Clin Orthop Surg.
2016 Dec;8(4):399-406. 10.4055/cios.2016.8.4.399.
Comparison between Radiological and Clinical Outcomes of Laminoplasties with Titanium Miniplates for Cervical Myelopathy
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. jsahn@cnu.ac.kr
- KMID: 2412322
- DOI: http://doi.org/10.4055/cios.2016.8.4.399
Abstract
- BACKGROUND
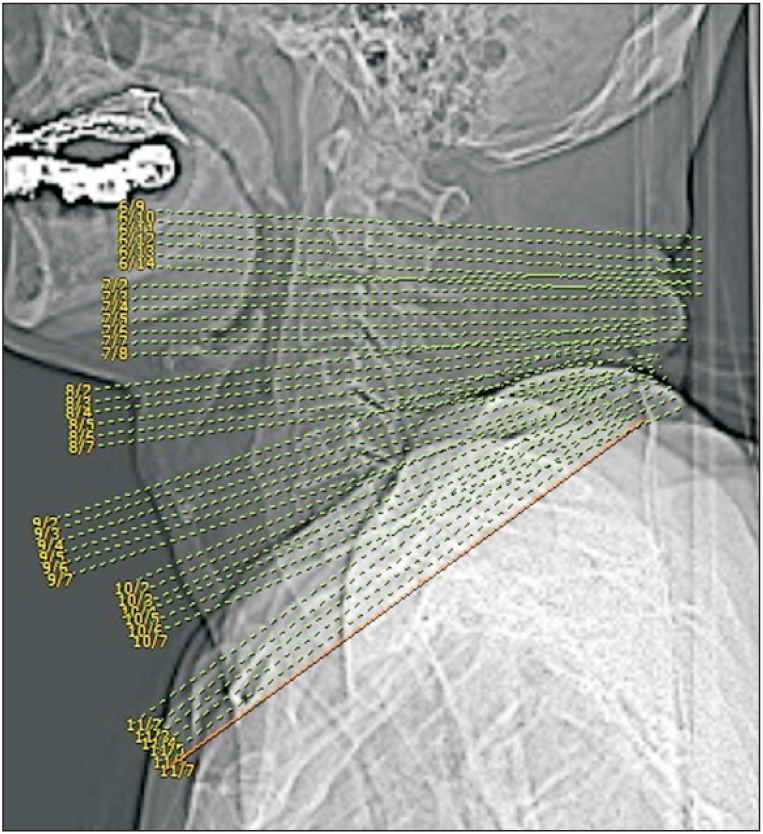
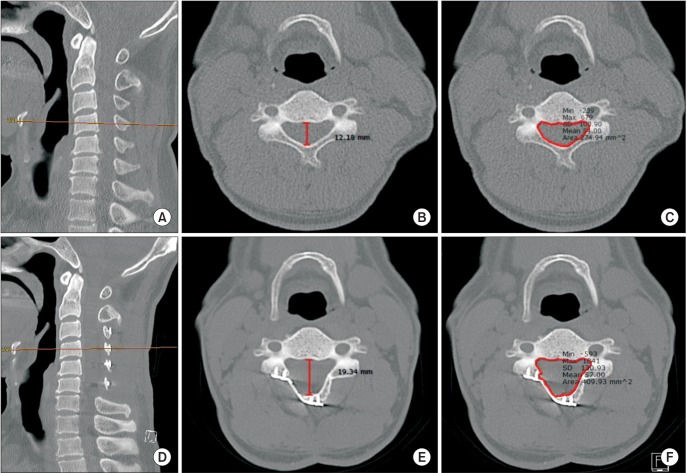
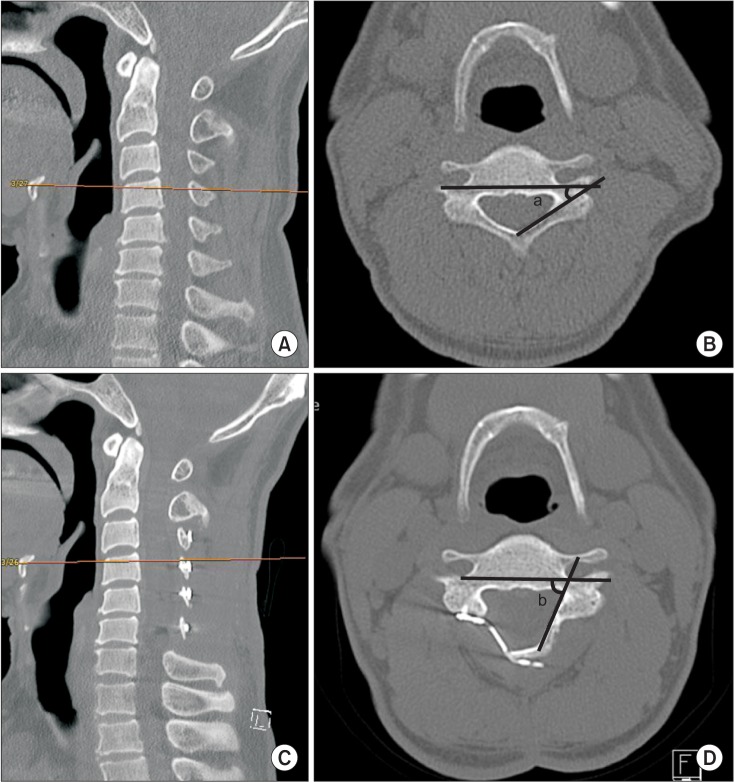
Laminoplasty is a surgical procedure frequently performed for cervical myelopathy. We investigated correlations between changes in the anteroposterior diameter (APD) of the spinal canal, spinal canal area (SCA), and laminar angle (LA) and clinical outcomes of laminoplasty.
