Clin Orthop Surg.
2017 Sep;9(3):270-279. 10.4055/cios.2017.9.3.270.
Comparison of Poly-L-Lactic Acid and Poly-L-Lactic Acid/Hydroxyapatite Bioabsorbable Screws for Tibial Fixation in ACL Reconstruction: Clinical and Magnetic Resonance Imaging Results
- Affiliations
-
- 1Department of Orthopedic Surgery, Konkuk University Medical Center, Seoul, Korea. boram107@hanmail.net
- 2Department of Orthopedic Surgery, Hanil General Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Inje University Seoul Paik Hospital, Seoul, Korea.
- 4Department of Orthopedic Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2412262
- DOI: http://doi.org/10.4055/cios.2017.9.3.270
Abstract
- BACKGROUND
The purpose of this study was to compare the clinical and radiological results of 2 different tibial fixations performed using bioabsorbable screws with added hydroxyapatite (HA) and pure poly-L-lactic acid (PLLA) screws in anterior cruciate ligament (ACL) reconstruction.
METHODS
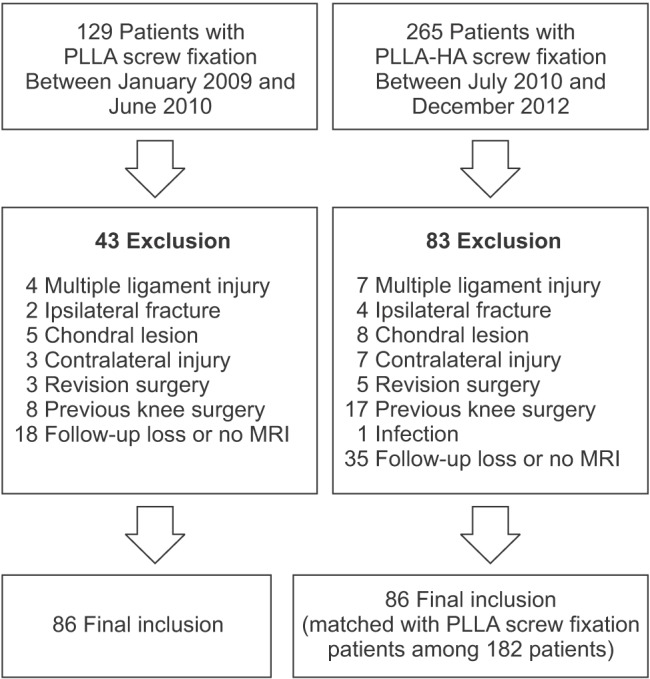
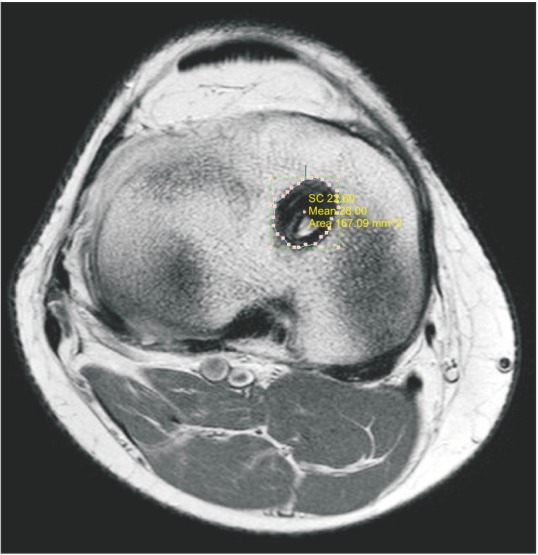
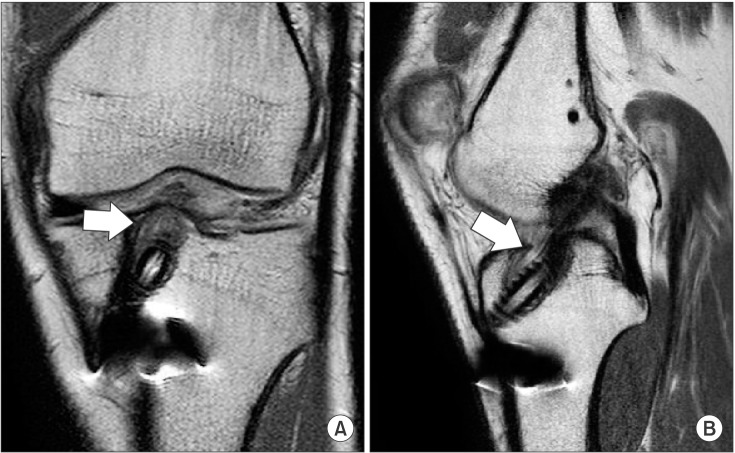
A total of 394 patients who underwent arthroscopic ACL reconstruction between March 2009 and June 2012 were retrospectively reviewed. Of those, 172 patients who took the radiological and clinical evaluations at more than 2 years after surgery were enrolled and divided into 2 groups: PLLA group (n = 86) and PLLA-HA group (n = 86). Both groups were assessed by means of the Lysholm score, International Knee Documentation Committee (IKDC) subjective