Clin Nutr Res.
2018 Apr;7(2):146-152. 10.7762/cnr.2018.7.2.146.
Nutrition Intervention through Interdisciplinary Medical Treatment in Hospice Patients: From Admission to Death
- Affiliations
-
- 1Department of Nutrition, Yeouido St. Mary's Hospital, The Catholic University of Korea, Seoul 07345, Korea. 21602873@cmcnu.or.kr
- KMID: 2409993
- DOI: http://doi.org/10.7762/cnr.2018.7.2.146
Abstract
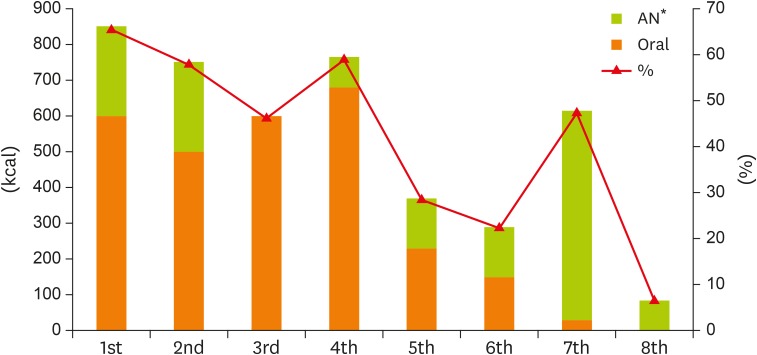
- The demand for hospice services as well as for "˜well-dying' of terminal patients is increasing as patient financial burden is decreasing due to National Health Insurance coverage for hospice care. Hospice institutions utilize interdisciplinary teams comprising doctors, nurses, dietitians, and other health staffs to provide comprehensive patient management. This report examined the nutritional status of a hospice patient from admission to death as well as the nutrition management of this patient in the hospice ward through nutrition interventions performed by a dietitian in the interdisciplinary team. The patient in the present case was a 74-year-old man diagnosed with pancreatic head cancer who died after 26 days of hospice care following transfer from the general ward. During hospice care, the dietitian monitored the patient's nutritional status and performed 8 nutrition interventions, but his oral intake decreased as the patient's symptoms worsened. The average energy intake rates were 30% and 17% of required rates for oral and artificial nutrition, respectively. In line with a report suggesting that the main focus of nutrition in palliative care should be on improving the quality of life and reducing worry in patients, rather than aggressive nutritional management, there is a need for nutrition interventions that are personalized to individual patients by monitoring progress and offering continuous counseling from the time of admission. In addition, further studies such as comparative analysis of nutritional management in Korean hospice ward will be needed for better nutrition management for terminally ill patients.
MeSH Terms
Figure
Reference
-
1. Kim CG. Hospice & palliative care policy in Korea. Korean J Hosp Palliat Care. 2017; 20:8–17.2. Doyle D, Woodruff R. The IAHPC manual of palliative care. 2nd ed. Houston (TX): IAHPC Press;2008.3. Hui D, Dev R, Bruera E. The last days of life: symptom burden and impact on nutrition and hydration in cancer patients. Curr Opin Support Palliat Care. 2015; 9:346–354. PMID: 26509860.4. Marley K, Cunningham KA. Food for thought: improving nutritional assessment and management in the hospice setting. [abstract]. BMJ Support Palliat Care. 2015; 5(Suppl 3):A28.5. Compassion and Support at the End of Life (US). Signs of dying [Internet]. 2009. cited 2017 November 15. Available from https://www.compassionandsupport.org/index.php/for_patients_families/death_dying/signs_of_dying.6. Bosaeus I, Daneryd P, Svanberg E, Lundholm K. Dietary intake and resting energy expenditure in relation to weight loss in unselected cancer patients. Int J Cancer. 2001; 93:380–383. PMID: 11433403.
Article7. Adelaide Hills Community Health Service (AU). Diet and nutrition in palliative care: a guide for clients and carers. Mount Barker: Adelaide Hills Community Health Service;2012.8. Cimino JE. The role of nutrition in hospice and palliative care of the cancer patient. Topics Clin Nutr. 2003; 18:154–161.
Article9. Dalal S, Bruera E. Dehydration in cancer patients: to treat or not to treat. J Support Oncol. 2004; 2:467–479. PMID: 15605914.10. Shils ME, Shike M. Modern nutrition in health and disease. 10th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2006.11. Bozzetti F, Arends J, Lundholm K, Micklewright A, Zurcher G, Muscaritoli M. ESPEN. ESPEN guidelines on parenteral nutrition: non-surgical oncology. Clin Nutr. 2009; 28:445–454. PMID: 19477052.12. Kim DY, Lee SM, Lee KE, Lee HR, Kim JH, Lee KW, Lee JS, Lee SN. An evaluation of nutrition support for terminal cancer patients at teaching hospitals in Korea. Cancer Res Treat. 2006; 38:214–217. PMID: 19771245.
Article13. Raijmakers NJ, van Zuylen L, Costantini M, Caraceni A, Clark J, Lundquist G, Voltz R, Ellershaw JE, van der Heide A. OPCARE9. Artificial nutrition and hydration in the last week of life in cancer patients. A systematic literature review of practices and effects. Ann Oncol. 2011; 22:1478–1486. PMID: 21199887.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perception on Hospice, Attitudes toward Death and Needs of Hospice Care between the Patients with Cancer and Family
- A Comparative Study on Death Orientation and the Cognition & Nursing Needs of Hospice in Hospice Volunteers: a comparison between the trained and non trained volunteer
- A Study on the Death Orientation of Hospice Care Members
- Effects of Holistic Hospice Nursing Intervention Program on Self Esteem and Spiritual Well-being for Inpatients of Hospice Palliative Care Unit
- Comparison of Death Orientation of Nurses before and after Hospice Training Program