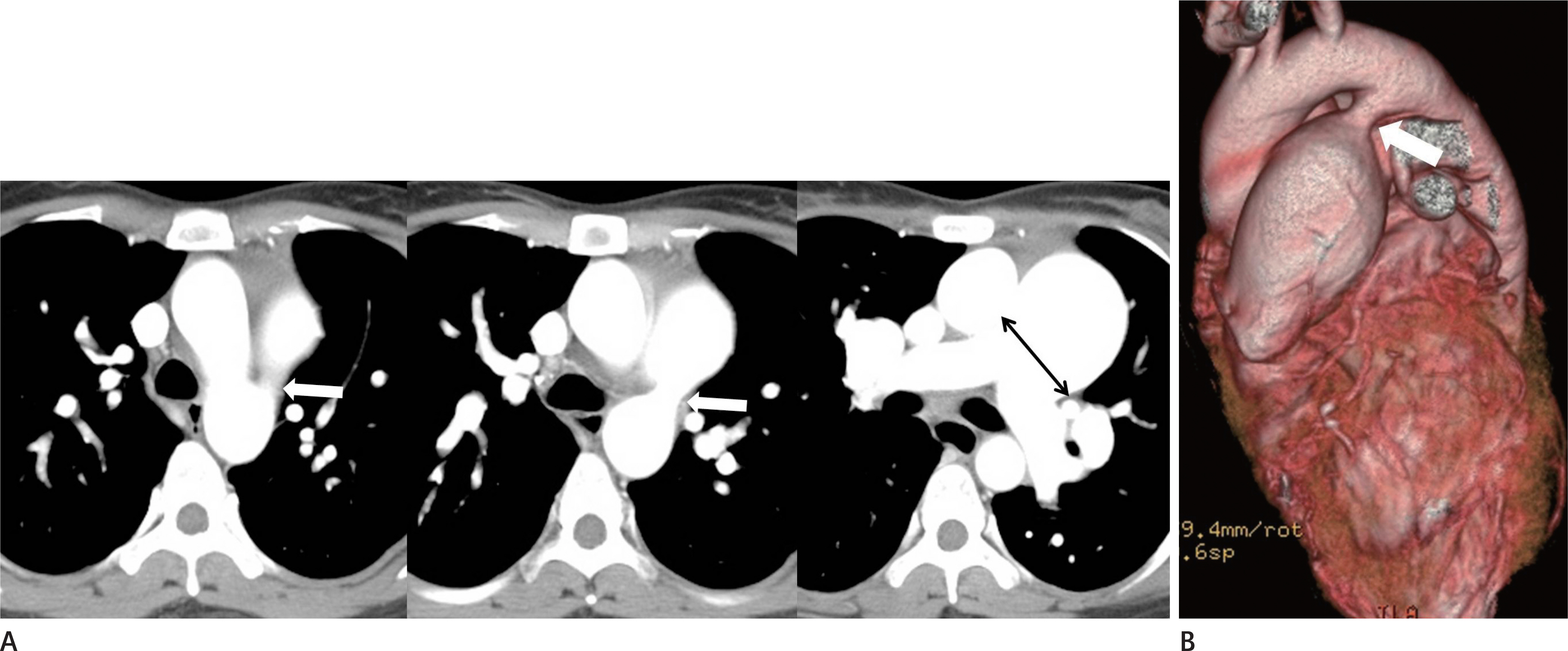
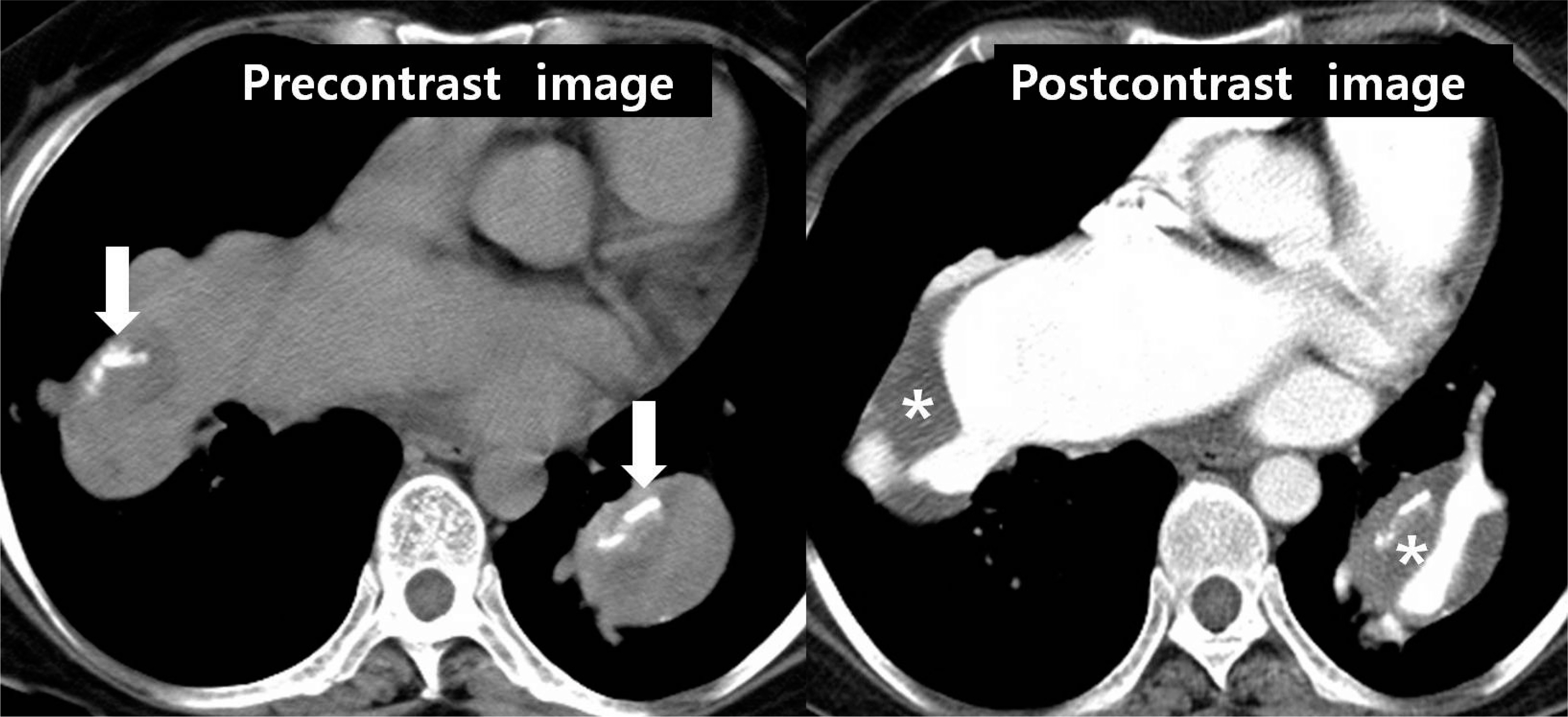
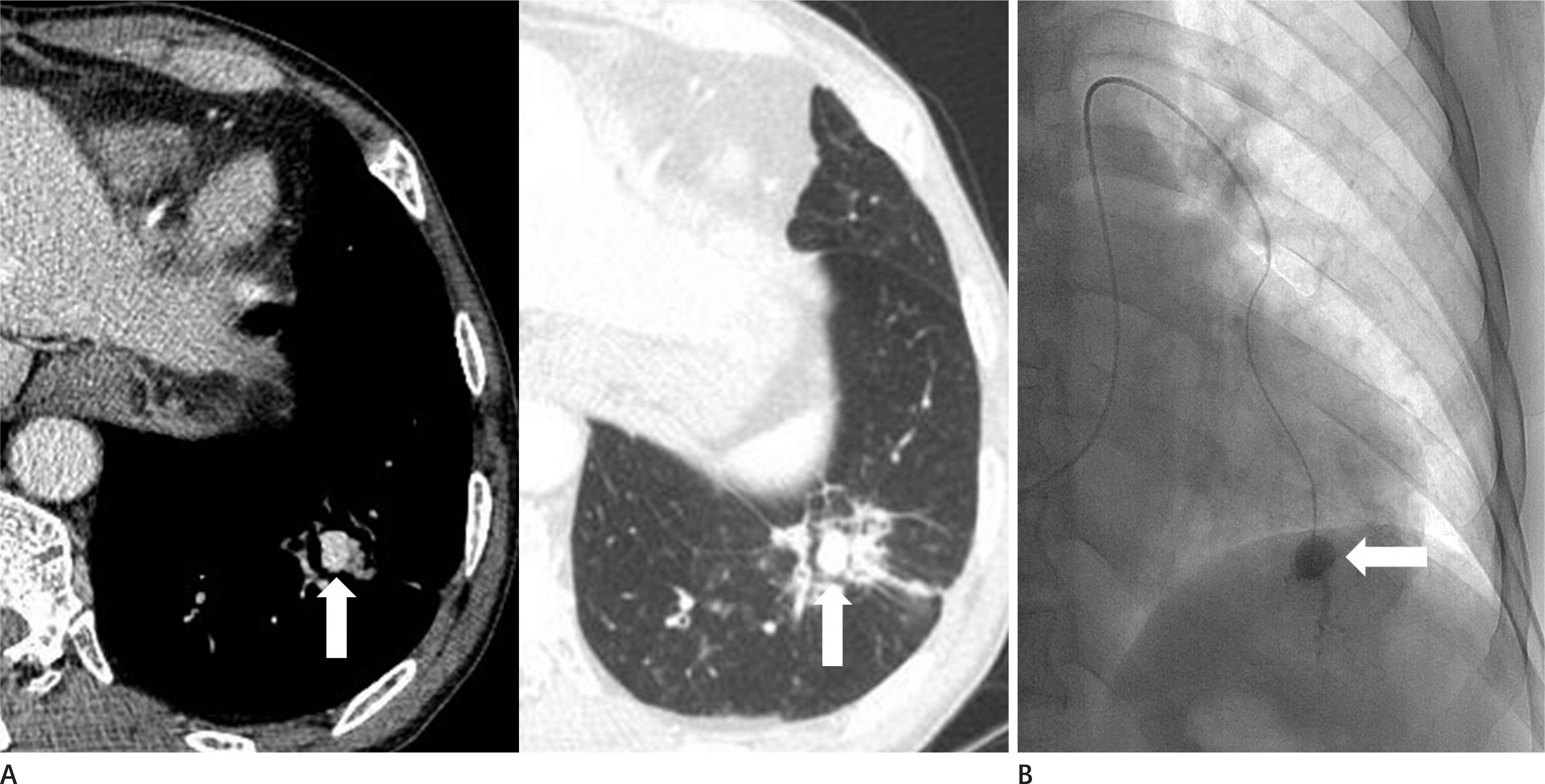
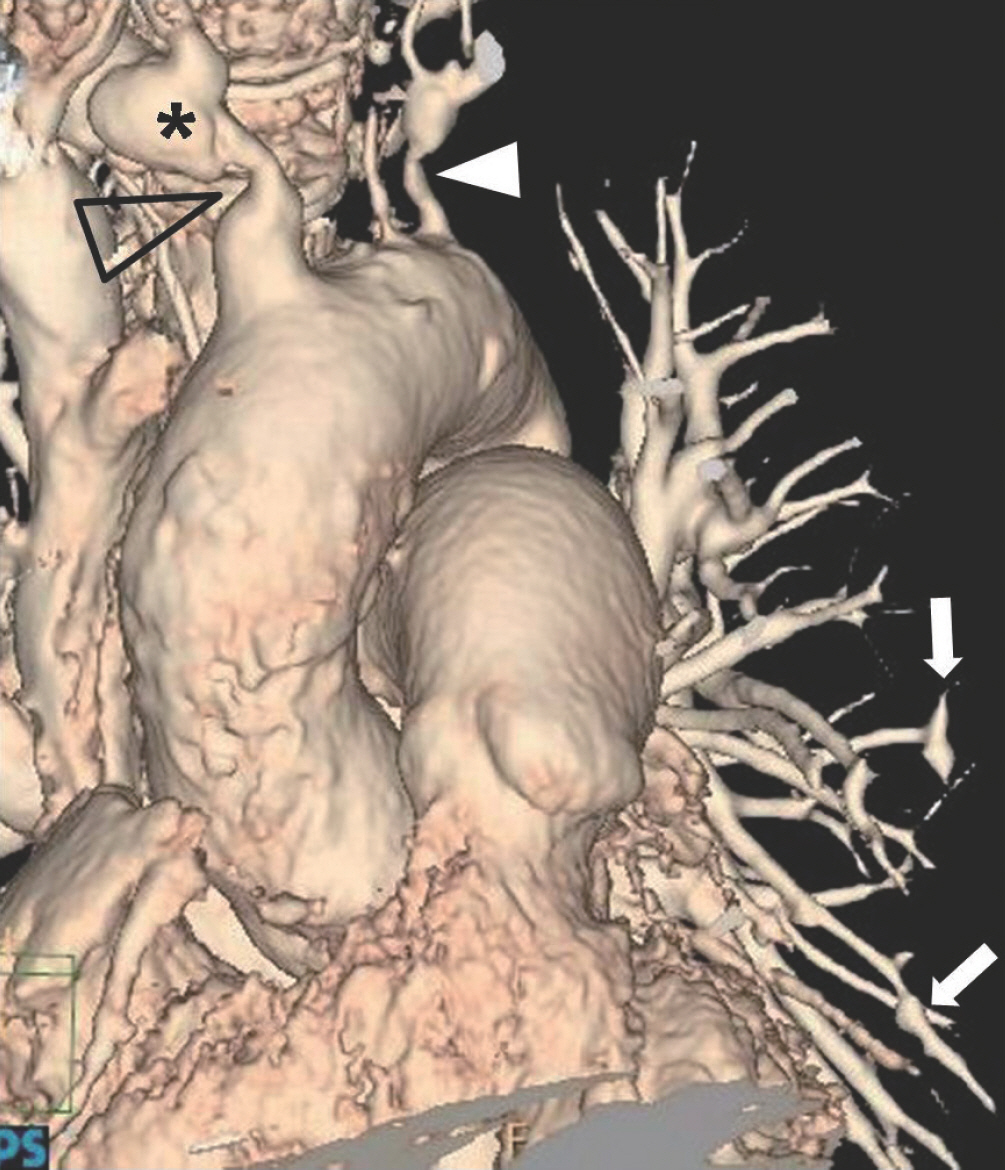
Spectrum of Multi-Detector Computed Tomography Findings that Alter Pulmonary Artery Diameters in Adults
- Affiliations
-
- 1Department of Radiology, Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea. ytokim@schmc.ac.kr
- KMID: 2412357
- DOI: http://doi.org/10.3348/jksr.2018.78.6.389
Abstract
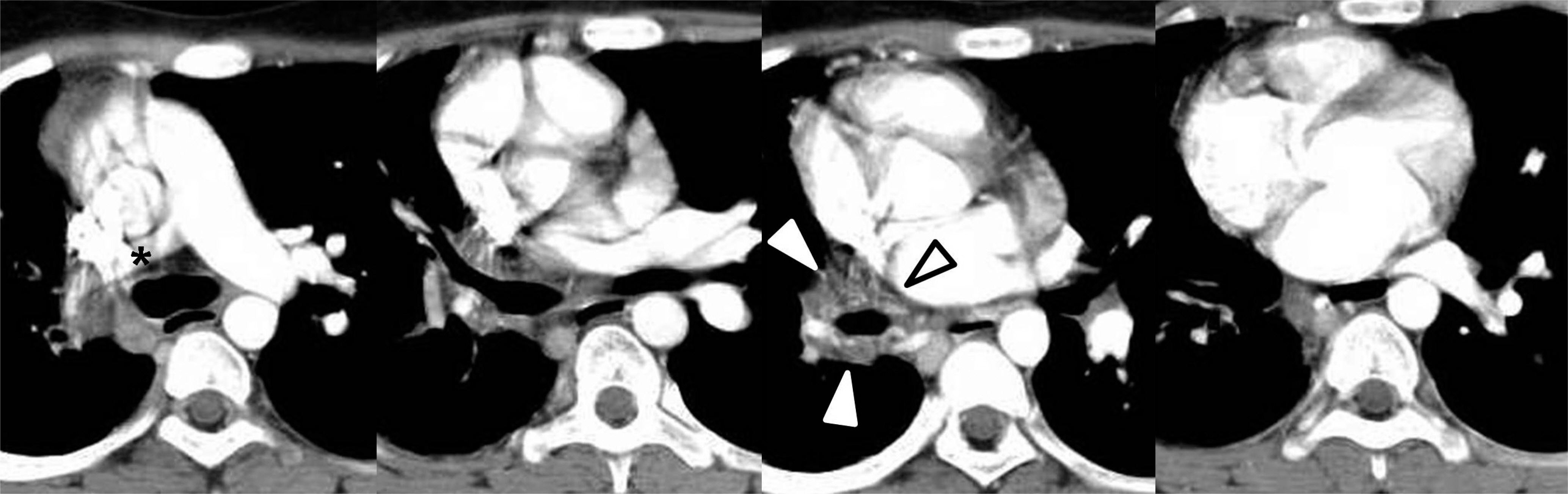
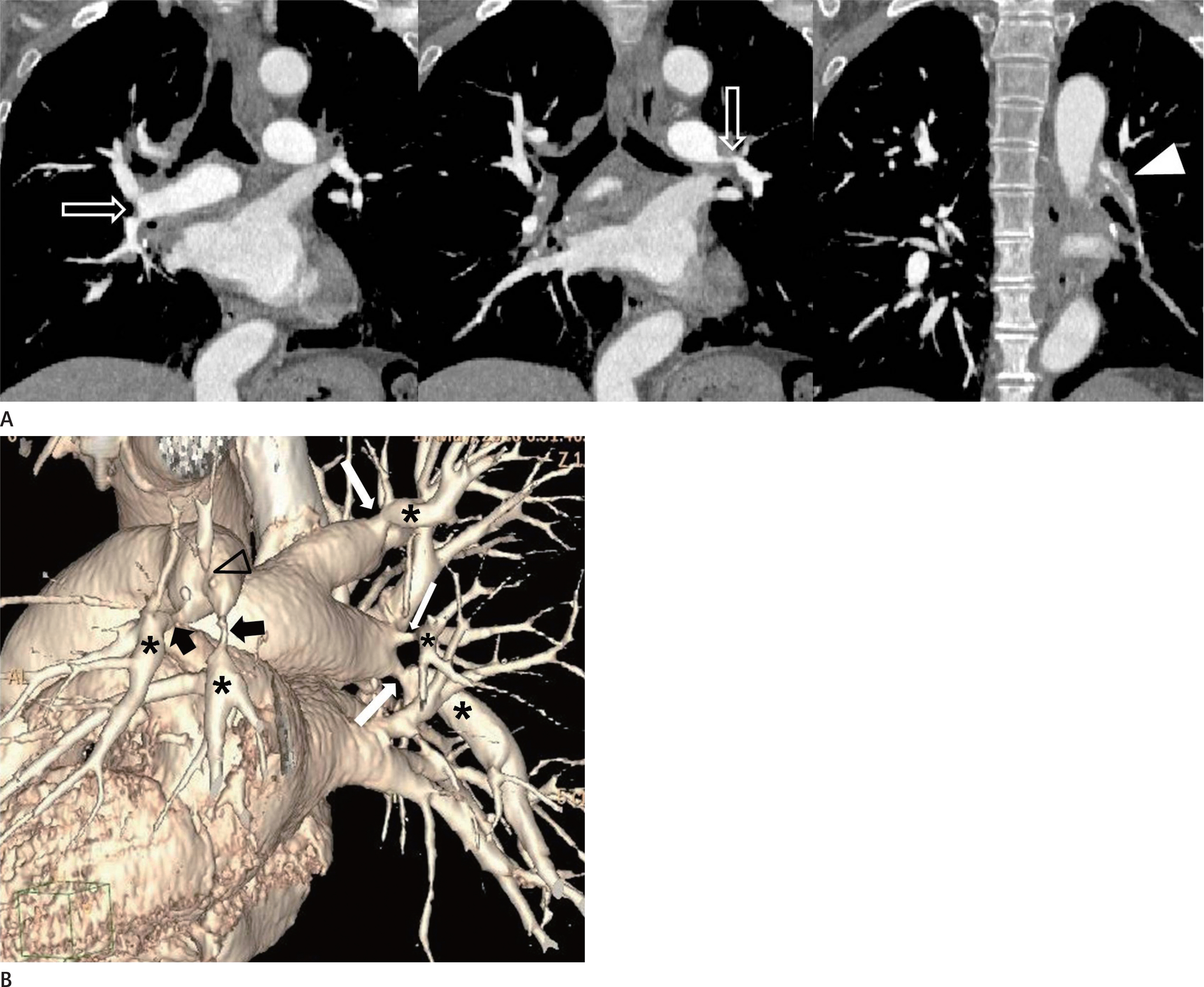
