Perinatology.
2017 Dec;28(4):115-118. 10.14734/PN.2017.28.4.115.
Association of Cervical Length and Term Delivery after Elective Cerclage in Women with High Risk of Preterm Delivery
- Affiliations
-
- 1Department of Pediatrics, Soonchunhyang University Hospital, Soonchunhyang University School of Medicine, Seoul, Korea. ksyob@gilhospital.com
- KMID: 2409117
- DOI: http://doi.org/10.14734/PN.2017.28.4.115
Abstract
OBJECTIVE
To analyze the association between cervical length (CL) and term delivery after elective cerclage in women with high risk of preterm delivery.
METHODS
Medical records of 97 women with high risk of preterm delivery who underwent McDonald elective cerclage and delivered by a single surgeon between January 2003 and June 2012 were reviewed and analyzed. The subjects were grouped according to their preoperative CL as measured by ultrasonography, in which 2.5 cm was defined as short cervical length (SCL). We compared the clinical outcomes according to the SCL (≤2.5 cm vs. >2.5 cm) and predicted the optimal postoperative CL for term delivery after 37 weeks.
RESULTS
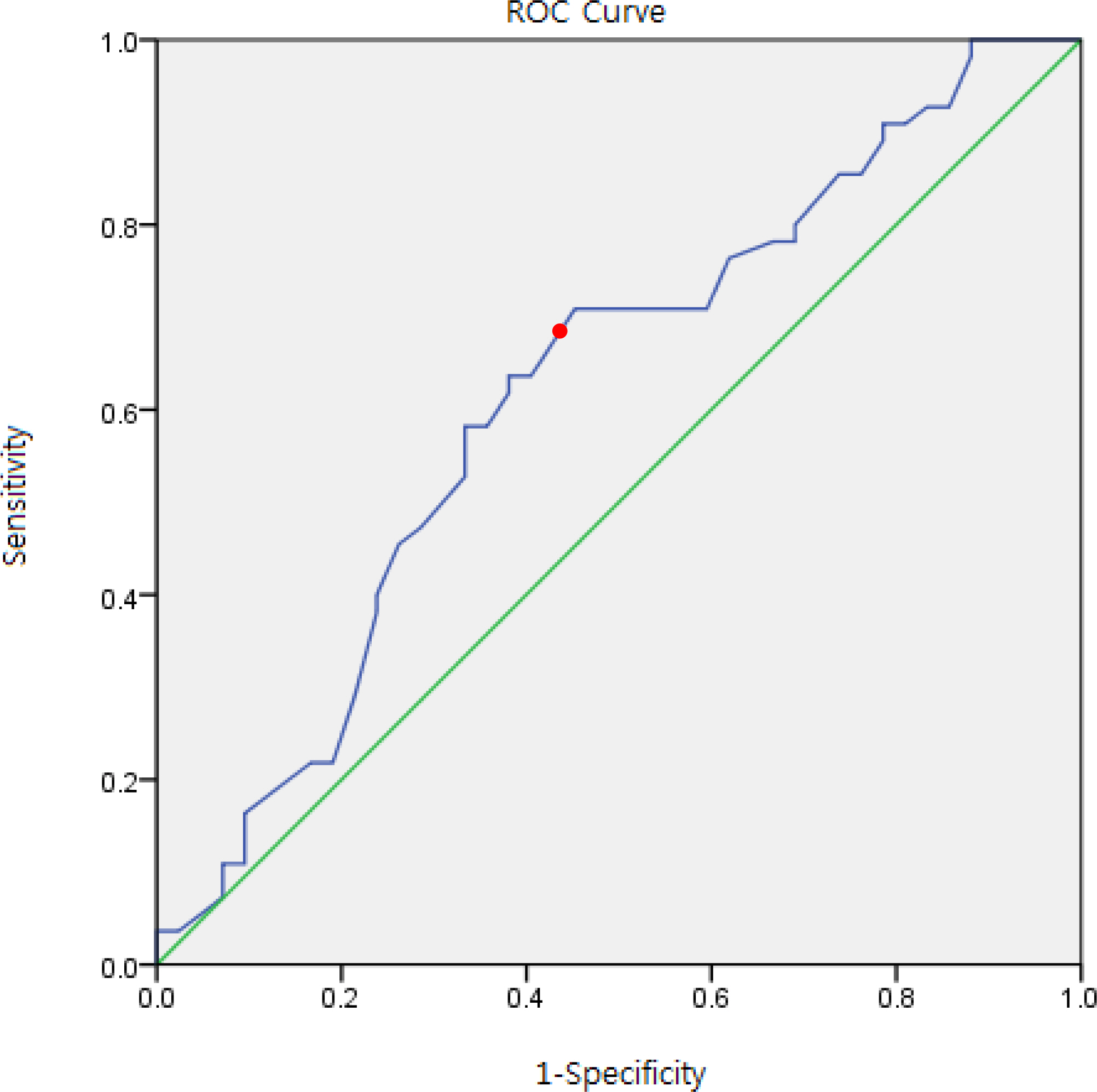
Postoperative CL significantly differed (2.8 cm vs. 3.3 cm, P=0.003) by the SCL (n=40, n=57), while gestational age at delivery did not differ significantly between the two groups. Two thirds of the subjects who had postoperative CL longer than 3.1 cm maintained pregnancy until 37 weeks (sensitivity: 64%, specificity: 65%). After adjusting for confounding factors, we found that postoperative CL longer than 3.1 cm was associated with an average gestation period of 37 weeks or more (odds ratio=2.6, 95% confidence interval 1.2-6.0).
