J Korean Ophthalmol Soc.
2018 May;59(5):491-495. 10.3341/jkos.2018.59.5.491.
A Case of Spontaneous Recovery of an Iris Cyst in a Patient with Peritoneal Tuberculosis
- Affiliations
-
- 1Department of Ophthalmology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. coolleo7@naver.com
- KMID: 2411460
- DOI: http://doi.org/10.3341/jkos.2018.59.5.491
Abstract
- PURPOSE
We report a case of spontaneous recovery of an iris cyst with only tuberculosis medication and conservative eye drops when uveitis and angle closure occurred because of a cyst in a patient with peritoneal tuberculosis.
CASE SUMMARY
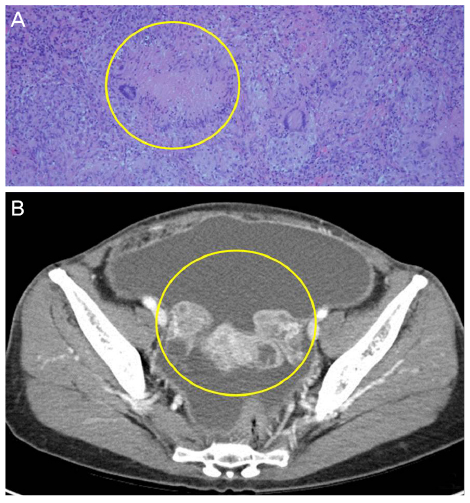
A 49-year-old female who was diagnosed with iritis and treated with steroid eye drops visited our clinic because of decreased visual acuity 1 month prior. There were anterior chamber inflammation cells and an iris cyst completely obstructing the anterior chamber at 12 o'clock. At the time, the patient had been diagnosed with peritoneal tuberculosis in the Department of Internal Medicine and Gynecology and had been treated with surgery and medication. The patient had no past history of glaucoma, but when the iris cyst developed, the intraocular pressure increased to 29 mmHg and anterior inflammatory cells were seen in the range of +1 to +2. The primary lesion of tuberculosis improved and the iris cyst disappeared with treatments involving medication for tuberculosis, steroid eye drops, and glaucoma eye drops, without invasive treatments such as alcohol curettage, laser treatment, or cyst resection.
CONCLUSIONS
If an iris cyst is a new lesion of the eye, it is necessary to identify the pattern and cause of the iris cyst first, and if a secondary benign iris cyst is suspected, the primary treatment of the causative disease is necessary rather than prompt invasive treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Shields CL, Kancherla S, Patel J, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology. 2012; 119:407–414.
Article2. Shields JA. Primary cysts of the iris. Trans Am Ophthalmol Soc. 1981; 79:771–809.3. Shields JA, Shields CL, Lois N, Mercado G. Iris cysts in children: classification, incidence, and management. Br J Ophthalmol. 1999; 83:334–338.4. Lois N, Shields CL, Shields JA, Mercado G. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology. 1998; 105:1879–1885.5. Shields JA, Klinc MW, Augsburger JJ. Primary iris cyst: a review of the literature and report of 62 cases. Br J Ophthalmol. 1984; 68:152–166.6. Saricaoğlu MS, Sengun A, Guven D, Karakurt A. Ocular tuberculosis with angle granuloma. Eye (Lond). 2004; 18:219–220.
Article7. Thompson MJ, Albert DM. Ocular tuberculosis. Arch Ophthalmol. 2005; 123:844–849.
Article8. Yeh S, Sen HN, Colyer M, et al. Update on ocular tuberculosis. Curr Opin Ophthalmol. 2012; 23:551–556.
Article9. Shin JH, Park HY, Cho SJ. Free-floating pigmented iris cyst in the anterior chamber. J Korean Ophthalmol Soc. 2008; 49:1862–1866.
Article10. Hulke JW. Report on cases of cysts of the iris. Roy Lond Ophth Hosp Rep. 1869; 6:12.11. Lee SS, Yoo SJ, Kim BY. Laser treatment for recurrent secondary iris cyst. J Korean Ophthalmol Soc. 2004; 45:146–151.12. Shields CL, Arepalli S, Lally EB, et al. Iris stromal cyst management with absolute alcohol-induced sclerosis in 16 patients. JAMA Ophthalmol. 2014; 132:703–708.
Article13. Wiwatwongwana A, Ittipunkul N, Wiwatwongwana D. Ab externo laser photocoagulation for the treatment of spontaneous iris stromal cyst. Graefes Arch Clin Exp Ophthalmol. 2012; 250:155–156.
Article14. Bodaghi B, LeHoang P. Ocular tuberculosis. Curr Opin Ophthalmol. 2000; 11:443–448.
Article15. Sheu SJ, Shyu JS, Chen LM, et al. Ocular manifestations of tuberculosis. Ophthalmology. 2001; 108:1580–1585.
Article16. Rosen PH, Spalton DJ, Graham EM. Intraocular tuberculosis. Eye (Lond). 1990; 4:486–492.
Article17. Biswas J, Madhavan HN, Gopal L, Badrinath SS. Intraocular tuberculosis. Clinicopathologic study of five cases. Retina. 1995; 15:461–468.18. Alvarez GG, Roth VR, Hodge W. Ocular tuberculosis: diagnostic and treatment challenges. Int J Infect Dis. 2009; 13:432–435.
Article