Cancer Res Treat.
2018 Apr;50(2):324-334. 10.4143/crt.2016.544.
A National Study of Survival Trends and Conditional Survival in Nasopharyngeal Carcinoma: Analysis of the National Population-Based Surveillance Epidemiology and End Results Registry
- Affiliations
-
- 1Department of Radiation Oncology, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China. sunying@sysucc.org.cn
- 2Department of Medical Statistics and Epidemiology, School of Public Health, Sun Yat-sen University, Guangzhou, China.
- KMID: 2411122
- DOI: http://doi.org/10.4143/crt.2016.544
Abstract
- PURPOSE
Conditional survival (CS) provides important information on survival for a period of time after diagnosis. Currently, information on CS patterns of patients with nasopharyngeal carcinoma (NPC) is lacking. We aimed to analyze survival rate over time and estimate CS for NPC patients using a national population-based registry.
MATERIALS AND METHODS
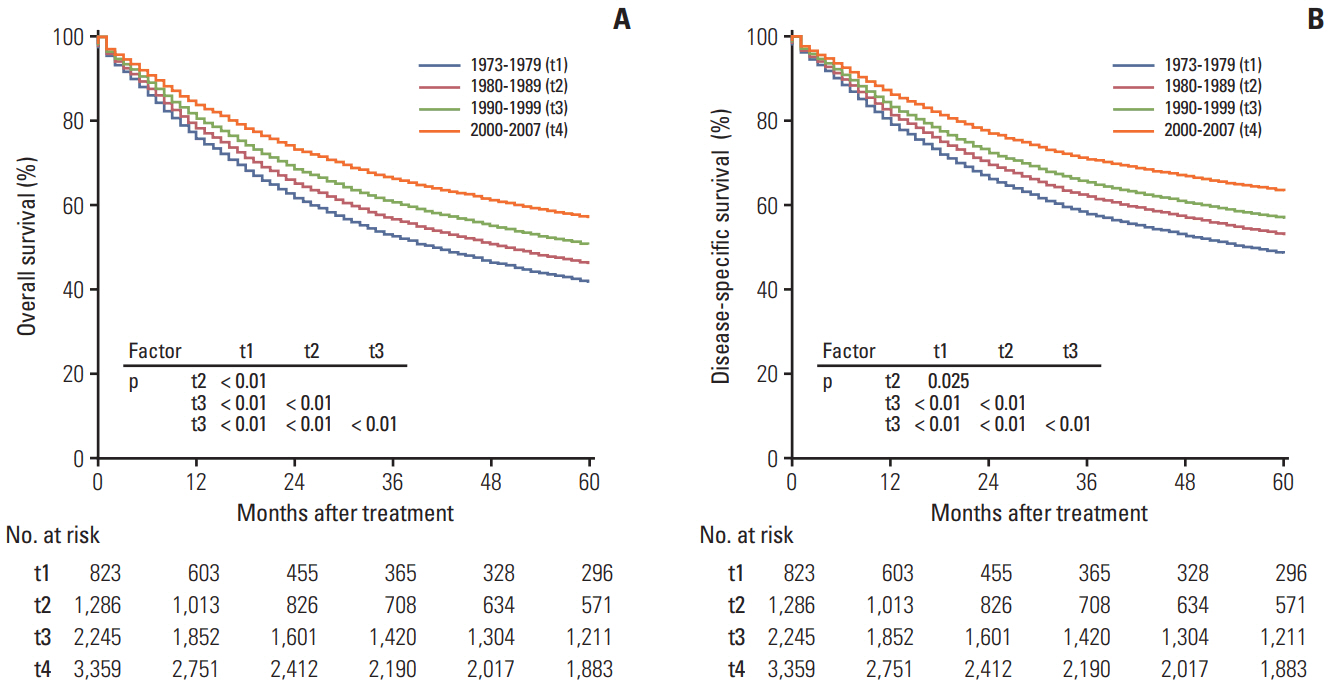
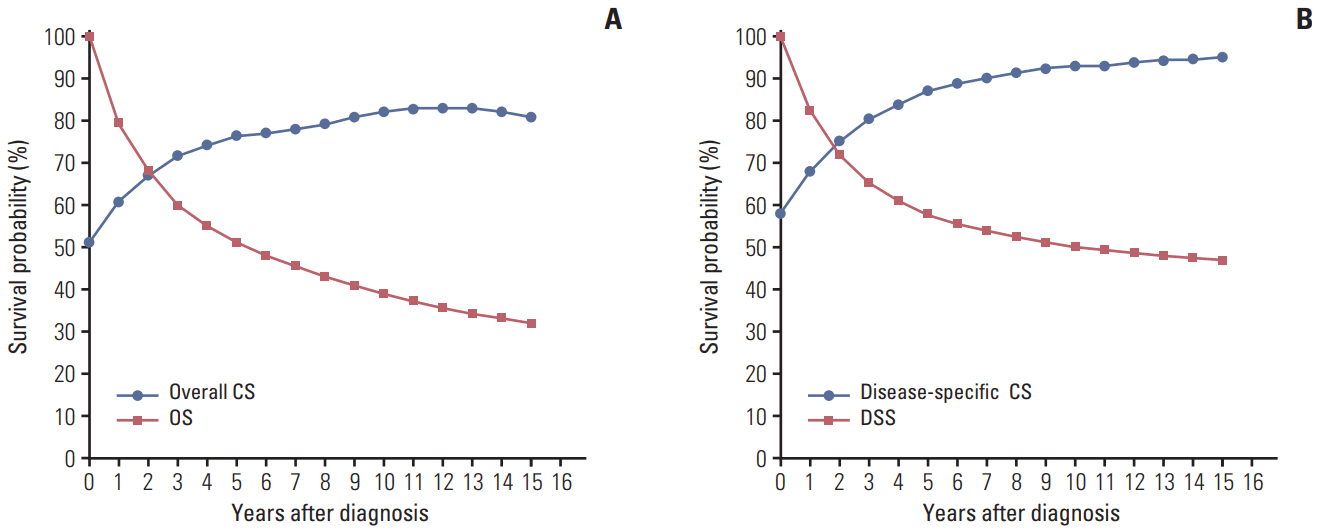
