Korean J Neurotrauma.
2018 Apr;14(1):39-42. 10.13004/kjnt.2018.14.1.39.
Malignant Metastasis Misdiagnosed as Osteoporotic Compression Fracture: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 2410921
- DOI: http://doi.org/10.13004/kjnt.2018.14.1.39
Abstract
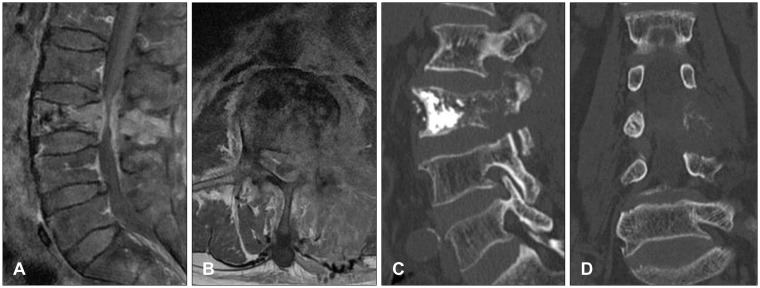
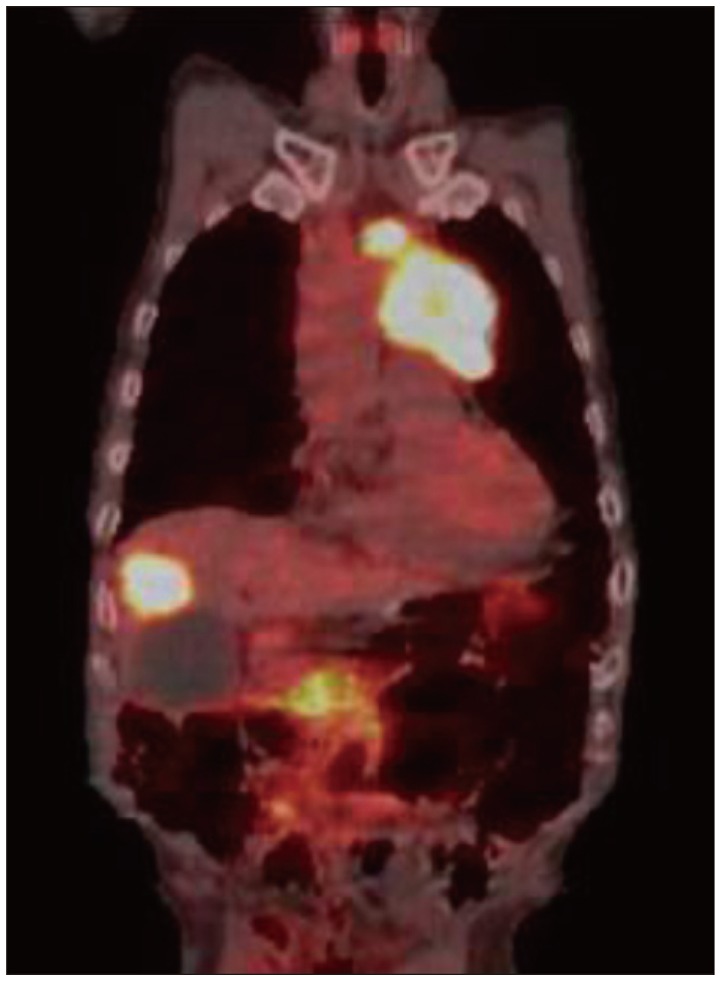
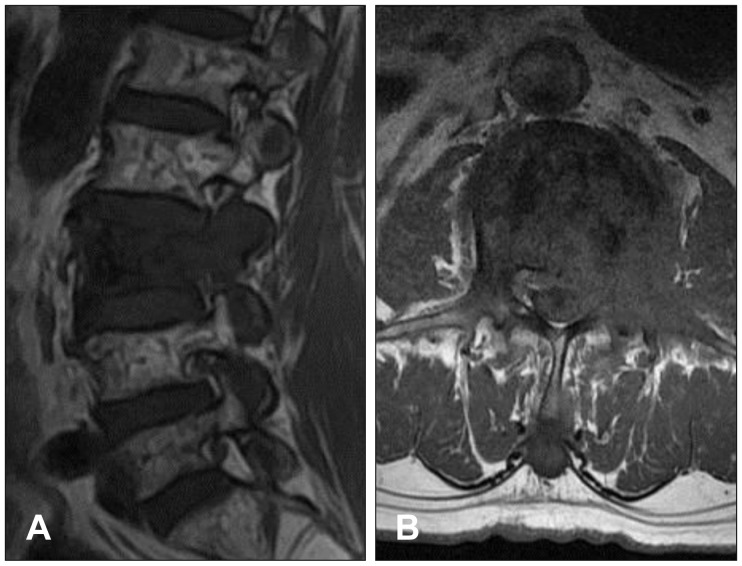
- In cases of vertebral collapse after a trivial injury in elderly patients with severe osteoporosis, it can be a diagnostic challenge to determine whether the cause is a benign compression fracture or malignant metastasis. A 78-year-old male patient was referred to the emergency department for the evaluation of weakness of the left lower limb. He had undergone percutaneous vertebroplasty four months earlier after being diagnosed with L3 osteoporotic compression fracture. He was treated with foraminotomy at the L3-4 level after being diagnosed with foraminal stenosis two months earlier at a spine clinic. Magnetic resonance (MR) images showed significant signal change from the vertebral body to the posterior element, and widely spreading extraspinal extension of soft tissue at L3. Computed tomography scan revealed osteolytic changes in regions including the ventral body and pedicle. Emergent decompressive laminectomy and bone biopsy were performed, and the histologic evaluation showed metastatic squamous cell carcinoma. A retrospective review of previous MR images showed obvious pedicle and facet involvement, and paraspinal extension of soft tissue, which are highly suggestive of malignant metastasis.
Keyword
MeSH Terms
Figure
Reference
-
1. Baker LL, Goodman SB, Perkash I, Lane B, Enzmann DR. Benign versus pathologic compression fractures of vertebral bodies: assessment with conventional spin-echo, chemical-shift, and STIR MR imaging. Radiology. 1990; 174:495–502. PMID: 2296658.
