Korean J Pain.
2018 Apr;31(2):93-101. 10.3344/kjp.2018.31.2.93.
Pain alleviation in patients undergoing cardiac surgery; presternal local anesthetic and magnesium infiltration versus conventional intravenous analgesia: a randomized double-blind study
- Affiliations
-
- 1Department of Anesthesia, ICU, and Pain, Faculty of Medicine, Assiut University, Assiut, Egypt. sayed_k_72@yahoo.com
- 2Department of Cardiothoracic, Faculty of Medicine, Assiut University, Assiut, Egypt.
- 3Department of Clinical Pathology, Faculty of Medicine, Assiut University, Assiut, Egypt.
- KMID: 2410831
- DOI: http://doi.org/10.3344/kjp.2018.31.2.93
Abstract
- BACKGROUND
Magnesium is one of the effective, safe local anesthetic adjuvants that can exert an analgesic effect in conditions presenting acute and chronic post-sternotomy pain. We studied the efficacy of continuous infusion of presternal magnesium sulfate with bupivacaine for pain relief following cardiac surgery.
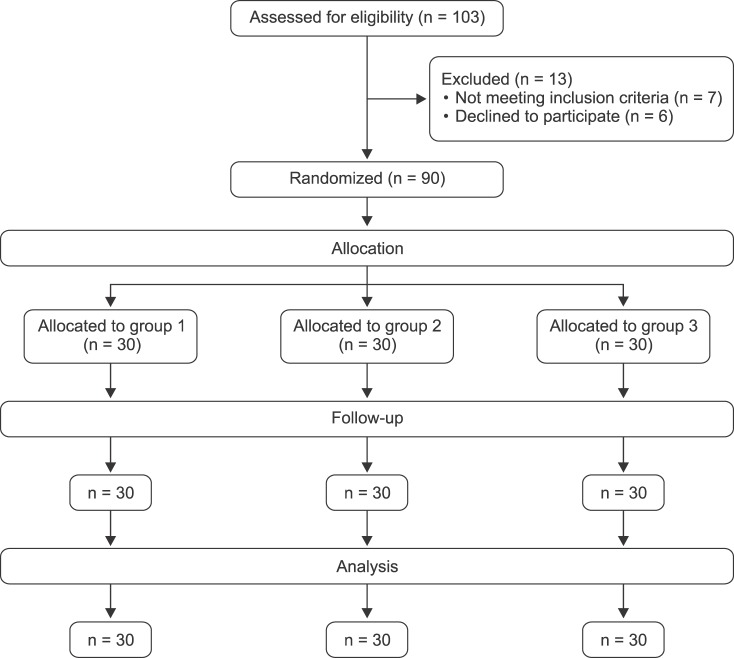
METHODS
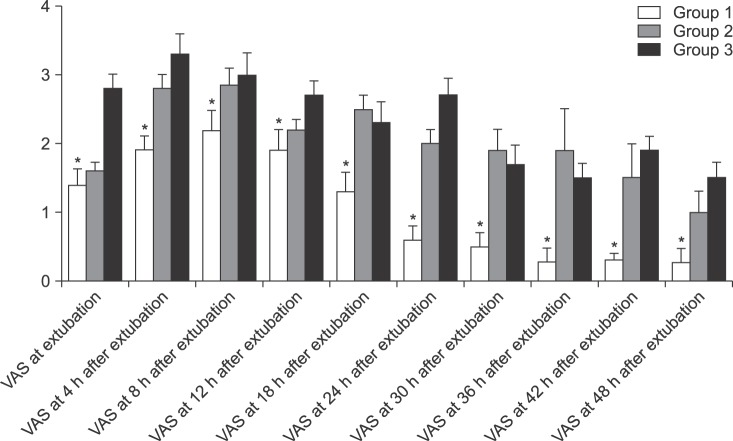
Ninety adult patients undergoing valve replacement cardiac surgery randomly allocated into three groups. In all patients; a presternal catheter was placed for continuous infusion of either 0.125% bupivacaine and 5% magnesium sulfate (3 ml/h for 48 hours) in group 1, or 0.125% bupivacaine only in the same rate in group 2, versus conventional intravenous paracetamol and ketorolac in group 3. Rescue analgesia was iv 25 µg fentanyl. Postoperative Visual Analog Scale (VAS) and fentanyl consumption during the early two postoperative days were assessed. All patients were followed up over two months for occurrence of chronic post-sternotomy pain.