Patients diagnosed with NPC between 1973 and 2007 with at least 5-year follow-up were identified from the Surveillance Epidemiology End Results registry. Traditional survival rates and crude CS estimateswere calculated using Kaplan-Meier analysis. Risk-adjusted survival curves were plotted from the proportional hazards model using the correct group prognosis method.
RESULTS
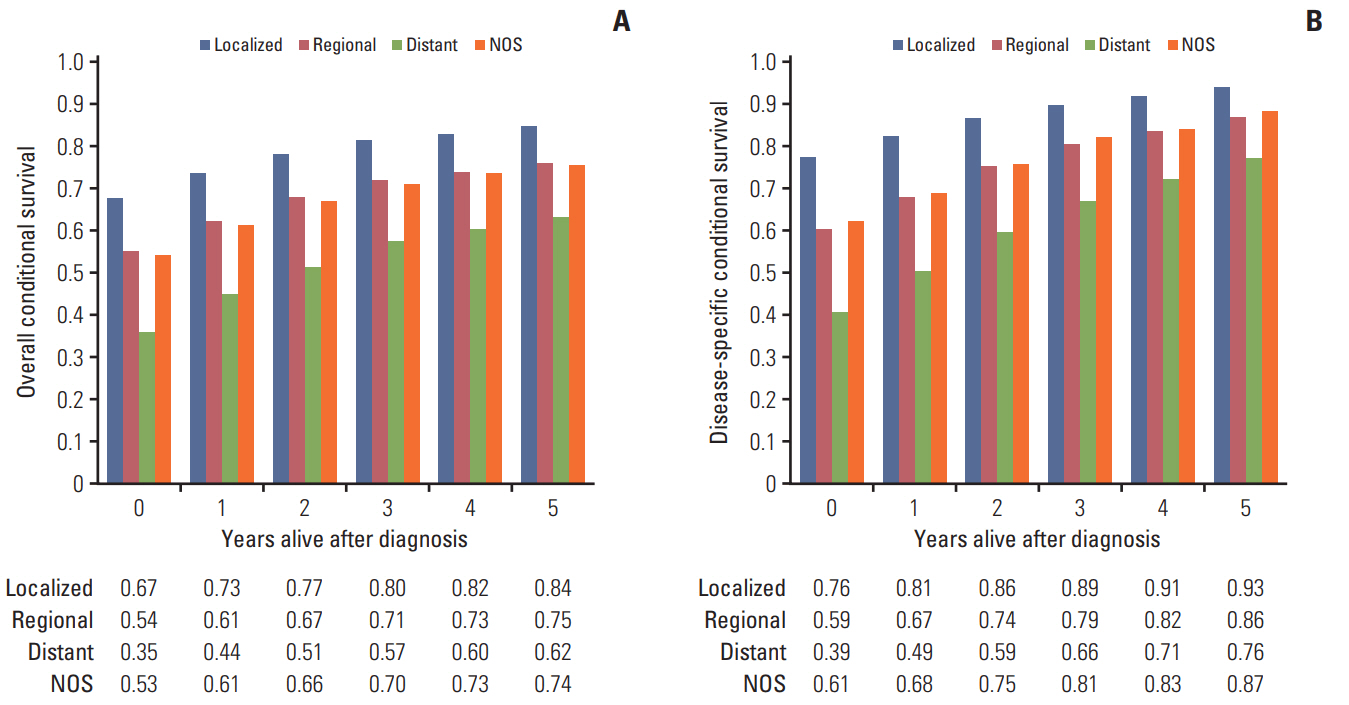
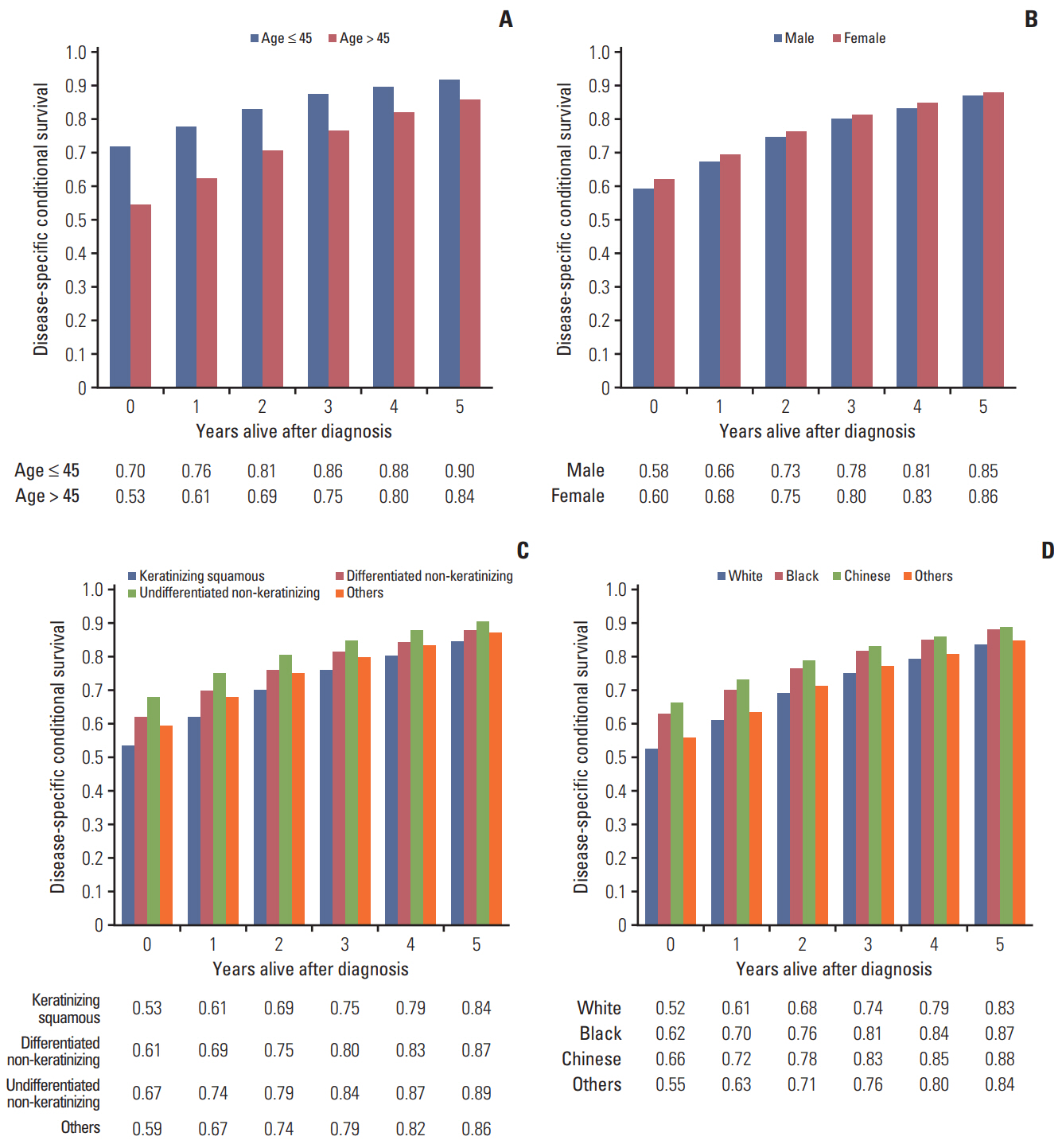
For 7,713 patients analyzed, adjusted baseline 5-year overall survival improved significantly from 36.0% in patients diagnosed in 1973-1979, 41.7% in 1980-1989, 46.6% in 1990-1999, to 54.7% in 2000-2007 (p < 0.01). CS analysis demonstrated that for every additional year survived, adjusted probability of surviving the next 5 years increased from 66.7% (localized), 54.0% (regional), and 35.3% (distant) at the time of diagnosis, to 83.7% (localized), 75.0% (regional), and 62.2% (distant) for patients who had survived 5 years. Adjusted 5-year CS differed among age, sex, tumor histology, ethnicity, and stage subgroups initially, but converged with time.