Article2. Chen WT, Shih TT, Chen RC, Lo HY, Chou CT, Lee JM, et al. Blood perfusion of vertebral lesions evaluated with gadolinium-enhanced dynamic MRI: in comparison with compression fracture and metastasis. J Magn Reson Imaging. 2002; 15:308–314. PMID: 11891976.
Article3. Cuénod CA, Laredo JD, Chevret S, Hamze B, Naouri JF, Chapaux X, et al. Acute vertebral collapse due to osteoporosis or malignancy: appearance on unenhanced and gadolinium-enhanced MR images. Radiology. 1996; 199:541–549. PMID: 8668809.
Article4. Ishiyama M, Fuwa S, Numaguchi Y, Kobayashi N, Saida Y. Pedicle involvement on MR imaging is common in osteoporotic compression fractures. AJNR Am J Neuroradiol. 2010; 31:668–673. PMID: 20019106.
Article5. Jeong JH, Roh SW, Rhim SC, Jeon SR. Effectiveness of surgical decompression and fixation in patients with metastatic spinal cord compression. Korean J Spine. 2007; 4:210–214.6. Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003; 23:179–187. PMID: 12533652.7. Spuentrup E, Buecker A, Adam G, van Vaals JJ, Guenther RW. Diffusion-weighted MR imaging for differentiation of benign fracture edema and tumor infiltration of the vertebral body. AJR Am J Roentgenol. 2001; 176:351–358. PMID: 11159073.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraspinal Extradural Cyst Subsequent to a Vertebral Compression Fracture - A Case Report -
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Unilateral Biportal Endoscopy as a Treatment for Acute Radiculopathy after Osteoporotic Lumbar Compression Fracture: A Case Report
- Neglected Osteoporotic Vertebral Compression Fracture Treated with Postural Reduction and Minimally Invasive Transpedicular Fixation with Weekly Teriparatide
- Correlation between Progression of Compression and Bone Densiometry Index in Osteoporotic Compression Fracture of Thoracolumbar Spine