Allergy Asthma Immunol Res.
2018 May;10(3):225-235. 10.4168/aair.2018.10.3.225.
Perceptions of Severe Asthma and Asthma-COPD Overlap Syndrome Among Specialists: A Questionnaire Survey
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. hjyoon@hanyang.ac.kr
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pulmonary, Allergy and Critical Care Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea.
- 5Department of Internal Medicine, CHA University School of Medicine, Seongnam, Korea.
- 6Department of Internal Medicine, Hallym University College of Medicine, Anyang, Korea.
- 7Department of Internal Medicine, College of Medicine, Ewha Womans University, Seoul, Korea.
- 8Department of Internal Medicine, Inje University College of Medicine, Busan, Korea.
- 9Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yscho@amc.seoul.kr
- 10Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- 11Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 12Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 13Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 14Department of Internal Medicine, Konkuk University, School of Medicine, Seoul, Korea.
- 15Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 16Department of Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 17Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2409057
- DOI: http://doi.org/10.4168/aair.2018.10.3.225
Abstract
- PURPOSE
Severe asthma and asthma-chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) are difficult to control and are often associated with poor clinical outcomes. However, much is not understood regarding the diagnosis and treatment of severe asthma and ACOS. To evaluate the current perceptions of severe asthma and COPD among asthma and COPD specialists, we designed an e-mail and internet-based questionnaire survey.
METHODS
Subjects were selected based on clinical specialty from among the members of the Korean Academy of Asthma, Allergy and Clinical Immunology and the Korean Academy of Tuberculosis and Respiratory Diseases. Of 432 subjects who received an e-mail invitation to the survey, 95 subjects, including 58 allergists and 37 pulmonologists, responded and submitted their answers online.
RESULTS
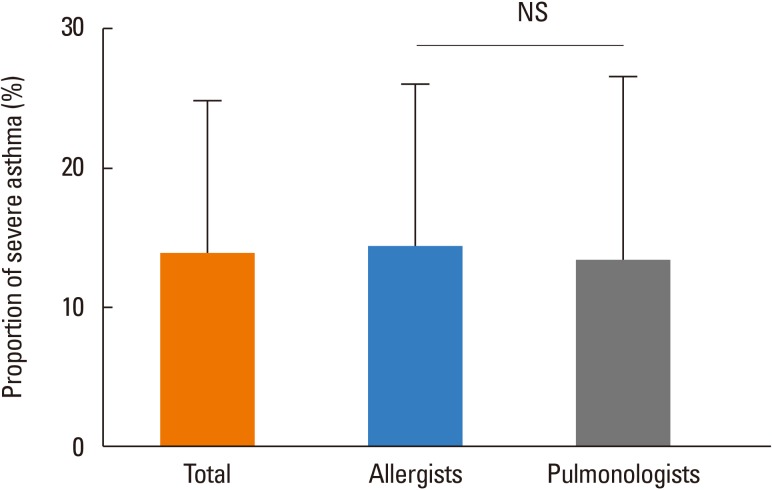
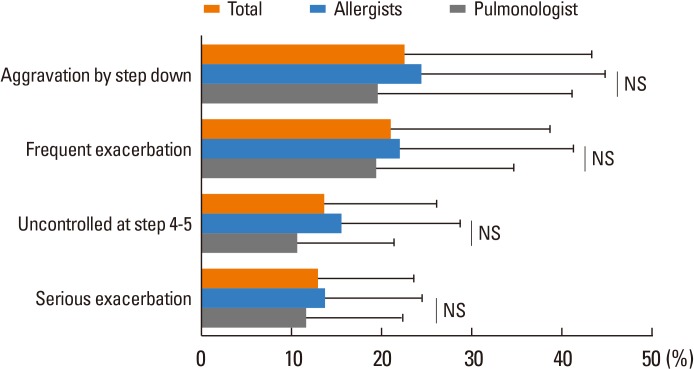
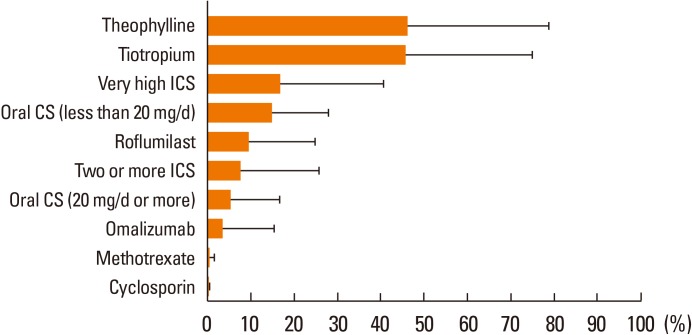
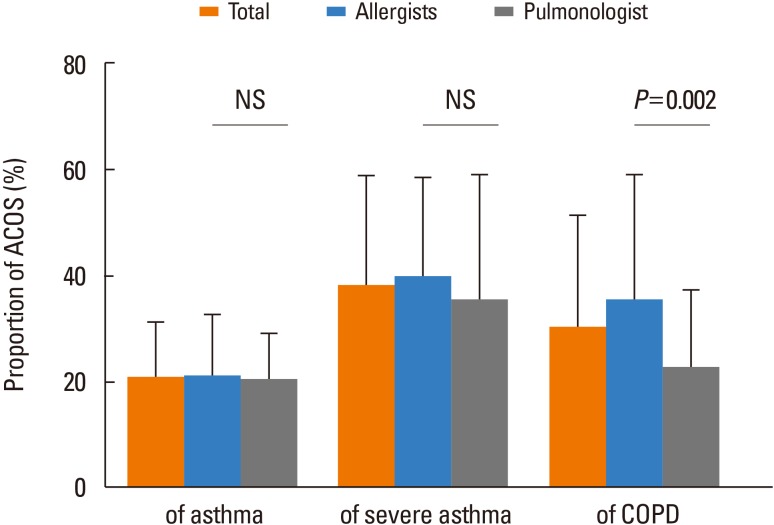
