J Periodontal Implant Sci.
2018 Apr;48(2):103-113. 10.5051/jpis.2018.48.2.103.
Comparison of marginal bone loss between internal- and external-connection dental implants in posterior areas without periodontal or peri-implant disease
- Affiliations
-
- 1Department of Periodontology, Dental Research Institute, Seoul National University School of Dentistry, Seoul, Korea. kst72@snu.ac.kr
- KMID: 2410689
- DOI: http://doi.org/10.5051/jpis.2018.48.2.103
Abstract
- PURPOSE
The purpose of this retrospective study with 4-12 years of follow-up was to compare the marginal bone loss (MBL) between external-connection (EC) and internal-connection (IC) dental implants in posterior areas without periodontal or peri-implant disease on the adjacent teeth or implants. Additional factors influencing MBL were also evaluated.
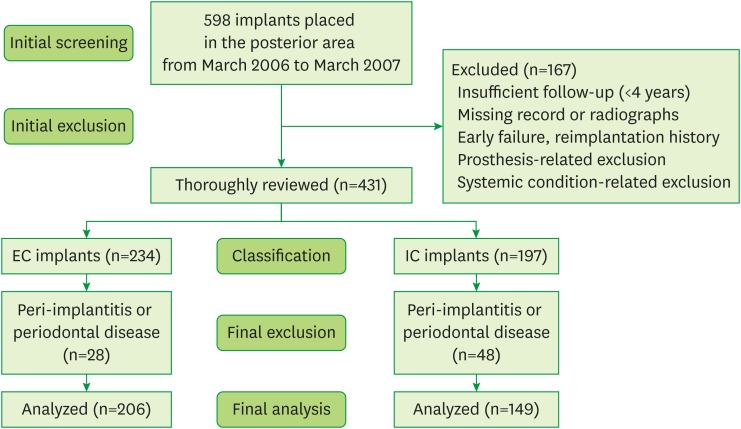
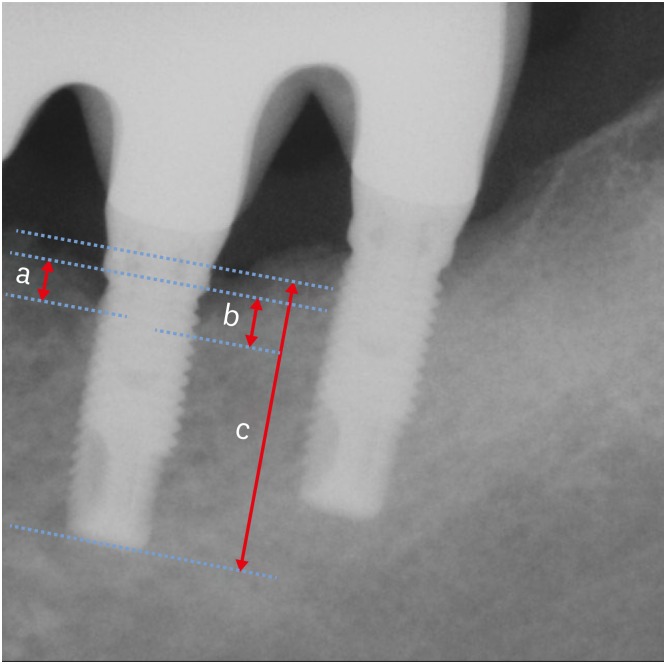
METHODS
This retrospective study was performed using dental records and radiographic data obtained from patients who had undergone dental implant treatment in the posterior area from March 2006 to March 2007. All the implants that were included had follow-up periods of more than 4 years after loading and satisfied the implant success criteria, without any peri-implant or periodontal disease on the adjacent implants or teeth. They were divided into 2 groups: EC and IC. Subgroup comparisons were conducted according to splinting and the use of cement in the restorations. A statistical analysis was performed using the Mann-Whitney U test for comparisons between 2 groups and the Kruskal-Wallis test for comparisons among more than 2 groups.