knee score, and Tegner activity score. Stability was evaluated using the KT-2000 arthrometer. Magnetic resonance imaging was performed to evaluate tibial tunnel widening, screw resorption, osteoingeration, and foreign body reactions.
RESULTS
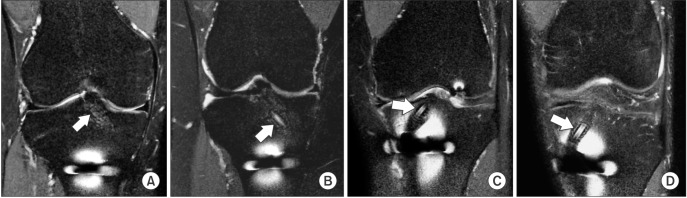
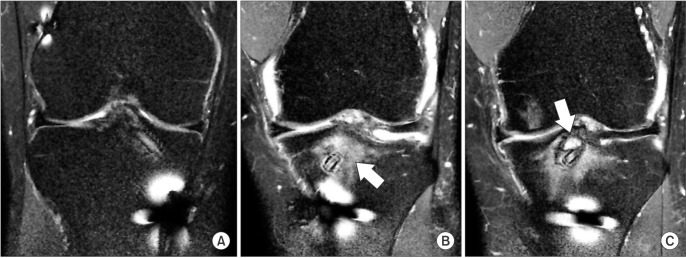
The PLLA-HA group showed significant reduction in the extent of tibial tunnel widening and foreign body reactions and significant increase in screw resorption compared to the pure PLLA group (p < 0.001 for both). In contrast, postoperative Lysholm score, Tegner activity score, IKDC score, and side-to-side difference on the KT-2000 arthrometer showed no significant differences between groups (p = 0.478, p = 0.906, p = 0.362, and p = 0.078, respectively). The PLLA group showed more significant widening in the proximal tibial tunnel than the PLLA-HA group (p = 0.001). In the correlation analysis, proximal tibial tunnel widening revealed a positive correlation with knee laxity (r = 0.866) and a negative correlation with Lysholm score (r = −0.753) (p < 0.01 for both).
CONCLUSIONS
The HA added PLLA screws would be advantageous for tibial graft fixation by reducing tibial tunnel widening, improving osteointegration, and lowering foreign body reactions. Even though no clinically significant differences were noted between the pure PLLA group and PLLA-HA group, widening of the proximal area of the tibial tunnel showed a tendency to increase knee laxity measured using the KT-2000 arthrometer.