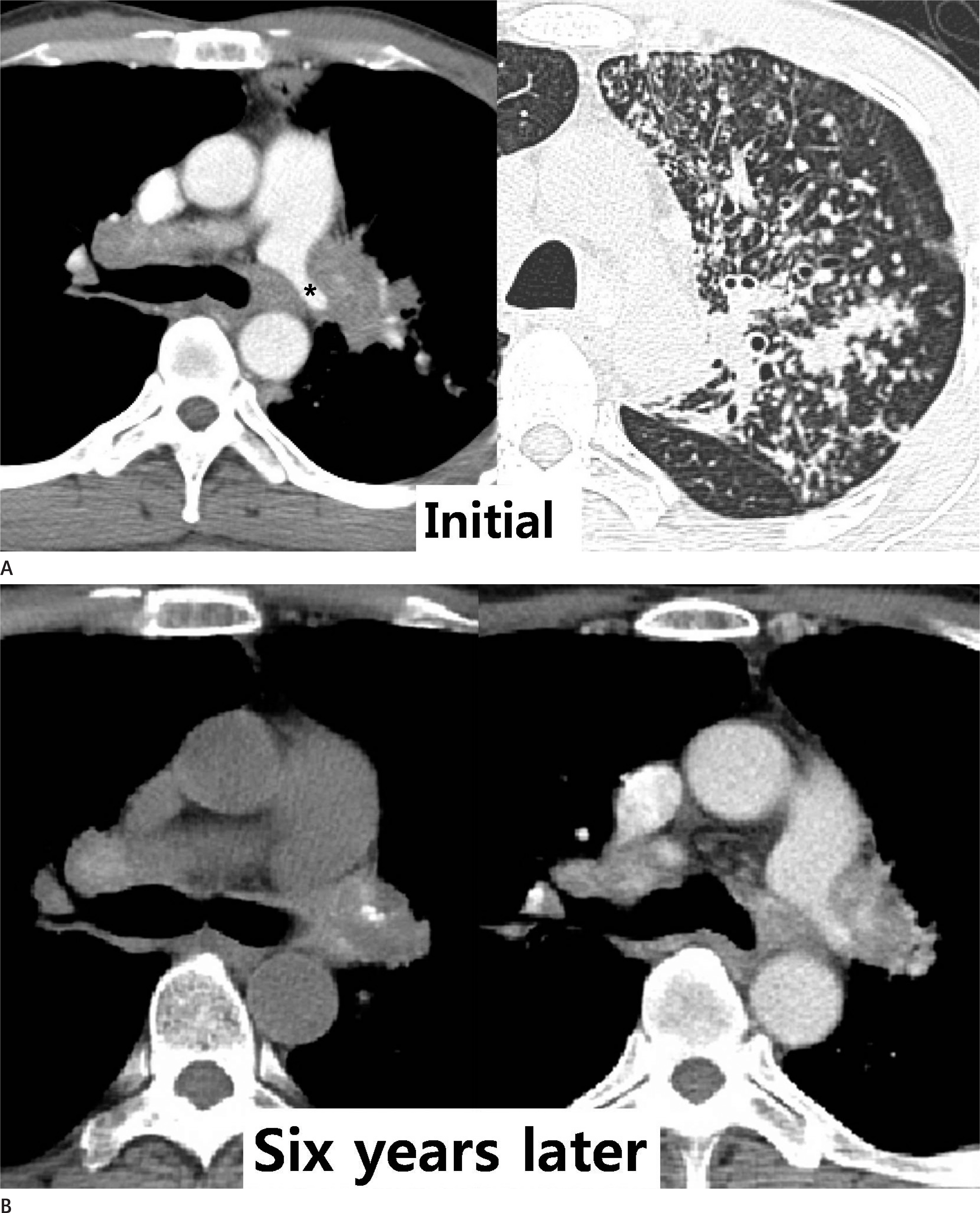
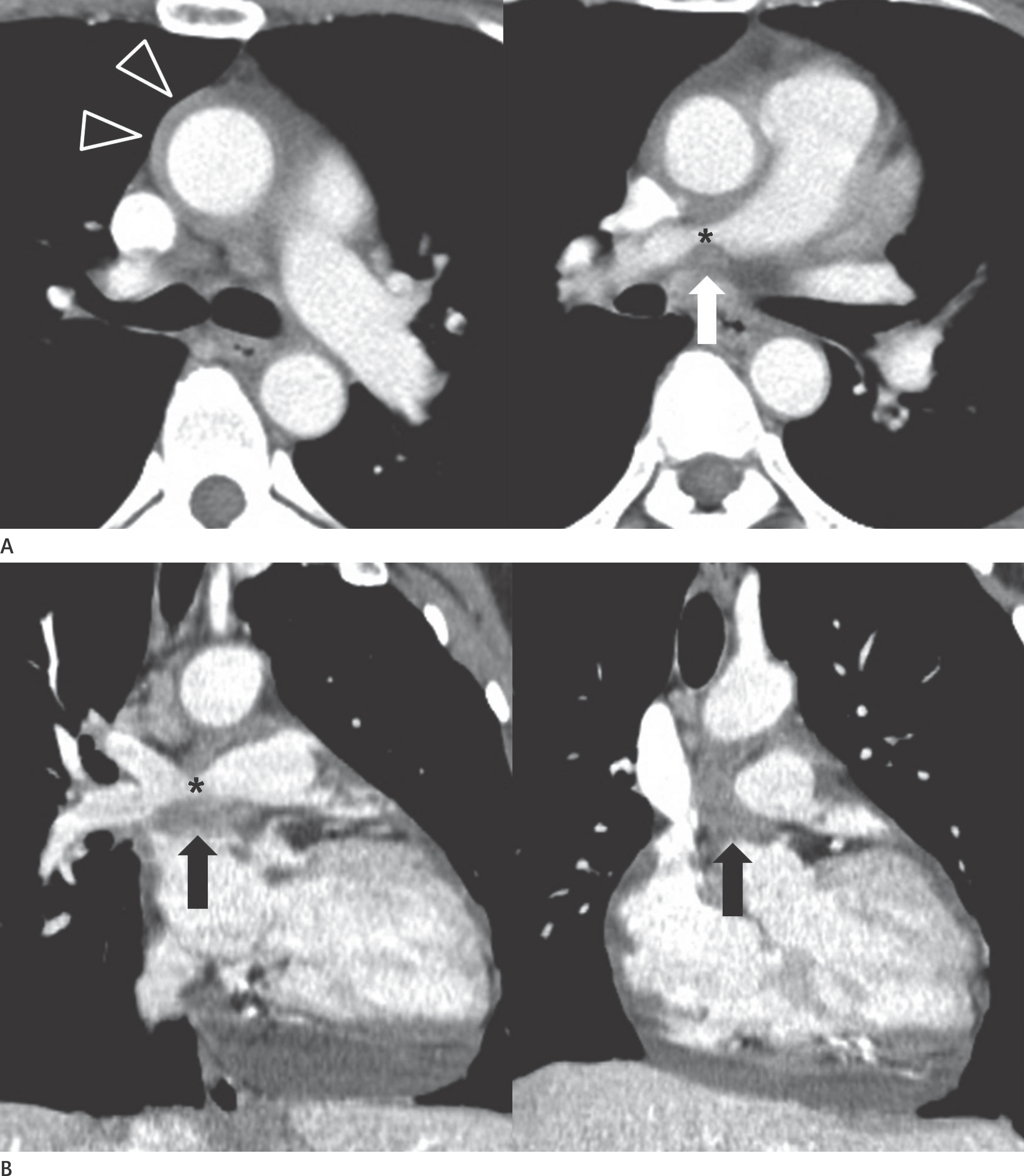
- Abnormalities in the anatomy of pulmonary arteries may have heritable or environmental causes and involve a reduction or enlargement in transverse diameters of the blood vessels eg, congenital and developmental disorders, acquired intrinsic causes, extrinsic compression, and constriction. Pulmonary hypertension, pulmonary artery aneurysm and pseudoaneurysm, and idiopathic dilatation can also increase the diameter of a pulmonary