Clin Orthop Surg.
2018 Jun;10(2):191-196. 10.4055/cios.2018.10.2.191.
The Need for Early Tracheostomy in Patients with Traumatic Cervical Cord Injury
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonnam National University Hospital, Gwangju, Korea. osdrseo@gmail.com
- KMID: 2411744
- DOI: http://doi.org/10.4055/cios.2018.10.2.191
Abstract
- BACKGROUND
In patients who need sustained endotracheal intubation and mechanical ventilation due to respiratory failure after traumatic cervical spinal cord injury, tracheostomy can be performed to reduce the duration of mechanical ventilation and respiratory complications. The purpose of this study was to determine criteria and timing of tracheostomy in patients with severe traumatic cervical spinal cord injury accompanied by motor weakness.
METHODS
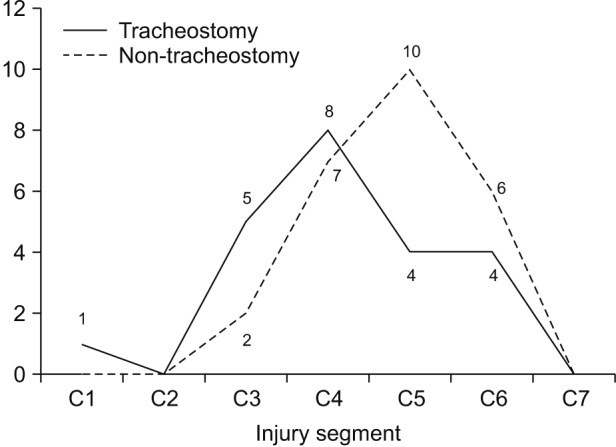
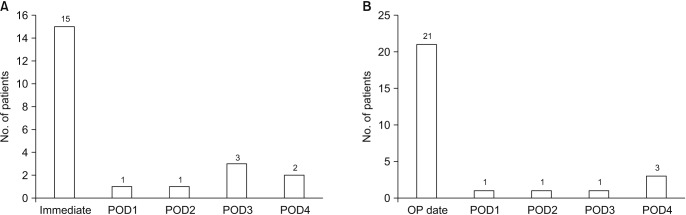
We reviewed 22 patients who underwent tracheostomy (study group) and 27 patients who did not (control group) from January 2005 to March 2016. We assessed the American Spinal Injury Association (ASIA) impairment scale score and investigated accompanying thoracic injury, paradoxical respiration, postoperative endotracheal intubation and other clinical parameters. The study group was also subdivided into the early tracheostomy group and late tracheostomy group depending on whether the tracheostomy was performed within or later than 7 days after surgery.
RESULTS
Twenty-two patients in the study group had a mean ASIA impairment scale score of 14.1 points, which was lower than the control group's 23.4 points. Paradoxical respiration was observed in 77% of the patients in the study group compared to 18% in the control group. Postoperative intubation was maintained in 68% in the study group; 32% underwent endotracheal intubation due to respiratory failure within 4 days after surgery and had a tracheostomy. In the control group, postoperative intubation was maintained in 22%, and all of them were weaned off intubation within 4 days after surgery. The duration of intensive care unit hospitalization was 11.4 days for the early tracheostomy group, which was shorter than the late tracheostomy group's 19.7 days.
CONCLUSIONS
In patients with severe traumatic cervical spinal cord injury, tracheostomy may be needed when the motor grade of the ASIA scale is low, above the C4 segment is injured, or paradoxical respiration occurs after injuries. In addition, if endotracheal extubation is not feasible within 4 days after surgery, an early tracheostomy should be considered.
MeSH Terms
Figure
Reference
-
1. Mansel JK, Norman JR. Respiratory complications and management of spinal cord injuries. Chest. 1990; 97(6):1446–1452. PMID: 2189697.
Article2. National Spinal Cord Injury Statistical Center, University of Alabama at Birmingham. 10 Annual report for the spinal cord injury model system. Birmingham, AL: National Spinal Cord Injury Statistical Center;2011.3. Nakajima A, Honda S, Yoshimura S, Ono Y, Kawamura J, Moriai N. The disease pattern and causes of death of spinal cord injured patients in Japan. Paraplegia. 1989; 27(3):163–171. PMID: 2762003.
Article4. Neumann CR, Brasil AV, Albers F. Risk factors for mortality in traumatic cervical spinal cord injury: Brazilian data. J Trauma. 2009; 67(1):67–70. PMID: 19590310.