Keyword
MeSH Terms
-
*Absorbable Implants
Adult
Anterior Cruciate Ligament/diagnostic imaging/surgery
Anterior Cruciate Ligament Injuries/diagnostic imaging/surgery
Anterior Cruciate Ligament Reconstruction/instrumentation/*methods
*Bone Screws
Durapatite/*therapeutic use
Female
Humans
Magnetic Resonance Imaging
Male
Polyesters/*therapeutic use
Retrospective Studies
Tibia/diagnostic imaging/*surgery
Polyesters
Durapatite
Figure
Reference
-
1. Vaishya R, Agarwal AK, Ingole S, Vijay V. Current trends in anterior cruciate ligament reconstruction: a review. Cureus. 2015; 7(11):e378. PMID: 26697280.
Article2. Bedi A, Maak T, Musahl V, et al. Effect of tibial tunnel position on stability of the knee after anterior cruciate ligament reconstruction: is the tibial tunnel position most important? Am J Sports Med. 2011; 39(2):366–373. PMID: 21173195.3. Van der Bracht H, Verhelst L, Stuyts B, Page B, Bellemans J, Verdonk P. Anatomic single-bundle ACL surgery: consequences of tibial tunnel diameter and drill-guide angle on tibial footprint coverage. Knee Surg Sports Traumatol Arthrosc. 2014; 22(5):1030–1039. PMID: 23370987.
Article4. Bedi A, Musahl V, Steuber V, et al. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011; 27(3):380–390. PMID: 21035990.
Article5. Coats AC, Johnson DL. Two-stage revision anterior cruciate ligament reconstruction: indications, review, and technique demonstration. Orthopedics. 2012; 35(11):958–960. PMID: 23127442.
Article6. Athanasiou KA, Agrawal CM, Barber FA, Burkhart SS. Orthopaedic applications for PLA-PGA biodegradable polymers. Arthroscopy. 1998; 14(7):726–737. PMID: 9788368.
Article7. Macarini L, Murrone M, Marini S, Mocci A, Ettorre GC. MRI in ACL reconstructive surgery with PDLLA bioabsorbable interference screws: evaluation of degradation and osteointegration processes of bioabsorbable screws. Radiol Med. 2004; 107(1-2):47–57. PMID: 15031696.8. Warden WH, Chooljian D, Jackson DW. Ten-year magnetic resonance imaging follow-up of bioabsorbable poly-L-lactic acid interference screws after anterior cruciate ligament reconstruction. Arthroscopy. 2008; 24(3):370.e1–370.e3. PMID: 18308192.
Article9. Johnston M, Morse A, Arrington J, Pliner M, Gasser S. Resorption and remodeling of hydroxyapatite-poly-L-lactic acid composite anterior cruciate ligament interference screws. Arthroscopy. 2011; 27(12):1671–1678. PMID: 21978431.
Article10. Barber FA, Dockery WD. Long-term absorption of betatricalcium phosphate poly-L-lactic acid interference screws. Arthroscopy. 2008; 24(4):441–447. PMID: 18375277.11. Macarini L, Milillo P, Mocci A, Vinci R, Ettorre GC. Poly-L-lactic acid–hydroxyapatite (PLLA-HA) bioabsorbable interference screws for tibial graft fixation in anterior cruciate ligament (ACL) reconstruction surgery: MR evaluation of osteointegration and degradation features. Radiol Med. 2008; 113(8):1185–1197. PMID: 18956150.12. Lee SR, Jang HW, Lee DW, Nam SW, Ha JK, Kim JG. Evaluation of femoral tunnel positioning using 3-dimensional computed tomography and radiographs after single bundle anterior cruciate ligament reconstruction with modified transtibial technique. Clin Orthop Surg. 2013; 5(3):188–194. PMID: 24009904.
Article13. Fules PJ, Madhav RT, Goddard RK, Newman-Sanders A, Mowbray MA. Evaluation of tibial bone tunnel enlargement using MRI scan cross-sectional area measurement after autologous hamstring tendon ACL replacement. Knee. 2003; 10(1):87–91. PMID: 12649033.