METHODS
Of the 204 cervical myelopathy patients who underwent laminoplasty from July 2010 to May 2015, 49 patients who were evaluated with pre- and postoperative computed tomography of the cervical vertebrae were included. The average age of the patients was 60.4 years (range, 31 to 82 years), and the average duration of follow-up was 31.6 months (range, 9 to 68 months). Changes in the APD and SCA were measured at the middle of the vertebral body. Changes in LA were measured where both pedicles were clearly visible. Clinical outcomes were assessed using the Japanese Orthopaedic Association (JOA) score and visual analog scale score for pain preoperatively (1 day before surgery) and postoperatively (last outpatient visit) and examining postoperative complications.
RESULTS
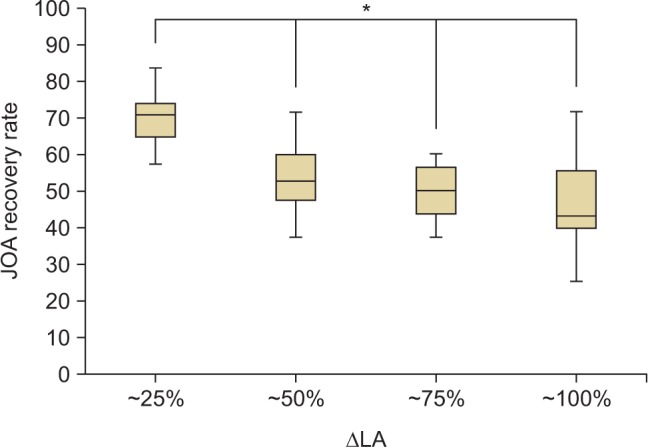
The APD showed an average of 54.7% increase from 11.5 to 17.8 mm. The SCA showed an average of 57.7% increase from 225.9 to 356.3 mm². The LA increased from 34.2° preoperatively to 71.9° postoperatively. The JOA score increased from an average of 9.1 preoperatively to 13.4 postoperatively. Three patients were found to have hinge fractures during surgery. Postoperative complications, including two cases of C5 palsy, were recorded. The correlation coefficient between the LA change and JOA score improvement was −0.449 (p < 0.05). Patients with a < 33° (25%) increase in the LA showed the most significant clinical improvement.
CONCLUSIONS
Patients with a < 33° (25%) change in the LA after laminoplasty with a titanium miniplate showed the most significant clinical improvement. Thus, LA changes can be useful in predicting the clinical outcome of laminoplasty.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Analysis of Variance
Bone Plates/adverse effects/*statistics & numerical data
Cervical Vertebrae/diagnostic imaging/*surgery
Female
Humans
Laminoplasty/adverse effects/*instrumentation/methods/*statistics & numerical data
Male
Middle Aged
Postoperative Complications
Spinal Cord Diseases/diagnostic imaging/*surgery
Titanium/*therapeutic use
Tomography, X-Ray Computed
Treatment Outcome
Titanium
Figure
Reference
-
1. Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998; 80(1):19–24. PMID: 9460946.
Article2. Suzuki A, Tamai K, Terai H, et al. Clinical outcome of cervical laminoplasty and postoperative radiological change for cervical myelopathy with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2016; 5. 20. [Epub]. DOI: 10.1097/BRS.0000000000001706.
Article3. Ahn JS, Lee JK, Lee WW, Hwang JM. Changes in cervical spine range of motion after laminoplasty in cervical spondylotic myelopathy. J Korean Soc Spine Surg. 2012; 19(3):85–89.