CONCLUSION
Treatment outcomes of NPC patients have greatly improved over the decades. Increases in CS become more prominent in patients with distant disease than in those with localized or regional disease as patients survive longer. CS provides more dynamic prognostic information for patients who have survived a period of time after diagnosis.
MeSH Terms
Figure
Reference
-
References
1. Tang LL, Chen WQ, Xue WQ, He YQ, Zheng RS, Zeng YX, et al. Global trends in incidence and mortality of nasopharyngeal carcinoma. Cancer Lett. 2016; 374:22–30.
Article2. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article3. Wei KR, Zheng RS, Zhang SW, Liang ZH, Ou ZX, Chen WQ. Nasopharyngeal carcinoma incidence and mortality in China in 2010. Chin J Cancer. 2014; 33:381–7.4. Lai SZ, Li WF, Chen L, Luo W, Chen YY, Liu LZ, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys. 2011; 80:661–8.5. Blanchard P, Lee A, Marguet S, Leclercq J, Ng WT, Ma J, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol. 2015; 16:645–55.
Article6. Sun Y, Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, et al. Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol. 2016; 17:1509–20.7. Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P. Quality of life in long-term cancer survivors. Oncol Nurs Forum. 1995; 22:915–22.8. Skuladottir H, Olsen JH. Conditional survival of patients with the four major histologic subgroups of lung cancer in Denmark. J Clin Oncol. 2003; 21:3035–40.
Article9. Merrill RM, Henson DE, Ries LA. Conditional survival estimates in 34,963 patients with invasive carcinoma of the colon. Dis Colon Rectum. 1998; 41:1097–106.
Article10. Wang SJ, Emery R, Fuller CD, Kim JS, Sittig DF, Thomas CR. Conditional survival in gastric cancer: a SEER database analysis. Gastric Cancer. 2007; 10:153–8.
Article11. Fukui T, Okasaka T, Kawaguchi K, Fukumoto K, Nakamura S, Hakiri S, et al. Conditional survival after surgical intervention in patients with non-small cell lung cancer. Ann Thorac Surg. 2016; 101:1877–82.