The specialists estimated that the percentage of severe cases among total asthma patients in their practice was 13.9%±11.0%. Asthma aggravation by stepping down treatment was the most common subtype, followed by frequent exacerbation, uncontrolled asthma despite higher treatment steps, and serious exacerbation. ACOS was estimated to account for 20.7% of asthma, 38.0% of severe asthma, and 30.1% of COPD cases. A history of smoking, persistently low forced expiratory volume in 1 second (FEV1), and low FEV1 variation were most frequently classified as the major criteria for the diagnosis of ACOS among asthma patients. Among COPD patients, the highly selected major criteria for ACOS were high FEV1 variation, positive bronchodilator response, a personal history of allergies and positive airway hyperresponsiveness. Allergists and pulmonologists showed different assessments and opinions on asthma phenotyping, percentage, and diagnostic criteria for ACOS.
CONCLUSIONS
Specialists had diverse perceptions and clinical practices regarding severe asthma and ACOS patients. This heterogeneity must be considered in future studies and strategy development for severe asthma and ACOS.
MeSH Terms
Figure
Cited by 1 articles
-
Biological treatments for severe asthma
Hyun Jung Jin
Yeungnam Univ J Med. 2020;37(4):262-268. doi: 10.12701/yujm.2020.00647.
Reference
-
1. Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014; 43:343–373. PMID: 24337046.2. Bousquet J, Mantzouranis E, Cruz AA, Aït-Khaled N, Baena-Cagnani CE, Bleecker ER, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010; 126:926–938. PMID: 20926125.
Article3. Custovic A, Johnston SL, Pavord I, Gaga M, Fabbri L, Bel EH, et al. EAACI position statement on asthma exacerbations and severe asthma. Allergy. 2013; 68:1520–1531. PMID: 24410781.
Article4. Sullivan SD, Wenzel SE, Bresnahan BW, Zheng B, Lee JH, Pritchard M, et al. Association of control and risk of severe asthma-related events in severe or difficult-to-treat asthma patients. Allergy. 2007; 62:655–660. PMID: 17508970.
Article5. Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009; 64:728–735. PMID: 19638566.
Article6. Zeki AA, Schivo M, Chan A, Albertson TE, Louie S. The asthma-COPD overlap syndrome: a common clinical problem in the elderly. J Allergy (Cairo). 2011; 2011:861926. PMID: 22121384.
Article7. Diaz-Guzman E, Khosravi M, Mannino DM. Asthma, chronic obstructive pulmonary disease, and mortality in the U.S. population. COPD. 2011; 8:400–407. PMID: 22149399.
Article8. Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011; 12:127. PMID: 21951550.
Article9. van Boven JF, Román-Rodríguez M, Palmer JF, Toledo-Pons N, Cosío BG, Soriano JB. Comorbidome, pattern, and impact of asthma-COPD overlap syndrome in real life. Chest. 2016; 149:1011–1020. PMID: 26836892.
