Yonsei Med J.
2018 Jun;59(4):480-488. 10.3349/ymj.2018.59.4.480.
Effects of Coronary Artery Revascularization with a Polymer-Free Biolimus A9–Coated BioFreedom Stent Versus Bypass Surgery before Noncardiac Surgery
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. kimbk@yuhs.ac
- 2Division of Cardiology, Department of Internal Medicine, Konkuk University Chungju Hospital, Chungju, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2410902
- DOI: http://doi.org/10.3349/ymj.2018.59.4.480
Abstract
- PURPOSE
The present study aimed to evaluate the efficacy and safety of polymer-free drug-coated BioFreedom stent implantation in comparison to coronary artery bypass graft (CABG) before major noncardiac surgery.
MATERIALS AND METHODS
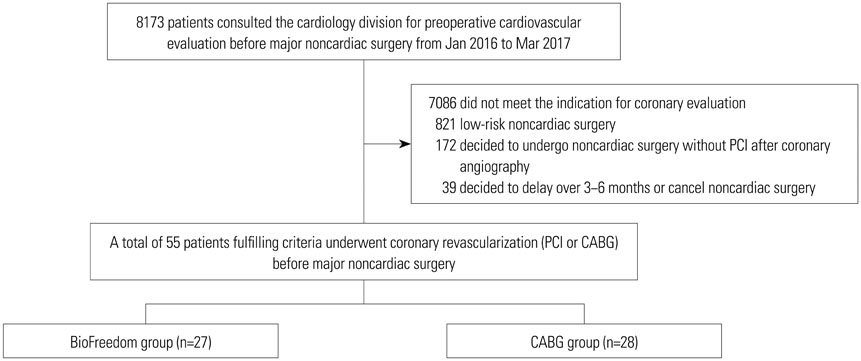
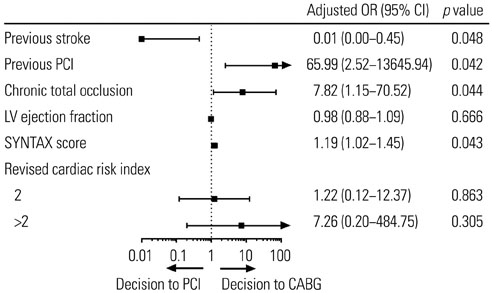
In a multicenter registry, 55 patients required revascularization before major noncardiac surgery that should not be delayed >6 months. Of them, 27 underwent BioFreedom stent implantation and 28 underwent CABG. Primary outcomes included rate of noncardiac surgery, time from revascularization to noncardiac surgery, and occurrence of composite outcomes (all-cause death, myocardial infarction, stent thrombosis, stroke, repeat revascularization, or major bleeding).
RESULTS
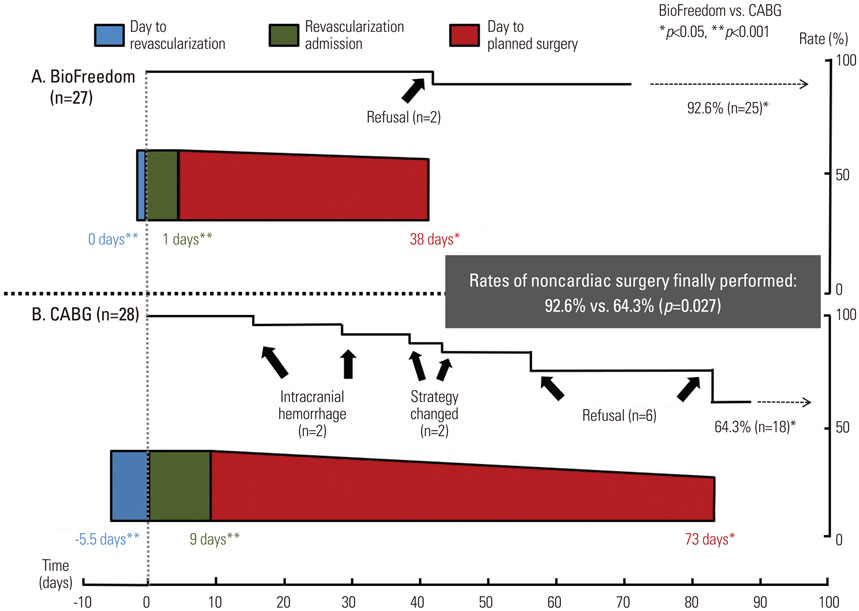
The rate of major noncardiac surgery was significantly higher in the BioFreedom group (92.6%) than in the CABG group (64.3%; p=0.027). Time from revascularization to noncardiac surgery was significantly shorter in the BioFreedom group (38.0 days) than in the CABG group (73.0 days; p=0.042). During the hospitalization for revascularization period, the occurrence of primary outcomes did not differ between the groups. However, the BioFreedom group showed a shorter hospitalization period and lower total treatment cost than the CABG group. During the hospital stay for noncardiac surgery, the occurrence of composite outcome was not significantly different between groups (4% vs. 0%; p>0.999): stroke occurred in only 1 case, and there were no cases of death or stent thrombosis in the BioFreedom group.