RESULTS
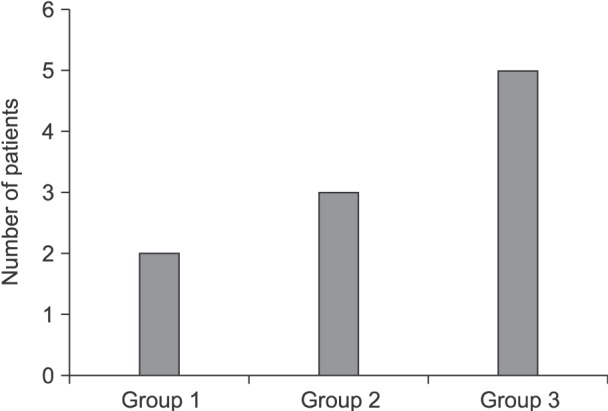
VAS values showed high significant differences during the first 48 hours with the least pain scale in group 1 and significantly least fentanyl consumption (30.8 ± 7 µg in group 1 vs. 69 ± 18 µg in group 2, and 162 ± 3 in group 3 respectively). The incidence of chronic pain has not differed between the three groups although it was more pronounced in group 3.
CONCLUSIONS
Continuous presternal bupivacaine and magnesium infusion resulted in better postoperative analgesia than both presternal bupivacaine alone or conventional analgesic groups.
MeSH Terms
Figure
Reference
-
1. Mueller XM, Tinguely F, Tevaearai HT, Revelly JP, Chioléro R, von Segesser LK. Pain location, distribution, and intensity after cardiac surgery. Chest. 2000; 118:391–396. PMID: 10936130.
Article2. Huang AP, Sakata RK. Pain after sternotomy - review. Rev Bras Anestesiol. 2016; 66:395–401. PMID: 25796483.
Article3. Cheong WK, Seow-Choen F, Eu KW, Tang CL, Heah SM. Randomized clinical trial of local bupivacaine perfusion versus parenteral morphine infusion for pain relief after laparotomy. Br J Surg. 2001; 88:357–359. PMID: 11260098.
Article4. Horn EP, Schroede F, Wilhelm S, Wappler F, Sessler DI, Uebe B, et al. Wound infiltration and drain lavage with ropivacaine after major shoulder surgery. Anesth Analg. 1999; 89:1461–1466. PMID: 10589629.
Article5. Wheatley GH 3rd, Rosenbaum DH, Paul MC, Dine AP, Wait MA, Meyer DM, et al. Improved pain management outcomes with continuous infusion of a local anesthetic after thoracotomy. J Thorac Cardiovasc Surg. 2005; 130:464–468. PMID: 16077414.
Article6. Zohar E, Fredman B, Phillipov A, Jedeikin R, Shapiro A. The analgesic efficacy of patient-controlled bupivacaine wound instillation after total abdominal hysterectomy with bilateral salpingo-oophorectomy. Anesth Analg. 2001; 93:482–487. PMID: 11473884.
Article7. Srebro D, Vučković S, Milovanović A, Košutić J, Vujović KS, Prostran M. Magnesium in pain research: state of the art. Curr Med Chem. 2017; 24:424–434.
Article8. Sirvinskas E, Laurinaitis R. Use of magnesium sulfate in anesthesiology. Medicina (Kaunas). 2002; 38:695–698. PMID: 12474653.9. Lysakowski C, Dumont L, Czarnetzki C, Tramèr MR. Magnesium as an adjuvant to postoperative analgesia: a systematic review of randomized trials. Anesth Analg. 2007; 104:1532–1539. PMID: 17513654.
Article10. Kundra S, Singh RM, Singh G, Singh T, Jarewal V, Katyal S. Efficacy of magnesium sulphate as an adjunct to ropivacaine in local infiltration for postoperative pain following lower segment caesarean section. J Clin Diagn Res. 2016; 10:UC18–UC22.
Article11. Eldaba AA, Amr YM, Sobhy RA. Effect of wound infiltration with bupivacaine or lower dose bupivacaine/magnesium versus placebo for postoperative analgesia after cesarean section. Anesth Essays Res. 2013; 7:336–340. PMID: 25885979.
Article12. Veering BT, Burm AG, Feyen HM, Olieman W, Souverijn JH, Van Kleef JW. Pharmacokinetics of bupivacaine during postoperative epidural infusion: enantioselectivity and role of protein binding. Anesthesiology. 2002; 96:1062–1069. PMID: 11981143.13. Mets B. The pharmacokinetics of anesthetic drugs and adjuvants during cardiopulmonary bypass. Acta Anaesthesiol Scand. 2000; 44:261–273. PMID: 10714838.
Article14. Chiu KM, Wu CC, Wang MJ, Lu CW, Shieh JS, Lin TY, et al. Local infusion of bupivacaine combined with intravenous patient-controlled analgesia provides better pain relief than intravenous patient-controlled analgesia alone in patients undergoing minimally invasive cardiac surgery. J Thorac Cardiovasc Surg. 2008; 135:1348–1352. PMID: 18544384.
Article15. Nasr DA, Abdelhamid HM, Mohsen M, Aly AH. The analgesic efficacy of continuous presternal bupivacaine infusion through a single catheter after cardiac surgery. Ann Card Anaesth. 2015; 18:15–20. PMID: 25566704.