CONCLUSION
Postoperative CL over 3.1 cm was associated with term delivery after 37 weeks.
Keyword
MeSH Terms
Figure
Reference
-
1). Martin JA., Hamilton BE., Osterman MJ., Curtin SC., Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015. 64:1–65.2). McDONALD IA. Suture of the cervix for inevitable miscarriage. J Obstet Gynaecol Br Emp. 1957. 64:346–50.
Article3). Abbott D., To M., Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012. 52:220–3.
Article4). Alfirevic Z., Stampalija T., Roberts D., Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012. 4:CD008991.
Article5). Iams JD., Goldenberg RL., Meis PJ., Mercer BM., Moawad A., Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996. 334:567–73.
Article6). Crane J., Hutchens D. Transvaginal sonographic measurement of cervical length to predict preterm birth in asymptomatic women at increased risk: a systematic review. Ultrasound Obstet Gynecol. 2008. 31:579–87.
Article7). Hassan S., Romero R., Vidyadhari D., Fusey S., Baxter JK., Khandelwal M, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double–blind, placebo–controlled trial. Ultrasound Obstet Gynecol. 2011. 38:18–31.
Article8). Guzman ER., Houlihan C., Vintzileos A., Ivan J., Benito C., Kappy K. The significance of transvaginal ultrasonographic evaluation of the cervix in women treated with emergency cerclage. Am J Obstet Gynecol. 1996. 175:471–6.
Article9). Andersen HF., Karimi A., Sakala EP., Kalugdan R. Prediction of cervical cerclage outcome by endovaginal ultrasonography. Am J Obstet Gynecol. 1994. 171:1102–6.
Article10). Althuisius SM., Dekker GA., van Geijn HP., Hummel P. The effect of therapeutic McDonald cerclage on cervical length as assessed by transvaginal ultrasonography. Am J Obstet Gynecol. 1999. 180(2 Pt 1):366–9.
Article11). Funai EF., Paidas MJ., Rebarber A., O'Neill L., Rosen TJ., Young BK. Change in cervical length after prophylactic cerclage. Obstet Gynecol. 1999. 94:117–9.
Article12). Berghella V., Figueroa D., Szychowski JM., Owen J., Hankins GD., Iams JD, et al. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010. 202:351. .e1-6.
Article13). Scheib S., Visintine JF., Miroshnichenko G., Harvey C., Rychlak K., Berghella V. Is cerclage height associated with the incidence of preterm birth in women with an ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009. 200:e12–5.
Article14). Groom KM., Shennan AH., Bennett PR. Ultrasound-indicated cervical cerclage: outcome depends on preoperative cervical length and presence of visible membranes at time of cerclage. Am J Obstet Gynecol. 2002. 187:445–9.
Article15). Dijkstra K., Funai EF., O'Neill L., Rebarber A., Paidas MJ., Young BK. Change in cervical length after cerclage as a predictor of preterm delivery. Obstet Gynecol. 2000. 96:346–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Association of Cervical Length and Term Delivery after Elective Cerclage in Women with High Risk of Preterm Delivery
- Post-cerclage ultrasonographic cervical length can predict preterm delivery in elective cervical cerclage patients
- The role of prophylactic cerclage in preventing preterm delivery after electrosurgical conization
- Change in cervical length after therapeutic McDonald cerclage using a transvaginal ultrasonography as a predictor of term delivery
- Pregnancy outcome after cervical conization: risk factors for preterm delivery and the efficacy of prophylactic cerclage