artery. Multi-detector computed tomography (CT) is useful to evaluate each pulmonary artery and to diagnose the conditions that alter the diameter of the pulmonary artery. It is important to be familiar with the CT features of a variety of disorders to allow for accurate diagnoses and appropriate therapeutic management.
MeSH Terms
Figure
Reference
-
References
1. Edwards PD, Bull RK, Coulden R. CT measurement of main pulmonary artery diameter. Br J Radiol. 1998; 71:1018–1020.
Article2. Kuriyama K, Gamsu G, Stern RG, Cann CE, Herfkens RJ, Brundage BH. CT-determined pulmonary artery diameters in predicting pulmonary hypertension. Invest Radiol. 1984; 19:16–22.
Article3. Truong QA, Massaro JM, Rogers IS, Mahabadi AA, Kriegel MF, Fox CS, et al. Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham Heart Study. Circ Cardiovasc Imaging. 2012; 5:147–154.4. Castañer E, Gallardo X, Rimola J, Pallardó Y, Mata JM, Per-endreu J, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. Radiographics. 2006; 26:349–371.
Article5. Schoepf UJ, Costello P. CT angiography for diagnosis of pulmonary embolism: state of the art. Radiology. 2004; 230:329–337.
Article6. Jones SE, Wittram C. The indeterminate CT pulmonary angiogram: imaging characteristics and patient clinical outcome. Radiology. 2005; 237:329–337.
Article7. Wittram C. How i do it: CT pulmonary angiography. AJR Am J Roentgenol. 2007; 188:1255–1261.
Article8. Mayo J, Thakur Y. Pulmonary CT angiography as first-line imaging for PE: image quality and radiation dose considerations. AJR Am J Roentgenol. 2013; 200:522–528.