CONCLUSION
This study demonstrated that BioFreedom stenting as a revascularization strategy before major noncardiac surgery might be feasible and safe in selected patients with less severe coronary artery diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, Hert SD, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on noncardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014; 35:2383–2431.
Article2. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016; 134:e123–e155.
Article3. Urban P, Meredith IT, Abizaid A, Pocock SJ, Carrié D, Naber C, et al. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med. 2015; 373:2038–2047.
Article4. Garot P, Morice MC, Tresukosol D, Pocock SJ, Meredith IT, Abizaid A, et al. 2-year outcomes of high bleeding risk patients after polymer-free drug-coated stents. J Am Coll Cardiol. 2017; 69:162–171.
Article5. Kim JS, Lee BH, Ko YG, Choi D, Jang Y, Min PK, et al. Comparison of sirolimus-eluting stent and paclitaxel-eluting stent for long-term cardiac adverse events in diabetic patients: the Korean Multicenter Angioplasty Team (KOMATE) Registry. Catheter Cardiovasc Interv. 2008; 72:601–607.
Article6. Kim BK, Oh S, Jeon DW, Yang JY, Kim JS, Park S, et al. Long-term clinical outcomes and stent thrombosis of sirolimus-eluting versus bare metal stents in patients with end-stage renal disease: results of Korean multicenter angioplasty team (KOMATE) Registry. J Interv Cardiol. 2009; 22:411–419.
Article7. Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014; 64:e77–e137.8. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.9. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012; 60:1581–1598.
Article10. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.
Article11. Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I:a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987; 76:142–154.
Article12. Curtis AJ, Russell CO, Stoelwinder JU, McNeil JJ. Waiting lists and elective surgery: ordering the queue. Med J Aust. 2010; 192:217–220.
Article13. Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012; 41:734–744.
Article14. Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013; 381:629–638.
Article15. Kim BK, Yoon JH, Shin DH, Kim JS, Ko YG, Choi D, et al. Prospective and systematic analysis of unexpected requests for non-cardiac surgery or other invasive procedures during the first year after drug-eluting stent implantation. Yonsei Med J. 2014; 55:345–352.
Article16. Mäkikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016; 388:2743–2752.
Article17. Ahn JM, Park DW, Lee CW, Chang M, Cavalcante R, Sotomi Y, et al. Comparison of stenting versus bypass surgery according to the completeness of revascularization in severe coronary artery disease: patient-level pooled analysis of the SYNTAX, PRECOMBAT, and BEST Trials. JACC Cardiovasc Interv. 2017; 10:1415–1424.
Article18. Korte W, Cattaneo M, Chassot PG, Eichinger S, von Heymann C, Hofmann N, et al. Peri-operative management of antiplatelet therapy in patients with coronary artery disease: joint position paper by members of the working group on Perioperative Haemostasis of the Society on Thrombosis and Haemostasis Research (GTH), the working group on Perioperative Coagulation of the Austrian Society for Anesthesiology, Resuscitation and Intensive Care (ÖGARI) and the Working Group Thrombosis of the European Society for Cardiology (ESC). Thromb Haemost. 2011; 105:743–749.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nobori-Biolimus-Eluting Stents versus Resolute Zotarolimus-Eluting Stents in Patients Undergoing Coronary Intervention: A Propensity Score Matching
- Ischemia-guided Revascularization for Stable Ischemic Heart Disease
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Stenting versus Bypass Surgery for the Treatment of Left Main Coronary Artery Disease
- Perioperative management for patients undergoing noncardiac surgery after percutaneous coronary intervention