Article12. Fuller CD, Wang SJ, Thomas CR Jr, Hoffman HT, Weber RS, Rosenthal DI. Conditional survival in head and neck squamous cell carcinoma: results from the SEER dataset 1973-1998. Cancer. 2007; 109:1331–43.13. ClinicalTrials.gov. Glossary of clinical trial terms [Internet]. Bethesda, MD: US National Institutes of Health;2017. [cited 2017 May 2]. Available from: http://www.clinicaltrials.gov/ct2/info/glossary.14. Chua ML, Wee JT, Hui EP, Chan AT. Nasopharyngeal carcinoma. Lancet. 2016; 387:1012–24.
Article15. Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002; 40(8 Suppl):IV-3-18.16. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of disease for oncology. 3rd ed. Geneva: World Health Organization;2000.17. National Cancer Institute. Summary staging guide, SEER program. NIH Publication No. 81. Bethesda, MD: National Institute of Health;1981. p. 598–603.18. Nieto FJ, Coresh J. Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol. 1996; 143:1059–68.
Article19. Adjusted survival analysis programs [Internet]. Calgary: University of Calgary;2001. [cited 2001 Aug 2]. Available from: http://people.ucalgary.ca/~hquan/adjsurv.html.20. Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982; 69:239–41.
Article21. Gill RD. Multistate life-tables and regression models. Math Popul Stud. 1992; 3:259–76.
Article22. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. AJCC cancer staging handbook: from the AJCC cancer staging manual. 6th ed. New York: Springer;2002.23. Xing Y, Chang GJ, Hu CY, Askew RL, Ross MI, Gershenwald JE, et al. Conditional survival estimates improve over time for patients with advanced melanoma: results from a population-based analysis. Cancer. 2010; 116:2234–41.24. Chang GJ, Hu CY, Eng C, Skibber JM, Rodriguez-Bigas MA. Practical application of a calculator for conditional survival in colon cancer. J Clin Oncol. 2009; 27:5938–43.
Article25. Xiao G, Cao Y, Qiu X, Wang W, Wang Y. Influence of gender and age on the survival of patients with nasopharyngeal carcinoma. BMC Cancer. 2013; 13:226.
Article26. OuYang PY, Zhang LN, Lan XW, Xie C, Zhang WW, Wang QX, et al. The significant survival advantage of female sex in nasopharyngeal carcinoma: a propensity-matched analysis. Br J Cancer. 2015; 112:1554–61.
Article27. Ou SH, Zell JA, Ziogas A, Anton-Culver H. Epidemiology of nasopharyngeal carcinoma in the United States: improved survival of Chinese patients within the keratinizing squamous cell carcinoma histology. Ann Oncol. 2007; 18:29–35.
Article28. Wang SJ, Fuller CD, Emery R, Thomas CR. Conditional survival in rectal cancer: a SEER database analysis. Gastrointest Cancer Res. 2007; 1:84–9.29. Deleyiannis FW, Thomas DB, Vaughan TL, Davis S. Alcoholism: independent predictor of survival in patients with head and neck cancer. J Natl Cancer Inst. 1996; 88:542–9.
Article30. Hsu WL, Chen JY, Chien YC, Liu MY, You SL, Hsu MM, et al. Independent effect of EBV and cigarette smoking on nasopharyngeal carcinoma: a 20-year follow-up study on 9,622 males without family history in Taiwan. Cancer Epidemiol Biomarkers Prev. 2009; 18:1218–26.
Article31. Wang SJ, Fuller CD, Kim JS, Sittig DF, Thomas CR Jr, Ravdin PM. Prediction model for estimating the survival benefit of adjuvant radiotherapy for gallbladder cancer. J Clin Oncol. 2008; 26:2112–7.
Article32. Lee AW, Ma BB, Ng WT, Chan AT. Management of nasopharyngeal carcinoma: current practice and future perspective. J Clin Oncol. 2015; 33:3356–64.
Article33. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korean Brain Tumor registry (II): Registry and Data Base formula
- Introduction of Relative Survival Analysis Program: Using Sample of Cancer Registry Data with Stata Software
- Characteristics and Survival of Korean Anal Cancer From the Korea Central Cancer Registry Data
- Conditional relative survival of cervical cancer: a Korean National Cancer Registry Study
- Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999–2019