Clin Orthop Surg.
2017 Jun;9(2):200-206. 10.4055/cios.2017.9.2.200.
Reverse Total Shoulder Arthroplasty: Salvage Procedure for Failed Prior Arthroplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyung Hee University College of Medicine, Seoul, Korea. shoulderrhee@hanmail.net
- 2Department of Orthopaedic Surgery, Hallym University Hangang Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2412289
- DOI: http://doi.org/10.4055/cios.2017.9.2.200
Abstract
- BACKGROUND
To evaluate the clinical outcome of revision of primary shoulder replacement by using reverse total shoulder arthroplasty (RTSA).
METHODS
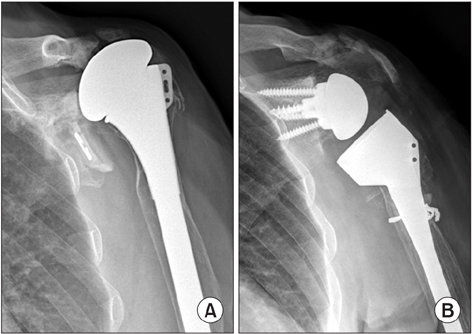
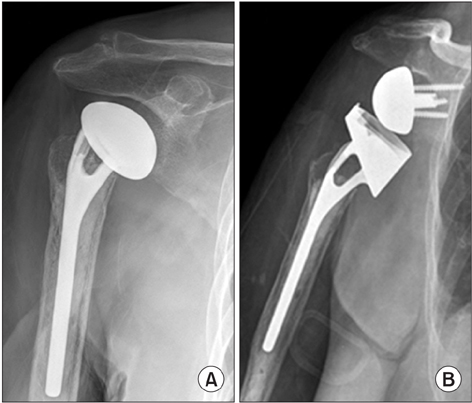
Seven patients underwent revision RTSA with a mean follow-up of 22.1 months (range, 12 to 54 months). Their mean age at the time of operation was 75.5 years (range, 70 to 80 years). Assessments were performed on the preoperative and postoperative visual analogue scale (VAS) score, muscle strength, range of motion, University of California at Los Angeles (UCLA) score, Constant score, subjective satisfaction and the anteroposterior and axillary views of the glenohumeral joint. The primary operation was hemiarthroplasty in 5 patients, total shoulder replacement in 1 patient, and reverse shoulder arthroplasty in 1 patient. The cause of revision surgery was infection in 2 patients, humeral stem loosening in 2 patients, glenoid arthropathy in 2 patients, and glenoid loosening in 1 patient. The mean duration from primary operation to revision surgery was 52 months (range, 27 to 120 months).
RESULTS
The VAS score for pain during motion was improved from 7.3 preoperatively to 2.1 postoperatively (p = 0.03). There were increases in the mean active forward flexion (from 62.1° to 92.8°), abduction (from 70° to 87.1°), external rotation (from 44.2° to 47.4°), and internal rotation (from L5 to L4; p > 0.05) postoperatively. Performance in activities of daily living improved (p > 0.05), except for lifting 10 lb above the shoulder (from 1.2 to 1.1; p = 0.434). Overall, 5 of 7 patients were satisfied with the results of revision surgery. The mean Constant score improved from 44.8 preoperatively to 57.1 postoperatively (p = 0.018). The mean UCLA score improved from 12.8 preoperatively to 22.8 postoperatively (p = 0.027). In the postoperative radiological evaluation, no radiolucency was observed around the base plate or humeral stem.
CONCLUSIONS
Pain could be reduced after revision RTSA, but improvements in range of motion and function were difficult to achieve. We think that the patients' satisfaction was relatively high despite the low function score due to the preoperative severe pain and marked limitation of range of motion.
Keyword
MeSH Terms
Figure
Reference
-
1. Sassoon AA, Rhee PC, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the nontraumatic shoulder. J Shoulder Elbow Surg. 2012; 21(11):1484–1491.
Article2. Hattrup SJ. Revision total shoulder arthroplasty for painful humeral head replacement with glenoid arthrosis. J Shoulder Elbow Surg. 2009; 18(2):220–224.
Article3. Sperling JW, Cofield RH. Revision total shoulder arthroplasty for the treatment of glenoid arthrosis. J Bone Joint Surg Am. 1998; 80(6):860–867.
Article4. Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg. 2004; 13(6):599–603.
Article5. Dines JS, Fealy S, Strauss EJ, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006; 88(7):1494–1500.
Article6. Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011; 20(1):146–157.
Article7. Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485.8. Austin L, Zmistowski B, Chang ES, Williams GR Jr. Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty? Clin Orthop Relat Res. 2011; 469(9):2531–2537.
Article9. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure: midterm results. Int Orthop. 2011; 35(1):53–60.
Article10. Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(11):1478–1483.
Article11. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; (214):160–164.
Article12. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986; 68(8):1136–1144.
Article13. Sperling JW, Cofield RH, O'Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000; 9(6):507–513.
Article14. Lazarus MD, Jensen KL, Southworth C, Matsen FA 3rd. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002; 84(7):1174–1182.
Article15. Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010; 19(8):1115–1120.
Article16. Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011; 93(24):2249–2254.
Article17. Cil A, Veillette CJ, Sanchez-Sotelo J, Sperling JW, Schleck C, Cofield RH. Revision of the humeral component for aseptic loosening in arthroplasty of the shoulder. J Bone Joint Surg Br. 2009; 91(1):75–81.
Article18. Dimmen S, Madsen JE. Long-term outcome of shoulder arthrodesis performed with plate fixation: 18 patients examined after 3-15 years. Acta Orthop. 2007; 78(6):827–833.
Article19. Maynou C, Menager S, Senneville E, Bocquet D, Mestdagh H. Clinical results of resection arthroplasty for infected shoulder arthroplasty. Rev Chir Orthop Reparatrice Appar Mot. 2006; 92(6):567–574.20. Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(4):514–522.
Article21. Kelly JD 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012; 21(11):1516–1525.
Article22. Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007; 89(2):189–195.
Article23. Ortmaier R, Resch H, Matis N, et al. Reverse shoulder arthroplasty in revision of failed shoulder arthroplasty-outcome and follow-up. Int Orthop. 2013; 37(1):67–75.
Article24. Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015; 39(2):299–304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Musculocutaneous Nerve Palsy after the Reverse Total Shoulder Arthroplasty
- Reverse Total Shoulder Arthroplasty: Techniques and Pitfalls
- Acromion Fracture after Reverse Total Shoulder Arthroplasty
- Recent Updates Regarding Outcomes and Complications of Reverse Total Shoulder Arthroplasty
- The Primary Reverse Total Shoulder Arthroplasty for Post-septic Destroyed Shoulder: A Case Report