Korean J Pain.
2018 Apr;31(2):102-108. 10.3344/kjp.2018.31.2.102.
Effects of warmed carrier fluid on nefopam injection-induced pain
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Myongji Hospital, Goyang, Korea. 05142@mjh.or.kr
- KMID: 2410832
- DOI: http://doi.org/10.3344/kjp.2018.31.2.102
Abstract
- BACKGROUND
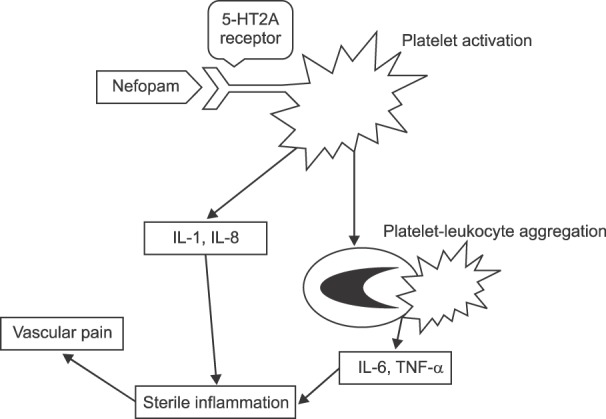
Nefopam is a non-opioid, non-steroidal analgesic drug with fewer adverse effects than narcotic analgesics and nonsteroidal anti-inflammatory drugs, and is widely used for postoperative pain control. Because nefopam sometimes causes side effects such as nausea, vomiting, somnolence, hyperhidrosis and injection-related pain, manufacturers are advised to infuse it slowly, over a duration of 15 minutes. Nevertheless, pain at the injection site is very common. Therefore, we investigated the effect of warmed carrier fluid on nefopam injection-induced pain.
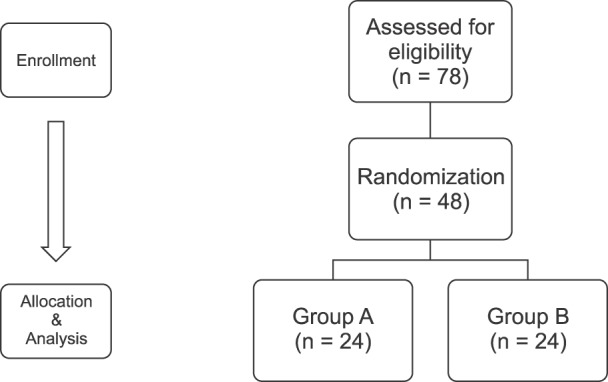
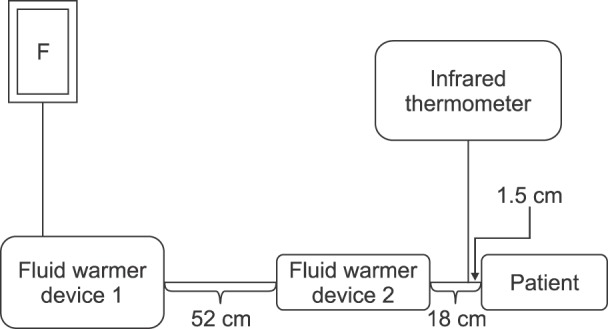
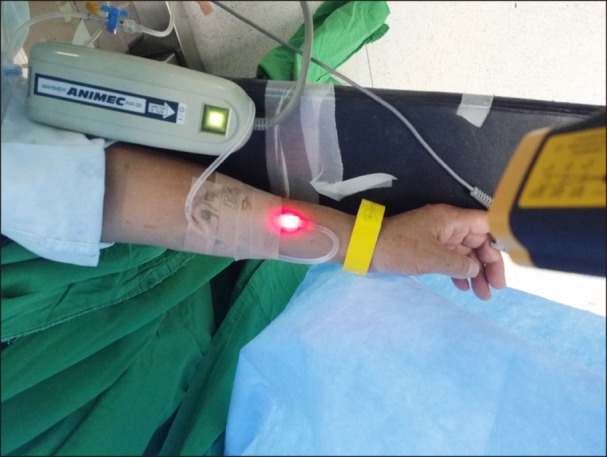
METHODS
A total of 48 patients were randomly selected and allocated to either a control or a warming group. Warming was performed by diluting 40 mg of nefopam in 100 ml of normal saline heated to 31-32℃ using two fluid warmers. The control group was administered 40 mg of nefopam dissolved in 100 ml of normal saline stored at room temperature (21-22℃) through the fluid warmers, but the fluid warmers were not activated.
