J Korean Acad Prosthodont.
2018 Apr;56(2):105-113. 10.4047/jkap.2018.56.2.105.
Three-dimensional finite element analysis according to the insertion depth of an immediately loaded implant in the anterior maxilla
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea. proshan@snu.ac.kr
- KMID: 2410113
- DOI: http://doi.org/10.4047/jkap.2018.56.2.105
Abstract
- PURPOSE
The purpose of this study was to investigate the effects of the insertion depth of an immediately loaded implant on the stress distribution of the surrounding bone and the micromovement of the implant using the three-dimensional finite element analysis.
MATERIALS AND METHODS
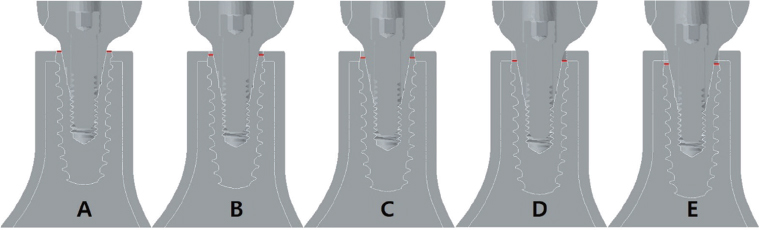
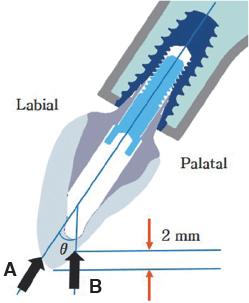
A total of five bone models were constructed such that the implant platform was positioned at the levels of 0.00 mm, 0.25 mm, 0.50 mm, 0.75 mm, and 1.00 mm depth from the crest of the cortical bone. A frictional coefficient of 0.3 and the insertion torque of 35 Ncm were simulated on the interface between the implant and surrounding bone. A static load of 178 N was applied to the provisional prosthesis with a vertical load in the axial direction and an oblique load at 30°with respect to the central axis of the implant, then a finite element analysis was performed.
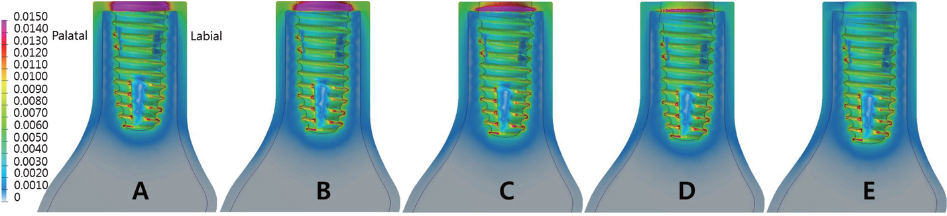
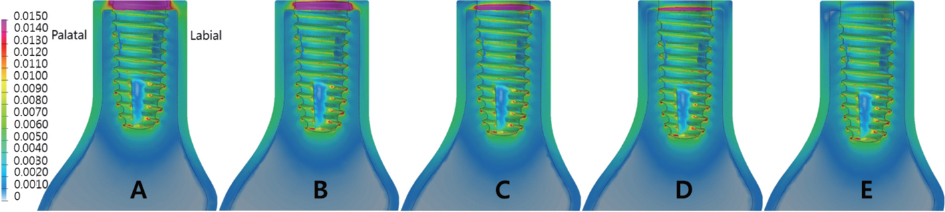
RESULTS
The implant insertion depth significantly affected the stress distribution on the surrounding bone. The largest micromovement value of the implant was 39.34 µm. The oblique load contributed significantly to the stress distribution and micromovement in comparison to the vertical load.
CONCLUSION
Increasing the implant insertion depth was advantageous in dispersing the concentrated stress in the cortical bone and did not significantly affect the micromovement associated with early osseointegration failure.
MeSH Terms
Figure
Reference
-
1. Rodriguez AM, Rosenstiel SF. Esthetic considerations related to bone and soft tissue maintenance and development around dental implants: report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. J Prosthet Dent. 2012; 108:259–267.
Article2. Misch CE, Wang HL, Misch CM, Sharawy M, Lemons J, Judy KW. Rationale for the application of immediate load in implant dentistry: Part I. Implant Dent. 2004; 13:207–217.
Article3. Cooper LF, De Kok IJ, Rojas-Vizcaya F, Pungpapong P, Chang SH. The immediate loading of dental implants. Compend Contin Educ Dent. 2007; 28:216–225. quiz 226.4. Mangano FG, Mastrangelo P, Luongo F, Blay A, Tunchel S, Mangano C. Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: a retrospective study on 103 patients with 3 years of follow-up. Clin Oral Implants Res. 2017; 28:272–282.
Article5. den Hartog L, Raghoebar GM, Stellingsma K, Vissink A, Meijer HJ. Immediate loading of anterior single-tooth implants placed in healed sites: Five-year results of a randomized clinical trial. Int J Prosthodont. 2016; 29:584–591.
Article6. den Hartog L, Raghoebar GM, Stellingsma K, Vissink A, Meijer HJ. Immediate non-occlusal loading of single implants in the aesthetic zone: a randomized clinical trial. J Clin Periodontol. 2011; 38:186–194.
Article7. Cooper LF, Reside GJ, Raes F, Garriga JS, Tarrida LG, Wiltfang J, Kern M, De Bruyn H. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: a 5-year prospective evaluation. Int J Oral Maxillofac Implants. 2014; 29:709–717.
Article8. Ding X, Zhu XH, Liao SH, Zhang XH, Chen H. Implant-bone interface stress distribution in immediately loaded implants of different diameters: a three-dimensional finite element analysis. J Prosthodont. 2009; 18:393–402.