Article4. Chen H, Liu H, Zou L, et al. Effect of Mini-plate Fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty. Clin Spine Surg. 2016; 29(6):E288–E295. PMID: 25023712.
Article5. Yeh KT, Yu TC, Chen IH, et al. Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosis. J Orthop Surg Res. 2014; 9:49. PMID: 25142174.
Article6. Lee DH, Park SA, Kim NH, et al. Laminar closure after classic Hirabayashi open-door laminoplasty. Spine (Phila Pa 1976). 2011; 36(25):E1634–E1640. PMID: 21336233.
Article7. Cho CB, Chough CK, Oh JY, Park HK, Lee KJ, Rha HK. Axial neck pain after cervical laminoplasty. J Korean Neurosurg Soc. 2010; 47(2):107–111. PMID: 20224708.
Article8. Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J. 2006; 15(9):1375–1379. PMID: 16547754.
Article9. Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine (Phila Pa 1976). 2003; 28(21):2447–2451. PMID: 14595162.10. Imagama S, Matsuyama Y, Yukawa Y, et al. C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br. 2010; 92(3):393–400. PMID: 20190311.11. Matsumoto M, Watanabe K, Tsuji T, et al. Risk factors for closure of lamina after open-door laminoplasty. J Neurosurg Spine. 2008; 9(6):530–537. PMID: 19035744.
Article12. Wang HQ, Mak KC, Samartzis D, et al. "Spring-back" closure associated with open-door cervical laminoplasty. Spine J. 2011; 11(9):832–838. PMID: 21890423.
Article13. Kurokawa R, Kim P. Cervical laminoplasty: the history and the future. Neurol Med Chir (Tokyo). 2015; 55(7):529–539. PMID: 26119898.
Article14. O'Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization: a computerized morphometric analysis. Spine (Phila Pa 1976). 1996; 21(4):474–483. PMID: 8658252.15. Rhee JM, Register B, Hamasaki T, Franklin B. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine (Phila Pa 1976). 2011; 36(1):9–14. PMID: 21192219.
Article16. Yang HL, Chen GD, Zhang HT, Wang L, Luo ZP. Opendoor laminoplasty with plate fixation at alternating levels for treatment of multilevel degenerative cervical disease. J Spinal Disord Tech. 2013; 26(1):E13–E18. PMID: 23075860.
Article17. Jiang L, Chen W, Chen Q, Xu K, Wu Q, Li F. Clinical application of a new plate fixation system in open-door laminoplasty. Orthopedics. 2012; 35(2):e225–e231. PMID: 22310411.
Article18. Chen G, Luo Z, Nalajala B, Liu T, Yang H. Expansive opendoor laminoplasty with titanium miniplate versus sutures. Orthopedics. 2012; 35(4):e543–e548. PMID: 22495857.
Article19. Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976). 2001; 26(17):1890–1894. PMID: 11568701.
Article20. Fehlings MG, Tetreault L, Nater A, et al. The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery. 2015; 77(Suppl 4):S1–S5. PMID: 26378347.21. Oyama M, Hattori S, Moriwaki N, Nitta S. A new method of cervical laminectomy. Chubu Nippon Seikeigeka Gakkai Zasshi. 1973; 16:792–794.22. Tsuji H. Laminoplasty for patients with compressive myelopathy due to so-called spinal canal stenosis in cervical and thoracic regions. Spine (Phila Pa 1976). 1982; 7(1):28–34. PMID: 7071659.
Article23. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976). 1983; 8(7):693–699. PMID: 6420895.
Article24. Hirabayashi K, Sotomi K. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine State Art Rev. 1987; 1(5):517–532.
Article25. Maezumi H. Cervical radiculopathy after the posterior decompression of the cervical cord. Ital J Orthop Traumatol. 1989; 20:324–328.26. Zhang H, Lu S, Sun T, Yadav SK. Effect of lamina open angles in expansion open-door laminoplasty on the clinical results in treating cervical spondylotic myelopathy. J Spinal Disord Tech. 2015; 28(3):89–94. PMID: 22832551.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Technique and Long-term Follow-up of Cervical Laminoplasty using Titanium Miniplates
- Modified Open-door Laminoplasty Using Hydroxyapatite Spacers and Miniplates
- Predictors of Outcome in Patients with Cervical Spondylotic Myelopathy Undergoing Unilateral Open-Door Laminoplasty
- Cervical Laminoplasty Using Titanium Miniplate
- Outcome of the Expansive Open-door Laminoplasty with Titanium Miniplate in Cervical Stenosis