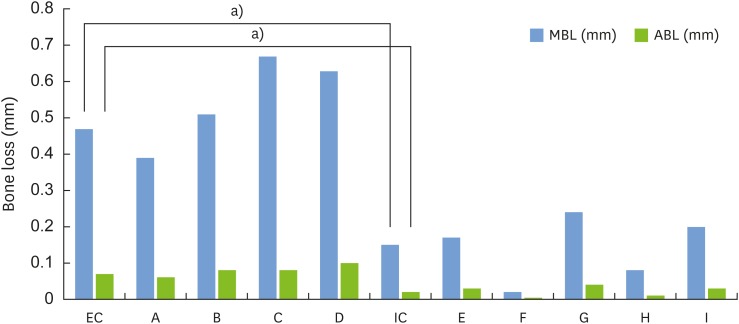
RESULTS
A total of 355 implants in 170 patients (206 EC and 149 IC) fulfilled the inclusion criteria and were analyzed in this study. The mean MBL was 0.47 mm and 0.15 mm in the EC and IC implants, respectively, which was a statistically significant difference (P < 0.001). Comparisons according to splinting (MBL of single implants: 0.34 mm, MBL of splinted implants: 0.31 mm, P=0.676) and cement use (MBL of cemented implants: 0.27 mm, MBL of non-cemented implants: 0.35 mm, P=0.178) showed no statistically significant differences in MBL, regardless of the implant connection type.
CONCLUSIONS
IC implants showed a more favorable bone response regarding MBL in posterior areas without peri-implantitis or periodontal disease.
MeSH Terms
Figure
Reference
-
1. Aparna IN, Dhanasekar B, Lingeshwar D, Gupta L. Implant crest module: a review of biomechanical considerations. Indian J Dent Res. 2012; 23:257–263. PMID: 22945720.
Article2. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981; 10:387–416. PMID: 6809663.
Article3. Goiato MC, Pellizzer EP, da Silva EV, Bonatto LR, dos Santos DM. Is the internal connection more efficient than external connection in mechanical, biological, and esthetical point of views? A systematic review. Oral Maxillofac Surg. 2015; 19:229–242. PMID: 25910993.
Article4. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25. PMID: 3527955.5. Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G. Long-term survival and success of oral implants in the treatment of full and partial arches: a 7-year prospective study with the ITI dental implant system. Int J Oral Maxillofac Implants. 2004; 19:247–259. PMID: 15101597.6. Laine P, Salo A, Kontio R, Ylijoki S, Lindqvist C, Suuronen R. Failed dental implants - clinical, radiological and bacteriological findings in 17 patients. J Craniomaxillofac Surg. 2005; 33:212–217. PMID: 15878525.
Article7. Behneke A, Behneke N, d'Hoedt B. A 5-year longitudinal study of the clinical effectiveness of ITI solid-screw implants in the treatment of mandibular edentulism. Int J Oral Maxillofac Implants. 2002; 17:799–810. PMID: 12507239.8. Assenza B, Scarano A, Petrone G, Iezzi G, Thams U, San Roman F, et al. Osteoclast activity around loaded and unloaded implants: a histological study in the beagle dog. J Oral Implantol. 2003; 29:1–7. PMID: 12614078.
Article9. Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010; 81:1350–1366. PMID: 20575657.
Article10. Jones AA, Cochran DL. Consequences of implant design. Dent Clin North Am. 2006; 50:339–360. vPMID: 16818019.
Article11. Hermann JS, Buser D, Schenk RK, Schoolfield JD, Cochran DL. Biologic Width around one- and two-piece titanium implants. Clin Oral Implants Res. 2001; 12:559–571. PMID: 11737099.
Article12. Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants: a methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001; 16:475–485. PMID: 11515994.13. Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001; 72:1372–1383. PMID: 11699479.
Article14. Misch CE. Generic root form component terminology. In : Misch CE, editor. Contemporary implant dentistry. 3rd ed. St Louis (MO): Mosby;2008. p. 2638.15. Schwarz F, Alcoforado G, Nelson K, Schaer A, Taylor T, Beuer F, et al. Impact of implant-abutment connection, positioning of the machined collar/microgap, and platform switching on crestal bone level changes. Camlog Foundation Consensus Report. Clin Oral Implants Res. 2014; 25:1301–1303. PMID: 24147913.
Article16. Pieri F, Aldini NN, Marchetti C, Corinaldesi G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: a randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2011; 26:169–178. PMID: 21365053.17. Koo KT, Lee EJ, Kim JY, Seol YJ, Han JS, Kim TI, et al. The effect of internal versus external abutment connection modes on crestal bone changes around dental implants: a radiographic analysis. J Periodontol. 2012; 83:1104–1109. PMID: 22145806.