Article9. Kao HC, Gung YW, Chung TF, Hsu ML. The influence of abutment angulation on micromotion level for immediately loaded dental implants: a 3-D finite element analysis. Int J Oral Maxillofac Implants. 2008; 23:623–630.10. Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010; 38:612–620.
Article11. Cassetta M, Driver A, Brandetti G, Calasso S. Peri-implant bone loss around platform-switched Morse taper connection implants: a prospective 60-month follow-up study. Int J Oral Maxillofac Surg. 2016; 45:1577–1585.
Article12. Chu CM, Hsu JT, Fuh LJ, Huang HL. Biomechanical evaluation of subcrestal placement of dental implants: in vitro and numerical analyses. J Periodontol. 2011; 82:302–310.
Article13. Chou HY, Müftü S, Bozkaya D. Combined effects of implant insertion depth and alveolar bone quality on periimplant bone strain induced by a wide-diameter, short implant and a narrow-diameter, long implant. J Prosthet Dent. 2010; 104:293–300.
Article14. León J, Carrascosa A, Rodríguez X, Ruiz-Magaz V, Pascual A, Nart J. Finite element analysis relative to the crestal position of a 3.0-mm-diameter implant. Int J Periodontics Restorative Dent. 2014; 34:381–387.
Article15. Huang CC, Lan TH, Lee HE, Wang CH. The biomechanical analysis of relative position between implant and alveolar bone: finite element method. J Periodontol. 2011; 82:489–496.
Article16. Rismanchian M, Askari N, Shafiei S. The effect of placement depth of platform-switched implants on periimplant cortical bone stress: a 3-dimensional finite element analysis. Implant Dent. 2013; 22:165–169.
Article17. Qian L, Todo M, Matsushita Y, Koyano K. Effects of implant diameter, insertion depth, and loading angle on stress/strain fields in implant/jawbone systems: finite element analysis. Int J Oral Maxillofac Implants. 2009; 24:877–886.18. Dos Santos MBF, Meloto GO, Bacchi A, Correr-Sobrinho L. Stress distribution in cylindrical and conical implants under rotational micromovement with different boundary conditions and bone properties: 3-D FEA. Comput Methods Biomech Biomed Engin. 2017; 20:893–900.
Article19. Borie E, Orsi IA, Noritomi PY, Kemmoku DT. Three-Dimensional Finite Element Analysis of the Biomechanical Behaviors of Implants with Different Connections, Lengths, and Diameters Placed in the Maxillary Anterior Region. Int J Oral Maxillofac Implants. 2016; 31:101–110.
Article20. Bal BT, Cağlar A, Aydin C, Yilmaz H, Bankoğlu M, Eser A. Finite element analysis of stress distribution with splinted and nonsplinted maxillary anterior fixed prostheses supported by zirconia or titanium implants. Int J Oral Maxillofac Implants. 2013; 28:e27–e38.
Article21. Lee JS, Cho IH, Kim YS, Heo SJ, Kwon HB, Lim YJ. Bone-implant interface with simulated insertion stress around an immediately loaded dental implant in the anterior maxilla: a three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2012; 27:295–302.22. Hsu ML, Chen FC, Kao HC, Cheng CK. Influence of off-axis loading of an anterior maxillary implant: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2007; 22:301–309.23. Santiago Junior JF, Pellizzer EP, Verri FR, de Carvalho PS. Stress analysis in bone tissue around single implants with different diameters and veneering materials: a 3-D finite element study. Mater Sci Eng C Mater Biol Appl. 2013; 33:4700–4714.
Article24. Verri FR, Santiago Júnior JF, Almeida DA, Verri AC, Batista VE, Lemos CA, Noritomi PY, Pellizzer EP. Three-dimensional finite element analysis of anterior single implant-supported prostheses with different bone anchorages. ScientificWorldJournal. 2015; 2015:321528.
Article25. Tahmaseb A, De Clerck R, Aartman I, Wismeijer D. Digital protocol for reference-based guided surgery and immediate loading: a prospective clinical study. Int J Oral Maxillofac Implants. 2012; 27:1258–1270.
Article26. Attard NJ, Zarb GA. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005; 94:242–258.
Article27. Okumura N, Stegaroiu R, Kitamura E, Kurokawa K, Nomura S. Influence of maxillary cortical bone thickness, implant design and implant diameter on stress around implants: a three-dimensional finite element analysis. J Prosthodont Res. 2010; 54:133–142.
Article28. Sugiura T, Yamamoto K, Horita S, Murakami K, Tsutsumi S, Kirita T. The effects of bone density and crestal cortical bone thickness on micromotion and peri-implant bone strain distribution in an immediately loaded implant: a nonlinear finite element analysis. J Periodontal Implant Sci. 2016; 46:152–165.
Article29. Brunski JB. Avoid pitfalls of overloading and micromotion of intraosseous implants. Dent Implantol Update. 1993; 4:77–81.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Finite element analysis on stress distribution of maxillary implant-retained overdentures depending on the Bar attachment design and palatal coverage
- Effects of implant tilting and the loading direction on the displacement and micromotion of immediately loaded implants: an in vitro experiment and finite element analysis
- Three-dimensional finite element analysis for stress distribution on the diameter of orthodontic mini-implants and insertion angle to the bone surface
- The effects of bone density and crestal cortical bone thickness on micromotion and peri-implant bone strain distribution in an immediately loaded implant: a nonlinear finite element analysis
- EFFECTS OF BONE ENGAGEMENT TYPE&IMPLANT LENGTH ON STRESS DISTRIBUTION: A THREE DIMENSIONAL FINITE ELEMENT ANALYSIS