Clin Orthop Surg.
2018 Jun;10(2):253-259. 10.4055/cios.2018.10.2.253.
Unsintered Hydroxyapatite and Poly-L-Lactide Composite Screws/Plates for Stabilizing β-Tricalcium Phosphate Bone Implants
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyoto University, Kyoto, Japan. akiosaka@kuhp.kyoto-u.ac.jp
- KMID: 2411753
- DOI: http://doi.org/10.4055/cios.2018.10.2.253
Abstract
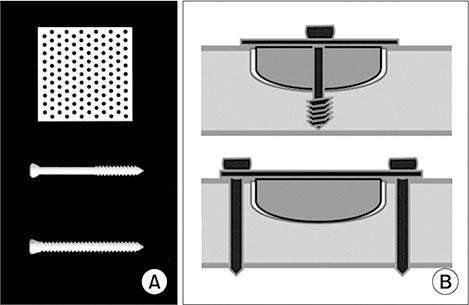
- Unsintered hydroxyapatite (u-HA) and poly-L-lactide (PLLA) composites (u-HA/PLLA) are osteoconductive and biodegradable. Screw (Super-Fixsorb MX30) and plate (Super-Fixsorb MX40 Mesh) systems made of u-HA/PLLA are typically used in small bones in maxillofacial surgeries. After the resection of bone tumors in larger bones, reconstructions with β-tricalcium phosphate (β-TCP) implants of strong compression resistance have been reported. After a resection, when the cavity is hemispheric- or concave-shaped, stabilization of the implanted β-TCP block is necessary. In the current series, u-HA/PLLA were used to stabilize the mechanically strong implanted low-porous β-TCP blocks in six bone tumor cases, including three giant cell tumors of bone, and one case each of chondroblastoma, chondrosarcoma, and parosteal osteosarcoma. The mean age of patients at the time of surgery was 31.3 years (range, 19 to 48 years). The bones involved were two ilia (posterior), a femur (diaphysis to distal metaphysis), and three tibias (proximal epiphysis, proximal metaphysis to epiphysis, and distal metaphysis to epiphysis). Neither displacement of the implanted β-TCP block nor any u-HA/PLLA-related complications were observed. The radiolucent character of the u-HA/PLLA did not hinder radiological examinations for potential signs of tumor recurrence. The method of using u-HA/PLLA components for the stabilization of β-TCP blocks makes the procedure easy to perform and reliable. It can extend the application of β-TCP blocks in reconstruction surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. O'Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am. 1994; 76(12):1827–1833.2. Sakamoto A. Reconstruction with β-tricalcium phosphate for giant cell tumor of bone around the knee. J Knee Surg. 2017; 30(1):75–77.
Article3. Sakellariou VI, Mavrogenis AF, Mazis GA, Papagelopoulos PJ. Osteosarcoma of navicular bone: en bloc excision and salvage of the foot. Foot Ankle Surg. 2012; 18(3):e29–e33.
Article4. Sakamoto M, Matsumoto T. Development and evaluation of superporous ceramics bone tissue scaffold materials with triple pore structure a) hydroxyapatite, b) beta-tricalcium phosphate. In : Tal H, editor. Bone regeneration. London: InTech;2012. p. 301–320.5. Stone JL, Beaupre GS, Hayes WC. Multiaxial strength characteristics of trabecular bone. J Biomech. 1983; 16(9):743–752.
Article6. Shikinami Y, Matsusue Y, Nakamura T. The complete process of bioresorption and bone replacement using devices made of forged composites of raw hydroxyapatite particles/poly l-lactide (F-u-HA/PLLA). Biomaterials. 2005; 26(27):5542–5551.
Article7. Ueki K, Okabe K, Marukawa K, et al. Skeletal stability after mandibular setback surgery: comparison between the hybrid technique for fixation and the conventional plate fixation using an absorbable plate and screws. J Craniomaxillofac Surg. 2014; 42(4):351–355.
Article8. Yasunaga T, Matsusue Y, Furukawa T, Shikinami Y, Okuno M, Nakamura T. Bonding behavior of ultrahigh strength unsintered hydroxyapatite particles/poly(L-lactide) composites to surface of tibial cortex in rabbits. J Biomed Mater Res. 1999; 47(3):412–419.
Article9. Furukawa T, Matsusue Y, Yasunaga T, et al. Histomorphometric study on high-strength hydroxyapatite/poly(L-lactide) composite rods for internal fixation of bone fractures. J Biomed Mater Res. 2000; 50(3):410–419.
Article10. Ng AM, Tan KK, Phang MY, et al. Differential osteogenic activity of osteoprogenitor cells on HA and TCP/HA scaffold of tissue engineered bone. J Biomed Mater Res A. 2008; 85(2):301–312.
Article11. Liu B, Lun DX. Current application of β-tricalcium phosphate composites in orthopaedics. Orthop Surg. 2012; 4(3):139–144.
Article12. Sakamoto A. Joint preserved reconstruction after curettage in giant cell tumor of bone arising in the distal radius: case report. Int J Surg Case Rep. 2015; 16:181–183.
Article13. Sakamoto A. Reconstruction with β-tricalcium phosphate after navicular tumor resection. J Foot Ankle Surg. 2017; 56(1):98–102.
Article14. Hayashi M, Muramatsu H, Sato M, Tomizuka Y, Inoue M, Yoshimoto S. Surgical treatment of facial fracture by using unsintered hydroxyapatite particles/poly l-lactide composite device (OSTEOTRANS MX(®)): a clinical study on 17 cases. J Craniomaxillofac Surg. 2013; 41(8):783–788.
Article15. Eppley BL, Morales L, Wood R, et al. Resorbable PLLA-PGA plate and screw fixation in pediatric craniofacial surgery: clinical experience in 1883 patients. Plast Reconstr Surg. 2004; 114(4):850–856.
Article16. Shikinami Y, Okuno M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA). Part I: basic characteristics. Biomaterials. 1999; 20(9):859–877.
Article17. Shikinami Y, Okuno M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly L-lactide (PLLA). Part II: practical properties of miniscrews and miniplates. Biomaterials. 2001; 22(23):3197–3211.
Article18. Sakai A, Oshige T, Zenke Y, Menuki K, Murai T, Nakamura T. Mechanical comparison of novel bioabsorbable plates with titanium plates and small-series clinical comparisons for metacarpal fractures. J Bone Joint Surg Am. 2012; 94(17):1597–1604.
Article19. Landes CA, Ballon A, Tran A, Ghanaati S, Sader R. Segmental stability in orthognathic surgery: hydroxyapatite/poly-l-lactide osteoconductive composite versus titanium miniplate osteosyntheses. J Craniomaxillofac Surg. 2014; 42(6):930–942.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital Wall Reconstruction with Osteoconductive Unsintered Hydroxyapatite/Poly L-Lactide
- Medial Wall Orbital Reconstruction using Unsintered Hydroxyapatite Particles/Poly L-Lactide Composite Implants
- In vitro and in vivo analyses of the biocompatibility of sintered TCP-HA composite screws
- Clinical courses and degradation patterns of absorbable plates in facial bone fracture patients
- Stability of maxillary position after lefort i osteotomy using biodegradable plates and screws