Article18. Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006; 21:789–794. PMID: 17066642.19. Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin Oral Implants Res. 1992; 3:104–111. PMID: 1290790.20. Prendergast PJ, Huiskes R. Microdamage and osteocyte-lacuna strain in bone: a microstructural finite element analysis. J Biomech Eng. 1996; 118:240–246. PMID: 8738790.
Article21. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995; 74:51–55. PMID: 7674191.
Article22. Maeda Y, Satoh T, Sogo M. In vitro differences of stress concentrations for internal and external hex implant-abutment connections: a short communication. J Oral Rehabil. 2006; 33:75–78. PMID: 16409521.23. Laurell L, Lundgren D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res. 2011; 13:19–28. PMID: 19681932.
Article24. Vigolo P, Zaccaria M. Clinical evaluation of marginal bone level change of multiple adjacent implants restored with splinted and nonsplinted restorations: a 5-year prospective study. Int J Oral Maxillofac Implants. 2010; 25:1189–1194. PMID: 21197497.25. Vigolo P, Mutinelli S, Zaccaria M, Stellini E. Clinical evaluation of marginal bone level change around multiple adjacent implants restored with splinted and nonsplinted restorations: a 10-year randomized controlled trial. Int J Oral Maxillofac Implants. 2015; 30:411–418. PMID: 25830402.
Article26. Guichet DL, Caputo AA, Choi H, Sorensen JA. Passivity of fit and marginal opening in screw- or cement-retained implant fixed partial denture designs. Int J Oral Maxillofac Implants. 2000; 15:239–246. PMID: 10795456.27. Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 2012; 23(Suppl 6):163–201. PMID: 23062142.
Article28. Zechner W, Watzak G, Gahleitner A, Busenlechner D, Tepper G, Watzek G. Rotational panoramic versus intraoral rectangular radiographs for evaluation of peri-implant bone loss in the anterior atrophic mandible. Int J Oral Maxillofac Implants. 2003; 18:873–878. PMID: 14696663.29. Kullman L, Al-Asfour A, Zetterqvist L, Andersson L. Comparison of radiographic bone height assessments in panoramic and intraoral radiographs of implant patients. Int J Oral Maxillofac Implants. 2007; 22:96–100.30. Fickl S, Zuhr O, Stein JM, Hürzeler MB. Peri-implant bone level around implants with platform-switched abutments. Int J Oral Maxillofac Implants. 2010; 25:577–581. PMID: 20556258.31. Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008; 28:347–355. PMID: 18717373.32. Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching: is there any biomechanical rationale? Clin Oral Implants Res. 2007; 18:581–584. PMID: 17608737.
Article33. Padial-Molina M, Suarez F, Rios HF, Galindo-Moreno P, Wang HL. Guidelines for the diagnosis and treatment of peri-implant diseases. Int J Periodontics Restorative Dent. 2014; 34:e102–11. PMID: 25411744.
Article34. Sanz M, Chapple IL. Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012; 39(Suppl 12):202–206. PMID: 22533957.35. Sadowsky SJ. The implant-supported prosthesis for the edentulous arch: design considerations. J Prosthet Dent. 1997; 78:28–33. PMID: 9237143.
Article36. Heckmann SM, Winter W, Meyer M, Weber HP, Wichmann MG. Overdenture attachment selection and the loading of implant and denture-bearing area. Part 2: a methodical study using five types of attachment. Clin Oral Implants Res. 2001; 12:640–647. PMID: 11737109.
Article37. Naert I, Duyck J, Vandamme K. Occlusal overload and bone/implant loss. Clin Oral Implants Res. 2012; 23(Suppl 6):95–107.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of crown-to-implant ratio on periimplant marginal bone loss in the posterior region: a five-year retrospective study
- Retrospective study on marginal bone resorption around immediately loaded implants
- Success rate and marginal bone loss of Osstem USII plus implants; Short term clinical study
- Factors associated with the survival and marginal bone loss of dental implants: a 5-year retrospective study
- Marginal bone level changes in association with different vertical implant positions: a 3-year retrospective study