Article5. Ball PA. Critical care of spinal cord injury. Spine (Phila Pa 1976). 2001; 26(24 Suppl):S27–S30. PMID: 11805605.
Article6. Berney S, Stockton K, Berlowitz D, Denehy L. Can early extubation and intensive physiotherapy decrease length of stay of acute quadriplegic patients in intensive care? A retrospective case control study. Physiother Res Int. 2002; 7(1):14–22. PMID: 11992981.
Article7. Brook AD, Sherman G, Malen J, Kollef MH. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care. 2000; 9(5):352–359. PMID: 10976359.
Article8. Branco BC, Plurad D, Green DJ, et al. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma. 2011; 70(1):111–115. PMID: 20526209.
Article9. Fishburn MJ, Marino RJ, Ditunno JF Jr. Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil. 1990; 71(3):197–200. PMID: 2317137.10. Goettler CE, Fugo JR, Bard MR, et al. Predicting the need for early tracheostomy: a multifactorial analysis of 992 intubated trauma patients. J Trauma. 2006; 60(5):991–996. PMID: 16688060.
Article11. Harrop JS, Sharan AD, Scheid EH Jr, Vaccaro AR, Przybylski GJ. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg. 2004; 100(1 Suppl Spine):20–23. PMID: 14748569.
Article12. Kluger Y, Paul DB, Lucke J, et al. Early tracheostomy in trauma patients. Eur J Emerg Med. 1996; 3(2):95–101. PMID: 9028753.
Article13. Palmieri TL, Jackson W, Greenhalgh DG. Benefits of early tracheostomy in severely burned children. Crit Care Med. 2002; 30(4):922–924. PMID: 11940771.
Article14. Northrup BE, Vaccaro AR, Rosen JE, Balderston RA, Cotler JM. Occurrence of infection in anterior cervical fusion for spinal cord injury after tracheostomy. Spine (Phila Pa 1976). 1995; 20(22):2449–2453. PMID: 8578397.
Article15. Milanchi S, Magner D, Wilson MT, Mirocha J, Margulies DR. Percutaneous tracheostomy in neurosurgical patients with intracranial pressure monitoring is safe. J Trauma. 2008; 65(1):73–79. PMID: 18580518.
Article16. Berlly M, Shem K. Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med. 2007; 30(4):309–318. PMID: 17853652.
Article17. Arabi YM, Alhashemi JA, Tamim HM, et al. The impact of time to tracheostomy on mechanical ventilation duration, length of stay, and mortality in intensive care unit patients. J Crit Care. 2009; 24(3):435–440. PMID: 19327302.
Article18. Epstein SK. Late complications of tracheostomy. Respir Care. 2005; 50(4):542–549. PMID: 15807919.19. Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy: a prospective study of 150 critically ill adult patients. Am J Med. 1981; 70(1):65–76. PMID: 7457492.
Article20. De Leyn P, Bedert L, Delcroix M, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007; 32(3):412–421. PMID: 17588767.
Article21. Stemmer EA, Oliver C, Carey JP, Connolly JE. Fatal complications of tracheotomy. Am J Surg. 1976; 131(3):288–290. PMID: 769582.
Article22. Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984; 94(3):367–377. PMID: 6700353.
Article23. Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg. 2000; 123(4):495–500. PMID: 11020193.
Article24. Esteller More E, Ibanez-Nolla J, Garcia-Hernandez F, et al. Post-mortem study of laryngotracheal lesions produced by prolonged intubation and/or tracheotomy. Acta Otorrinolaringol Esp. 1997; 48(7):545–550. PMID: 9489156.25. Esteller-More E, Ibanez J, Matino E, Adema JM, Nolla M, Quer IM. Prognostic factors in laryngotracheal injury following intubation and/or tracheotomy in ICU patients. Eur Arch Otorhinolaryngol. 2005; 262(11):880–883. PMID: 16258758.
Article26. Cosortium for Spinal Cord Medicine. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005; 28(3):259–293. PMID: 16048145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Early Tracheostomy on Hospital-Acquired Pneumonia and Infection of Anterior Cervical Fusion Site in Patients with Acute Cervical Cord Injury
- A Nomogram Model for Prediction of Tracheostomy in Patients With Traumatic Cervical Spinal Cord Injury
- The Effectiveness of Early Tracheostomy (within at least 10 Days) in Cervical Spinal Cord Injury Patients
- Predictive Values of Magnetic Resonance Imaging Features for Tracheostomy in Traumatic Cervical Spinal Cord Injury
- The Effects of Tracheostomy for the Functional Outcomes of Severe Traumatic Brain Injury Patients