Article16. Kocabas S, Yedicocuklu D, Yuksel E, Uysallar E, Askar F. Infiltration of the sternotomy wound and the mediastinal tube sites with 0.25% levobupivacaine as adjunctive treatment for postoperative pain after cardiac surgery. Eur J Anaesthesiol. 2008; 25:842–849. PMID: 18538054.
Article17. Lee JH, Yang WD, Han SY, Noh JI, Cho SH, Kim SH, et al. Effect of epidural magnesium on the incidence of chronic postoperative pain after video-assisted thoracic surgery. J Cardiothorac Vasc Anesth. 2012; 26:1055–1059. PMID: 22883445.
Article18. Steyaert A, Forget P, Dubois V, Lavand'homme P, De Kock M. Does the perioperative analgesic/anesthetic regimen influence the prevalence of long-term chronic pain after mastectomy? J Clin Anesth. 2016; 33:20–25. PMID: 27555127.
Article19. Kim MH, Lee KY, Park S, Kim SI, Park HS, Yoo YC. Effects of systemic lidocaine versus magnesium administration on postoperative functional recovery and chronic pain in patients undergoing breast cancer surgery: a prospective, randomized, double-blind, comparative clinical trial. PLoS One. 2017; 12:e0173026. PMID: 28253307.
Article20. Kwekkeboom KL, Costanzo ES, Campbell TC. Stress biomarkers in advanced cancer patients experiencing the pain, fatigue, sleep disturbance symptom cluster. J Clin Oncol. 2015; 33:5.
Article21. Gong S, Miao YL, Jiao GZ, Sun MJ, Li H, Lin J, et al. Dynamics and correlation of serum cortisol and corticosterone under different physiological or stressful conditions in mice. PLoS One. 2015; 10:e0117503. PMID: 25699675.
Article22. Gottardo F, Scollo A, Contiero B, Ravagnani A, Tavella G, Bernardini D, et al. Pain alleviation during castration of piglets: a comparative study of different farm options. J Anim Sci. 2016; 94:5077–5088. PMID: 28046151.
Article23. Ahiskalioglu A, Ahiskalioglu OE, Dostbil A, Can A, Aksoy M, Incel İ, et al. The effect of epidural levobupivacaine and fentanyl on stress response and pain management in patients undergoing percutaneous nephrolithotomy. West Indian Med J. 2016; [in press].
Article24. Kamble SP, Bevinaguddaiah Y, Nagaraja DC, Pujar VS, Anandaswamy TC. Effect of magnesium sulfate and clonidine in attenuating hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy. Anesth Essays Res. 2017; 11:67–71. PMID: 28298759.
Article25. Jee D, Lee D, Yun S, Lee C. Magnesium sulphate attenuates arterial pressure increase during laparoscopic cholecystectomy. Br J Anaesth. 2009; 103:484–489. PMID: 19617379.
Article26. Altura BM, Altura BT. Magnesium and vascular tone and reactivity. Blood Vessels. 1978; 15:5–16. PMID: 630136.
Article27. Donadi PK, Moningi S, Gopinath R. Comparison of bupivacaine and bupivacaine plus magnesium sulphate infiltration for postoperative analgesia in patients undergoing lumbar laminectomy: a prospective randomised double-blinded controlled study. J Neuroanaesth Crit Care. 2014; 1:183–187.
Article28. White PF, Rawal S, Latham P, Markowitz S, Issioui T, Chi L, et al. Use of a continuous local anesthetic infusion for pain management after median sternotomy. Anesthesiology. 2003; 99:918–923. PMID: 14508326.
Article29. Agarwal S, Nuttall GA, Johnson ME, Hanson AC Jr, Oliver WC. A prospective, randomized, blinded study of continuous ropivacaine infusion in the median sternotomy incision following cardiac surgery. Reg Anesth Pain Med. 2013; 38:145–150. PMID: 23386053.
Article30. Guillier M, Boselli E, Bouvet L, Freney J, Renaud FN, Chassard D, et al. Levobupivacaine hydrochloride and sufentanil have no antimicrobial effect at 25 degrees C in vitro. Eur J Anaesthesiol. 2007; 24:634–639. PMID: 17376254.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnesium: a versatile drug for anesthesiologists
- Analgesic Effect of Epidural Morphine and Incisional Site Infiltration with Bupivacaine in the Lower Abdominal Surgery
- Post-operative analgesia of 2% lignocaine with or without magnesium sulfate for inferior alveolar nerve block in symptomatic mandibular molars - a randomized double blind controlled clinical trial
- The benefits of preincision ropivacaine infiltration for reducing postoperative pain after robotic bilateral axillo-breast approach thyroidectomy: a prospective, randomized, double-blind, placebo-controlled study
- Comparison of pain relief in soft tissue tumor excision: anesthetic injection using an automatic digital injector versus conventional injection