The prevalence of primary hyperparathyroidism in Korea: a population-based analysis from patient medical records
- Affiliations
-
- 1Department of Surgery, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 2Department of Surgery, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea. kevinjoon@naver.com
- 3Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 5Department of Internal Medicine, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea.
- 6Department of Urology, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2410266
- DOI: http://doi.org/10.4174/astr.2018.94.5.235
Abstract
- PURPOSE
Because primary hyperparathyroidism (PHPT) is difficult to recognize, it has a high likelihood of being underdiagnosed. In this study, we estimated the incidence of PHPT and evaluated PHPT diagnosis in Korea.
METHODS
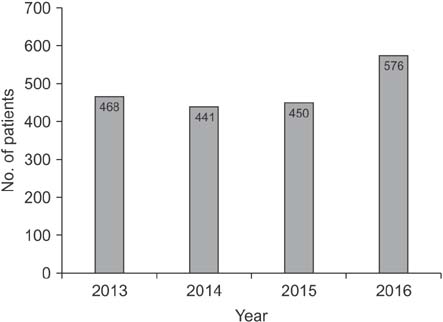
To calculate the prevalence of PHPT, we examined the medical records of patients that were hospitalized for urolithiasis between 2013 and 2016 at a single institute, and then identified those who were diagnosed with PHPT from the same group. A Korea-wide insurance claim database was used to ascertain the number of urolithiasis patients and the number of parathyroidectomies performed in Korea. The incidence of PHPT in the Korean population was estimated using the ratio of patients who presented with urolithiasis as the initial symptom of PHPT.
RESULTS
During the 4-year study period, 4 patients from the 925 urolithiasis patients enrolled in this study (0.4%) were diagnosed with PHPT. During this same period, there were 85,267 patients with urolithiasis in Korea, and the estimated number of PHPT patients was 341, which was 0.4% of 85,267. Considering that 12% to 23% of patients with PHPT are initially diagnosed with urolithiasis, the total number of PHPT patients was estimated to range from 1,483 to 2,842. The number of patients who underwent parathyroidectomy due to PHPT was 1,935 during the study period.
CONCLUSION
The number of patients we estimated to have PHPT corresponded closely with the number of patients undergoing parathyroidectomy during the study period. Considering the number of nonsymptomatic PHPT patients, PHPT may be properly diagnosed in Korea.
MeSH Terms
Figure
Cited by 3 articles
-
Changing Trends in Preoperative Localization and Surgical Techniques for the Treatment of Primary Hyperparathyroidism in a Single Tertiary Center
Jumyung Lee, Su-jin Kim, Hyeong Won Yu, Young Jun Chai, June Young Choi, Kyu Eun Lee
J Endocr Surg. 2019;19(4):126-135. doi: 10.16956/jes.2019.19.4.126.Parathyroid Cancer: Comparison with Benign Hyperparathyroidism
Jae Yeon Seok, Joon-Hyop Lee, Sihoon Lee, Suk Ha Kang, Yoo Seung Chung
J Endocr Surg. 2019;19(2):35-44. doi: 10.16956/jes.2019.19.2.35.Comparisons Between Normocalcemic Primary Hyperparathyroidism and Typical Primary Hyperparathyroidism
Hye Ryeon Choi, Sun Hyung Choi, Namki Hong, Yumie Rhee, Jin Kyong Kim, Cho Rok Lee, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung
J Korean Med Sci. 2022;37(13):e99. doi: 10.3346/jkms.2022.37.e99.
Reference
-
1. Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011; 365:2389–2397.2. Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014; 99:3561–3569.
Article3. Gopinath P, Mihai R. Hyperparathyroidism. Surgery. 2011; 29:451–458.
Article4. Bargren AE, Repplinger D, Chen H, Sippel RS. Can biochemical abnormalities predict symptomatology in patients with primary hyperparathyroidism. J Am Coll Surg. 2011; 213:410–414.
Article5. Boonstra CE, Jackson CE. Serum calcium survey for hyperparathyroidism: results in 50,000 clinic patients. Am J Clin Pathol. 1971; 55:523–526.
Article6. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006; 21:171–177.
Article7. Han SJ, Kim DK, Woo SU, Kim JH, Nam SJ, Yang JH. Clinical review of primary hyperparathyroidism. Korean J Endocr Surg. 2004; 4:42–47.
Article8. Bae JH, Choi HJ, Lee Y, Moon MK, Park YJ, Shin CS, et al. Preoperative predictive factors for parathyroid carcinoma in patients with primary hyperparathyroidism. J Korean Med Sci. 2012; 27:890–895.
Article9. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008.
Article10. Carneiro-Pla DM, Irvin GL 3rd, Chen H. Consequences of parathyroidectomy in patients with “mild” sporadic primary hyperparathyroidism. Surgery. 2007; 142:795–799.
Article11. Hinnie J. The management of primary hyperparathyroidism. Scott Med J. 2013; 58:251–253.
Article12. Richert L, Trombetti A, Herrmann FR, Triponez F, Meier C, Robert JH, et al. Age and gender distribution of primary hyperparathyroidism and incidence of surgical treatment in a European country with a particularly high life expectancy. Swiss Med Wkly. 2009; 139:400–404.13. Abood A, Vestergaard P. Increasing incidence of primary hyperparathyroidism in Denmark. Dan Med J. 2013; 60:A4567.14. Yu N, Donnan PT, Murphy MJ, Leese GP. Epidemiology of primary hyperparathyroidism in Tayside, Scotland, UK. Clin Endocrinol (Oxf). 2009; 71:485–493.
Article15. Adami S, Marcocci C, Gatti D. Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res. 2002; 17 Suppl 2. N18–N23.16. Bilezikian JP, Meng X, Shi Y, Silverberg SJ. Primary hyperparathyroidism in women: a tale of two cities--New York and Beijing. Int J Fertil Womens Med. 2000; 45:158–165.17. Innes A, Catto GR, Reid I, Matheson NA. The infrequency of primary hyperparathyroidism in north-east Scotland. J R Coll Surg Edinb. 1987; 32:263–266.18. Bolland MJ, Grey AB, Gamble GD, Reid IR. Association between primary hyperparathyroidism and increased body weight: a meta-analysis. J Clin Endocrinol Metab. 2005; 90:1525–1530.
Article19. Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond). 2008; 32:1431–1437.
Article20. Berger AD, Wu W, Eisner BH, Cooperberg MR, Duh QY, Stoller ML. Patients with primary hyperparathyroidism--why do some form stones. J Urol. 2009; 181:2141–2145.
Article21. Elkoushy MA, Yu AX, Tabah R, Payne RJ, Dragomir A, Andonian S. Determinants of urolithiasis before and after parathyroidectomy in patients with primary hyperparathyroidism. Urology. 2014; 84:22–26.
Article22. Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab. 2008; 93:3462–3470.
Article23. Yeh MW, Wiseman JE, Ituarte PH, Pasternak JD, Hwang RS, Wu B, et al. Surgery for primary hyperparathyroidism: are the consensus guidelines being followed? Ann Surg. 2012; 255:1179–1183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple brown tumors in a patient with primary hyperparathyroidism
- Primary hyperparathyroidism erosion of the sternal ends of the clavicles, a new sign of hyperparathyroidism: a case report
- Thyroid Nodules in Patients with Secondary Hyperparathyroidism
- A Case of Primary Hyperparathyroidism Associated with Hypercalcemic Crisis and Systemic Calcinosis
- Primary Hyperparathyroidism in Recurrent Urolithiasis: 1 Case