RESULTS
The pain intensity was lower in the warming group than in the control group (P < 0.001). The pain severity and tolerance measurements also showed statistically significant differences between groups (P < 0.001). In the analysis of vital signs before and after the injection, the mean blood pressure after the injection differed significantly between the groups (P = 0.005), but the heart rate did not. The incidence of hypertension also showed a significant difference between groups (P = 0.017).
CONCLUSIONS
Use of warmed carrier fluid for nefopam injection decreased injection-induced pain compared to mildly cool carrier fluid.
Keyword
MeSH Terms
Figure
Reference
-
1. Girard P, Chauvin M, Verleye M. Nefopam analgesia and its role in multimodal analgesia: a review of preclinical and clinical studies. Clin Exp Pharmacol Physiol. 2016; 43:3–12. PMID: 26475417.
Article2. Kim YM, Lim BG, Kim H, Kong MH, Lee MK, Lee IO. Slow injection of nefopam reduces pain intensity associated with intravenous injection: a prospective randomized trial. J Anesth. 2014; 28:399–406. PMID: 24201414.
Article3. Dordoni PL, Della Ventura M, Stefanelli A, Iannace E, Paparella P, Rocca B, et al. Effect of ketorolac, ketoprofen and nefopam on platelet function. Anaesthesia. 1994; 49:1046–1049. PMID: 7864317.
Article4. Bhatt AM, Pleuvry BJ, Maddison SE. Respiratory and metabolic effects of oral nefopam in human volunteers. Br J Clin Pharmacol. 1981; 11:209–211. PMID: 6783057.
Article5. Evans MS, Lysakowski C, Tramèr MR. Nefopam for the prevention of postoperative pain: quantitative systematic review. Br J Anaesth. 2008; 101:610–617. PMID: 18796441.
Article6. Piercey MF, Schroeder LA. Spinal and supraspinal sites for morphine and nefopam analgesia in the mouse. Eur J Pharmacol. 1981; 74:135–140. PMID: 6276187.
Article7. Heel RC, Brogden RN, Pakes GE, Speight TM, Avery GS. Nefopam: a review of its pharmacological properties and therapeutic efficacy. Drugs. 1980; 19:249–267. PMID: 6991238.8. Durrieu G, Olivier P, Bagheri H, Montastruc JL. Overview of adverse reactions to nefopam: an analysis of the French Pharmacovigilance database. Fundam Clin Pharmacol. 2007; 21:555–558. PMID: 17868209.
Article9. Jung KT, Kim HJ, Bae HS, Lee HY, Kim SH, So KY, et al. Effects of lidocaine, ketamine, and remifentanil on withdrawal response of rocuronium. Korean J Anesthesiol. 2014; 67:175–180. PMID: 25302093.
Article10. Polat R, Aktay M, Ozlü O. The effects of remifentanil, lidocaine, metoclopramide, or ketamine pretreatment on propofol injection pain. Middle East J Anaesthesiol. 2012; 21:673–677. PMID: 23265029.11. Alipour M, Tabari M, Alipour M. Paracetamol, ondansetron, granisetron, magnesium sulfate and lidocaine and reduced propofol injection pain. Iran Red Crescent Med J. 2014; 16:e16086. PMID: 24829787.
Article12. Mahajan C, Rath GP, Bithal PK, Prabhakar H, Yadav R, Dube SK. Local warming at injection site helps alleviate pain after rocuronium administration. J Anesth. 2010; 24:845–848. PMID: 20737278.
