Korean J Neurotrauma.
2018 Apr;14(1):20-23. 10.13004/kjnt.2018.14.1.20.
Improper Use of Thrombolytic Agents in Acute Hemiparesis Following Misdiagnosis of Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 2410916
- DOI: http://doi.org/10.13004/kjnt.2018.14.1.20
Abstract
OBJECTIVE
Acute hemiparesis is often an early presentation of acute ischemic stroke, though it can occur in various disorders. This study aimed to investigate the improper use of thrombolytic agents for patients with acute hemiparesis, following the misdiagnosis of acute ischemic stroke.
METHODS
We analyzed the clinical and radiological data of nine patients initially misdiagnosed with cerebral stroke in the emergency room from May 2013 to January 2017. All the patients were treated with tissue plasminogen activator (TPA) owing to the presence of acute hemiparesis. Subsequently, emergent computed tomography scan showed no intracranial hemorrhage. Clinical findings including neurological deficits, clinical course, and related complications were detected and analyzed.
RESULTS
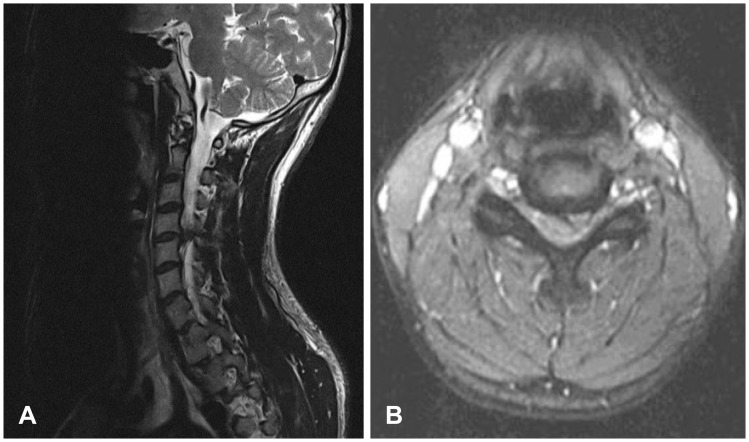
Acute hemiparesis was observed in the following conditions: spontaneous spinal epidural hematoma, Brown-Séquard syndrome caused by cervical disc herniation, cervical epidural abscess, hypoglycemia in the presence of an old stroke, and seizure or convulsion disorder. Although acute hemiparesis was regarded as a contraindication, inappropriate TPA administration did not aggravate the neurological condition in any of the patients who required surgery.
CONCLUSION
Upon presentation of acute hemiparesis, various conditions mimicking cerebral stroke should be considered to avoid misdiagnosis. We suggest that physicians should exercise caution when prescribing thrombolytic agents.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Traumatic Cervical Epidural Hematoma without Osseous Fracture Presenting as Hemiparesis
Hak Soo Lee, Chang Il Ju, Seok Won Kim
Korean J Neurotrauma. 2019;15(2):209-213. doi: 10.13004/kjnt.2019.15.e26.Clinical Differences Between Stroke and Stroke Mimics in Code Stroke Patients
Taekwon Kim, Han-Yeong Jeong, Gil Joon Suh
J Korean Med Sci. 2022;37(7):e54. doi: 10.3346/jkms.2022.37.e54.
Reference
-
1. Adamson DC, Bulsara K, Bronec PR. Spontaneous cervical epidural hematoma: case report and literature review. Surg Neurol. 2004; 62:156–159. PMID: 15261513.
Article2. Dimou J, Jithoo R, Bush S. A patient with delayed traumatic cervical spinal epidural haematoma presenting with hemiparesis. J Clin Neurosci. 2010; 17:404–405. PMID: 20074959.
Article3. Fernandes PM, Whiteley WN, Hart SR, Al-Shahi Salman R. Strokes: mimics and chameleons. Pract Neurol. 2013; 13:21–28. PMID: 23315456.
Article4. Ferro JM, Pinto AN, Falcão I, Rodrigues G, Ferreira J, Falcão F, et al. Diagnosis of stroke by the nonneurologist. A validation study. Stroke. 1998; 29:1106–1109. PMID: 9626279.5. Förster A, Griebe M, Wolf ME, Szabo K, Hennerici MG, Kern R. How to identify stroke mimics in patients eligible for intravenous thrombolysis? J Neurol. 2012; 259:1347–1353. PMID: 22231865.
Article6. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID: 18815396.
Article7. Hand PJ, Kwan J, Lindley RI, Dennis MS, Wardlaw JM. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke. 2006; 37:769–775. PMID: 16484610.8. Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2003; 34:71–76. PMID: 12511753.
Article9. Hemmen TM, Meyer BC, McClean TL, Lyden PD. Identification of nonischemic stroke mimics among 411 code strokes at the University of California, San Diego, Stroke Center. J Stroke Cerebrovasc Dis. 2008; 17:23–25. PMID: 18190817.
Article10. Korean Stroke Society. Stroke. ed 2. Seoul: Panmuneducation;2015.11. Kothari RU, Brott T, Broderick JP, Hamilton CA. Emergency physicians. Accuracy in the diagnosis of stroke. Stroke. 1995; 26:2238–2241. PMID: 7491643.12. Lemmens R, Ceuppens J, Wilms G, Depreitere B. Transient hemiparesis caused by spontaneous cervical epidural hematoma. Acta Neurol Belg. 2012; 112:291–293. PMID: 22565778.
Article13. Libman RB, Wirkowski E, Alvir J, Rao TH. Conditions that mimic stroke in the emergency department. Implications for acute stroke trials. Arch Neurol. 1995; 52:1119–1122. PMID: 7487564.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hemoperitoneum after Intraarterial Urokinase Infusion for Acute Ischemic Stroke
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Performance Rate of Thrombolytic Therapy and Acute Prognosis of Hyperacute Ischemic Stroke
- Problem Based Approach in Acute Ischemic Stroke
- Recent advances in thrombolysis of acute ischemic stroke