Article10. Rhee CK, Yoon HK, Yoo KH, Kim YS, Lee SW, Park YB, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD. 2014; 11:163–170. PMID: 24111662.
Article11. Cazzola M, Rogliani P. Do we really need asthma-chronic obstructive pulmonary disease overlap syndrome? J Allergy Clin Immunol. 2016; 138:977–983. PMID: 27372569.
Article12. Reddel HK. Treatment of overlapping asthma-chronic obstructive pulmonary disease: can guidelines contribute in an evidence-free zone? J Allergy Clin Immunol. 2015; 136:546–552. PMID: 26343938.
Article13. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention [Internet]. [place unknown]: Global Initiative for Asthma;2017. cited 2017 Aug 12. Available from: http://www.ginasthma.org.14. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of COPD [Internet]. [place unknown]: Global Initiative for Chronic Obstructive Lung Disease;2017. cited 2017 Aug 12. Available from: http://www.goldcopd.org/.15. American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000; 162:2341–2351. PMID: 11112161.16. von Bülow A, Kriegbaum M, Backer V, Porsbjerg C. The prevalence of severe asthma and low asthma control among Danish adults. J Allergy Clin Immunol Pract. 2014; 2:759–767. PMID: 25439368.
Article17. Hekking PP, Wener RR, Amelink M, Zwinderman AH, Bouvy ML, Bel EH. The prevalence of severe refractory asthma. J Allergy Clin Immunol. 2015; 135:896–902. PMID: 25441637.
Article18. Varsano S, Segev D, Shitrit D. Severe and non-severe asthma in the community: a large electronic database analysis. Respir Med. 2017; 123:131–139. PMID: 28137489.
Article19. Kim TB, Park CS, Bae YJ, Cho YS, Moon HB. COREA Study Group. Factors associated with severity and exacerbation of asthma: a baseline analysis of the cohort for reality and evolution of adult asthma in Korea (COREA). Ann Allergy Asthma Immunol. 2009; 103:311–317. PMID: 19852195.
Article20. Chung KF, Godard P, Adelroth E, Ayres J, Barnes N, Barnes P, et al. ERS Task Force on Difficult/Therapy-Resistant Asthma. Difficult/therapy-resistant asthma: the need for an integrated approach to define clinical phenotypes, evaluate risk factors, understand pathophysiology and find novel therapies. Eur Respir J. 1999; 13:1198–1208. PMID: 10414427.21. Wenzel S. Severe asthma: from characteristics to phenotypes to endotypes. Clin Exp Allergy. 2012; 42:650–658. PMID: 22251060.
Article22. Fajt ML, Wenzel SE. Development of new therapies for severe asthma. Allergy Asthma Immunol Res. 2017; 9:3–14. PMID: 27826957.
Article23. Chung KF. Asthma phenotyping: a necessity for improved therapeutic precision and new targeted therapies. J Intern Med. 2016; 279:192–204. PMID: 26076339.
Article24. O'Neill S, Sweeney J, Patterson CC, Menzies-Gow A, Niven R, Mansur AH, et al. The cost of treating severe refractory asthma in the UK: an economic analysis from the British Thoracic Society Difficult Asthma Registry. Thorax. 2015; 70:376–378. PMID: 24917087.25. Menzella F, Galeone C, Formisano D, Castagnetti C, Ruggiero P, Simonazzi A, et al. Real-life efficacy of omalizumab after 9 years of follow-up. Allergy Asthma Immunol Res. 2017; 9:368–372. PMID: 28497924.
Article26. Caminati M, Senna G, Stefanizzi G, Bellamoli R, Longhi S, Chieco-Bianchi F, et al. Drop-out rate among patients treated with omalizumab for severe asthma: Literature review and real-life experience. BMC Pulm Med. 2016; 16:128. PMID: 27562427.
Article27. Ferrando M, Bagnasco D, Varricchi G, Bernardi S, Bragantini A, Passalacqua G, et al. Personalized medicine in allergy. Allergy Asthma Immunol Res. 2017; 9:15–24. PMID: 27826958.
Article28. Gibson PG, McDonald VM. Asthma-COPD overlap 2015: now we are six. Thorax. 2015; 70:683–691. PMID: 25948695.
Article29. Wurst KE, Kelly-Reif K, Bushnell GA, Pascoe S, Barnes N. Understanding asthma-chronic obstructive pulmonary disease overlap syndrome. Respir Med. 2016; 110:1–11. PMID: 26525374.