Article13. Jeong M, Yoon H. Comparison of the effects of lidocaine pre-administration and local warming of the intravenous access site on propofol injection pain: randomized, double-blind controlled trial. Int J Nurs Stud. 2016; 61:209–218. PMID: 27372434.
Article14. Youn AM, Hsu TM. Heated carrier fluids in decreasing propofol injection pain: a randomized, controlled trial. Korean J Anesthesiol. 2017; 70:33–38. PMID: 28184264.
Article15. Kim DJ, Kim SH, So KY, An TH. Mega Acer Kit® is more effective for warming the intravenous fluid than Ranger™ and ThermoSens® at 440 ml/h of infusion rate: an experimental performance study. Korean J Anesthesiol. 2017; 70:456–461. PMID: 28794842.
Article16. Klement W, Arndt JO. Pain on i.v. injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991; 66:189–195. PMID: 1817619.
Article17. Gregori-Puigjane E, Setola V, Hert J, Crews BA, Irwin JJ, Lounkine E, et al. Identifying mechanism-of-action targets for drugs and probes. Proc Natl Acad Sci U S A. 2012; 109:11178–11183. PMID: 22711801.
Article18. Raote I, Bhattacharya A, Panicker MM. Serotonin 2A(5-HT2A) receptor function: ligand-dependent mechanisms and pathways. In : Chattopadhyay A, editor. Serotonin receptors in neurobiology. Boca Raton (FL): CRC Press;2007. p. 105–132.19. Kaplanski G, Porat R, Aiura K, Erban JK, Gelfand JA, Dinarello CA. Activated platelets induce endothelial secretion of interleukin-8 in vitro via an interleukin-1-mediated event. Blood. 1993; 81:2492–2495. PMID: 8490165.
Article20. Neumann FJ, Marx N, Gawaz M, Brand K, Ott I, Rokitta C, et al. Induction of cytokine expression in leukocytes by binding of thrombin-stimulated platelets. Circulation. 1997; 95:2387–2394. PMID: 9170401.
Article21. Christen S, Delachaux A, Dischl B, Golay S, Liaudet L, Feihl F, et al. Dose-dependent vasodilatory effects of acetylcholine and local warming on skin microcirculation. J Cardiovasc Pharmacol. 2004; 44:659–664. PMID: 15550784.
Article22. Minson CT, Berry LT, Joyner MJ. Nitric oxide and neurally mediated regulation of skin blood flow during local heating. J Appl Physiol (1985). 2001; 91:1619–1626. PMID: 11568143.
Article23. Taylor WF, Johnson JM, O'Leary D, Park MK. Effect of high local temperature on reflex cutaneous vasodilation. J Appl Physiol Respir Environ Exerc Physiol. 1984; 57:191–196. PMID: 6469780.
Article24. Elstad M, Vanggaard L, Lossius AH, Walløe L, Bergersen TK. Responses in acral and non-acral skin vasomotion and temperature during lowering of ambient temperature. J Therm Biol. 2014; 45:168–174. PMID: 25436967.
Article25. Bergersen TK, Skytioti M, Elstad M. Cold-induced sympathetic tone modifies the impact of endothelium-dependent vasodilation in the finger pulp. Auton Neurosci. 2017; 203:97–102. PMID: 27932205.
Article26. Hagemann K, Platte G, Meyer J, Effert S. Haemodynamic effects of nefopam (author's transl). Dtsch Med Wochenschr. 1978; 103:1040–1043. PMID: 668511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Nefopam in Perioperative Pain Management; Keeping Nefopam in between
- Effects of Nefopam on Streptozotocin-Induced Diabetic Neuropathic Pain in Rats
- Combination of nefopam and remifentanil is more effective to reduce rocuronium-induced withdrawal response compared with remifentanil alone: a prospective, double-blinded, randomized control study
- Antinociceptive Effect of Intrathecal Nefopam and Interaction with Morphine in Formalin-Induced Pain of Rats
- The Potential Role of Intrathecal Nefopam in the Management of Neuropathic Pain