Article9. Seymour J, Emanuel R, Pattinson N. Acquired pulmonary stenosis. Br Heart J. 1968; 30:776–785.
Article10. Do KH, Goo JM, Im JG, Kim KW, Chung JW, Park JH. Systemic arterial supply to the lungs in adults: spiral CT findings. Radiographics. 2001; 21:387–402.
Article11. Davies M, Guest PJ. Developmental abnormalities of the great vessels of the thorax and their embryological basis. Br J Radiol. 2003; 76:491–502.
Article12. Hislop A. Developmental biology of the pulmonary circulation. Paediatr Respir Rev. 2005; 6:35–43.
Article13. Anand SH, Jasper A, Mani SE, Joseph E, Mathai J. Proximal interruption of the pulmonary artery: a case series. J Clin Diagn Res. 2015; 9:TD04–TD06.
Article14. Ryu DS, Spirn PW, Trotman-Dickenson B, Hunsaker A, Jung SM, Park MS, et al. HRCT findings of proximal interruption of the right pulmonary artery. J Thorac Imaging. 2004; 19:171–175.
Article15. Choe YH, Ko JK, Lee HJ, Kang IS, Park PW, Lee YT. MR imaging of non-visualized pulmonary arteries at angiography in patients with congenital heart disease. J Korean Med Sci. 1998; 13:597–602.