Article30. Jo YS, Lee J, Yoon HI, Kim DK, Yoo CG, Lee CH. Different prevalence and clinical characteristics of asthma-chronic obstructive pulmonary disease overlap syndrome according to accepted criteria. Ann Allergy Asthma Immunol. 2017; 118:696–703.e1. PMID: 28583262.
Article31. Soler-Cataluña JJ, Cosío B, Izquierdo JL, López-Campos JL, Marín JM, Agüero R, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012; 48:331–337. PMID: 22341911.
Article32. Menezes AM, Montes de, Pérez-Padilla R, Nadeau G, Wehrmeister FC, Lopez-Varela MV, et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014; 145:297–304. PMID: 24114498.33. Kankaanranta H, Harju T, Kilpeläinen M, Mazur W, Lehto JT, Katajisto M, et al. Diagnosis and pharmacotherapy of stable chronic obstructive pulmonary disease: the finnish guidelines. Basic Clin Pharmacol Toxicol. 2015; 116:291–307. PMID: 25515181.
Article34. Sin DD, Miravitlles M, Mannino DM, Soriano JB, Price D, Celli BR, et al. What is asthma-COPD overlap syndrome? Towards a consensus definition from a round table discussion. Eur Respir J. 2016; 48:664–673. PMID: 27338195.
Article35. Perret JL, Dharmage SC, Matheson MC, Johns DP, Gurrin LC, Burgess JA, et al. The interplay between the effects of lifetime asthma, smoking, and atopy on fixed airflow obstruction in middle age. Am J Respir Crit Care Med. 2013; 187:42–48. PMID: 23155143.36. Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011; 139:752–763. PMID: 20884729.37. Gelb AF, Yamamoto A, Verbeken EK, Nadel JA. Unraveling the pathophysiology of the asthma-copd overlap syndrome: unsuspected mild centrilobular emphysema is responsible for loss of lung elastic recoil in never smokers with asthma with persistent expiratory airflow limitation. Chest. 2015; 148:313–320. PMID: 25950858.38. Sin DD. Asthma-COPD Overlap syndrome: what we know and what we don't. Tuberc Respir Dis. 2017; 80:11–20.
Article39. Tkacova R, Dai DL, Vonk JM, Leung JM, Hiemstra PS, van den Berge M, et al. Airway hyperresponsiveness in chronic obstructive pulmonary disease: a marker of asthma-chronic obstructive pulmonary disease overlap syndrome? J Allergy Clin Immunol. 2016; 138:1571–1579.e10. PMID: 27345171.40. Shaaban R, Zureik M, Soussan D, Neukirch C, Heinrich J, Sunyer J, et al. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet. 2008; 372:1049–1057. PMID: 18805333.
Article41. Postma DS, Rabe KF. The asthma-COPD overlap syndrome. N Engl J Med. 2015; 373:1241–1249. PMID: 26398072.
Article42. Louie S, Zeki AA, Schivo M, Chan AL, Yoneda KY, Avdalovic M, et al. The asthma-chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol. 2013; 6:197–219. PMID: 23473596.
Article43. Lin TY, Poon AH, Hamid Q. Asthma phenotypes and endotypes. Curr Opin Pulm Med. 2013; 19:18–23. PMID: 23114560.
Article44. Bateman ED, Reddel HK, van Zyl-Smit RN, Agusti A. The asthma-COPD overlap syndrome: towards a revised taxonomy of chronic airways diseases? Lancet Respir Med. 2015; 3:719–728. PMID: 26255108.
Article45. Rhee CK. Phenotype of asthma-chronic obstructive pulmonary disease overlap syndrome. Korean J Intern Med. 2015; 30:443–449. PMID: 26161009.
Article46. Miravitlles M, Alcázar B, Alvarez FJ, Bazús T, Calle M, Casanova C, et al. What pulmonologists think about the asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2015; 10:1321–1330.47. Ding B, Enstone A. Asthma and chronic obstructive pulmonary disease overlap syndrome (ACOS): structured literature review and physician insights. Expert Rev Respir Med. 2016; 10:363–371. PMID: 26789845.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Systemic Inflammation in Older Adults With Asthma-COPD Overlap Syndrome
- Overlap Between Asthma and COPD: Where the Two Diseases Converge
- Status of Studies Investigating Asthma–Chronic Obstructive Pulmonary Disease Overlap in Korea: A Review
- Treatment of Severe Asthma
- Asthma-COPD Overlap Syndrome: What We Know and What We Don't