Article14. Robinson J, Huber C, Jaraj P, Colombet P, Allard M, Meyer P. Reduced bone tunnel enlargement post hamstring ACL reconstruction with poly-L-lactic acid/hydroxyapatite bioabsorbable screws. Knee. 2006; 13(2):127–131. PMID: 16352431.
Article15. Weber AE, Delos D, Oltean HN, et al. Tibial and femoral tunnel changes after ACL reconstruction: a prospective 2-year longitudinal MRI study. Am J Sports Med. 2015; 43(5):1147–1156. PMID: 25681503.16. Frosch KH, Sawallich T, Schutze G, et al. Magnetic resonance imaging analysis of the bioabsorbable Milagro interference screw for graft fixation in anterior cruciate ligament reconstruction. Strategies Trauma Limb Reconstr. 2009; 4(2):73–79. PMID: 19697105.
Article17. Lajtai G, Noszian I, Humer K, Unger F, Aitzetmuller G, Orthner E. Serial magnetic resonance imaging evaluation of operative site after fixation of patellar tendon graft with bioabsorbable interference screws in anterior cruciate ligament reconstruction. Arthroscopy. 1999; 15(7):709–718. PMID: 10524818.
Article18. Moisala AS, Jarvela T, Paakkala A, Paakkala T, Kannus P, Jarvinen M. Comparison of the bioabsorbable and metal screw fixation after ACL reconstruction with a hamstring autograft in MRI and clinical outcome: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2008; 16(12):1080–1086. PMID: 18762911.
Article19. Singhal MC, Holzhauer M, Powell D, Johnson DL. MRI evaluation of the tibial tunnel/screw/tendon interface after ACL reconstruction using a bioabsorbable interference screw. Orthopedics. 2008; 31(6):575–579. PMID: 18661880.
Article20. Lind M, Feller J, Webster KE. Tibial bone tunnel widening is reduced by polylactate/hydroxyapatite interference screws compared to metal screws after ACL reconstruction with hamstring grafts. Knee. 2009; 16(6):447–451. PMID: 19423351.
Article21. Cox CL, Spindler KP, Leonard JP, Morris BJ, Dunn WR, Reinke EK. Do newer-generation bioabsorbable screws become incorporated into bone at two years after ACL reconstruction with patellar tendon graft?: a cohort study. J Bone Joint Surg Am. 2014; 96(3):244–250. PMID: 24500587.22. Hunt JA, Callaghan JT. Polymer-hydroxyapatite composite versus polymer interference screws in anterior cruciate ligament reconstruction in a large animal model. Knee Surg Sports Traumatol Arthrosc. 2008; 16(7):655–660. PMID: 18418577.
Article23. Tamai N, Myoui A, Tomita T, et al. Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J Biomed Mater Res. 2002; 59(1):110–117. PMID: 11745543.24. Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med. 2006; 34(11):1790–1800. PMID: 16861579.25. Clatworthy MG, Annear P, Bulow JU, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc. 1999; 7(3):138–145. PMID: 10401649.
Article26. Hoher J, Moller HD, Fu FH. Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc. 1998; 6(4):231–240. PMID: 9826805.27. Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am. 2011; 93(6):572–580. PMID: 21411708.28. Weiler A, Peine R, Pashmineh-Azar A, Abel C, Sudkamp NP, Hoffmann RF. Tendon healing in a bone tunnel: Part I: biomechanical results after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002; 18(2):113–123. PMID: 11830804.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic ACL Reconstruction using Bone-patellar Tendon-bone Autograft and Bioabsorbable Interference Screw
- Management of a Visible Nodule Following Poly-L-Lactic Acid Injection in the Periorbital Area
- Biodegradable poly (lactic acid) microspheres for drug delivery systems
- Serial Magnetic Resonance Imaging Evaluation of Bioabsorbable Interference Screws in Anterior Cruciate Ligament Reconstruction
- Late Onset Foreign Body Reaction due to Poly-L-Lactic Acid Facial Injections for Cosmetic Purpose