Article16. Sondheimer HM, Oliphant M, Schneider B, Kavey RE, Blackman MS, Parker FB Jr. Computerized axial tomography of the chest for visualization of “absent” pulmonary arteries. Circulation. 1982; 65:1020–1025.
Article17. Franch RH, Gay BB Jr. Congenital stenosis of the pulmonary artery branches. a classification, with postmortem findings in two cases. Am J Med. 1963; 35:512–529.18. Baum D, Khoury GH, Ongley PA, Swan HJ, Kincaid OW. Congenital stenosis of the pulmonary artery branches. Circulation. 1964; 29:680–687.
Article19. Isawa T, Taplin GV. Unilateral pulmonary artery agenesis, stenosis, and hypoplasia. Radiology. 1971; 99:605–612.
Article20. Stovin PG. Early lung development. Thorax. 1985; 40:401–404.
Article21. Park S, Cha YK, Kim JS, Kwon JH, Jeong YJ, Kim SJ. Isolated unilateral pulmonary artery hypoplasia with accompanying pulmonary parenchymal findings on CT: a case report. J Korean Soc Radiol. 2017; 76:369–373.
Article22. Dixit R, Kumar J, Chowdhury V, Rajeshwari K, Sethi GR. Case report: isolated unilateral pulmonary vein atresia diagnosed on 128-slice multidetector CT. Indian J Radiol Imaging. 2011; 21:253–256.
Article23. Moore AD, Godwin JD, Dietrich PA, Verschakelen JA, Henderson WR Jr. Swyer-James syndrome: CT findings in eight patients. AJR Am J Roentgenol. 1992; 158:1211–1215.
Article24. Castañer E, Gallardo X, Ballesteros E, Andreu M, Pallardó Y, Mata JM, et al. CT diagnosis of chronic pulmonary thromboembolism. Radiographics. 2009; 29:31–50. ; discussion 50–53.
Article25. Moser KM, Olson LK, Schlusselberg M, Daily PO, Dembitsky WP. Chronic thromboembolic occlusion in the adult can mimic pulmonary artery agenesis. Chest. 1989; 95:503–508.
Article26. Castañer E, Alguersuari A, Gallardo X, Andreu M, Pallardó Y, Mata JM, et al. When to suspect pulmonary vasculitis: radiologic and clinical clues. Radiographics. 2010; 30:33–53.
Article27. Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR. Fibrosing mediastinitis. Radiographics. 2001; 21:737–757.
Article28. Friedman MJ, Gabor GE, Fishman MC, Griepp RB. Bilateral pulmonary artery stenosis associated with pericarditis. results of surgery and follow-up by magnetic resonance imaging. Chest. 1988; 93:883–885.29. Hwang YJ, Park CH, Jeon YB, Park KY. Severe pulmonary artery stenosis by a calcified pericardial ring. Eur J Cardiothorac Surg. 2006; 29:619–621.
Article30. Nguyen ET, Silva CI, Seely JM, Chong S, Lee KS, Müller NL. Pulmonary artery aneurysms and pseudoaneurysms in adults: findings at CT and radiography. AJR Am J Roentgenol. 2007; 188:W126–W134.
Article31. Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013; 62(25 Suppl):): D34-D41.
Article32. Grosse C, Grosse A. CT findings in diseases associated with pulmonary hypertension: a current review. Radiographics. 2010; 30:1753–1777.
Article33. Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999; 14:270–278.
Article34. Lang IM, Madani M. Update on chronic thromboembolic pulmonary hypertension. Circulation. 2014; 130:508–518.
Article35. Saremi F, Gera A, Ho SY, Hijazi ZM, Sánchez-Quintana D. CT and MR imaging of the pulmonary valve. Radiographics. 2014; 34:51–71.
Article36. Ramachandran L, Dewan S, Kumar V, Wankhade B. Mucormycosis causing pulmonary artery aneurysm. Respir Med Case Rep. 2015; 16:71–73.
Article37. Ugolini P, Mousseaux E, Sadou Y, Sidi D, Mercier LA, Paquet E, et al. Idiopathic dilatation of the pulmonary artery: report of four cases. Magn Reson Imaging. 1999; 17:933–937.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Measurements of thoracic aorta and pulmonary artery diameter by computed tomography in normal Korean adults
- Three cases of right coronary anomaly confirmed by multi-detector computed tomography
- Overlooked or unrecognized pitfalls in noninvasive multi-detector computed tomography coronary angiography
- Multi-Detector CT Findings of Typical and Atypical Appendicitis: A Pictorial Essay
- MDCT Application in the Vascular System