J Korean Soc Radiol.
2018 Feb;78(2):95-102. 10.3348/jksr.2018.78.2.95.
Correlation of Semi-Quantitative Breast-Specific Gamma Imaging Findings with Dynamic Contrast-Enhanced MRI Parameters Assessed by a Computer-Aided Evaluation Program for Breast Cancer
- Affiliations
-
- 1Department of Radiology, Hanyang University College of Medicine, Seoul, Korea. huilingkoo@gmail.com
- 2Department of Radiology, Hanyang University College of Medicine, Hanyang University Guri Hospital, Guri, Korea.
- 3Department of Nuclear Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 4Department of General Surgery, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2408258
- DOI: http://doi.org/10.3348/jksr.2018.78.2.95
Abstract
- PURPOSE
To investigate whether a correlation exists between the semi-quantitative breast-specific gamma imaging (BSGI) findings and dynamic contrast-enhanced (DCE) MRI parameters assessed by a computer-aided evaluation program.
MATERIALS AND METHODS
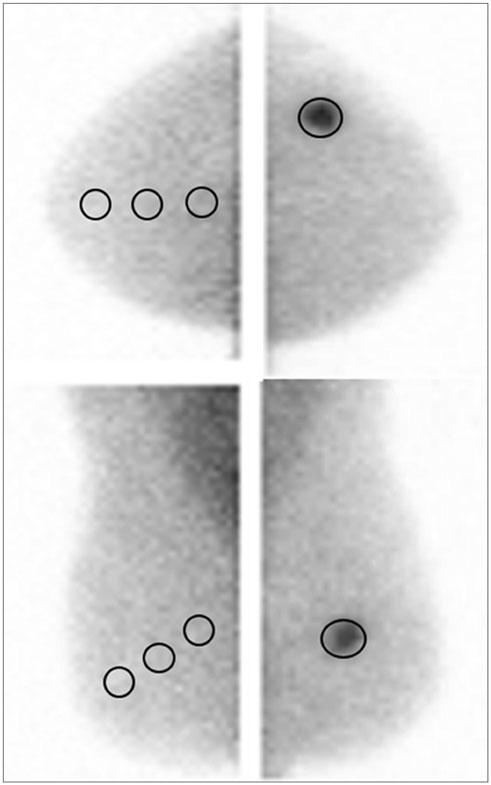
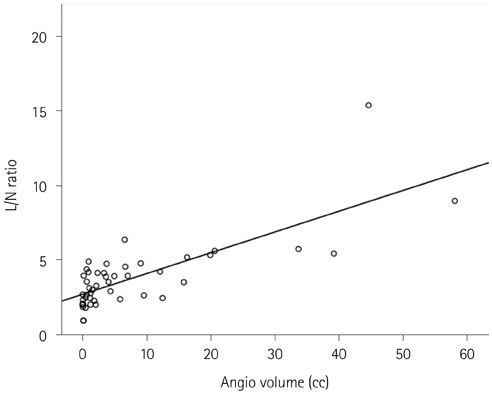
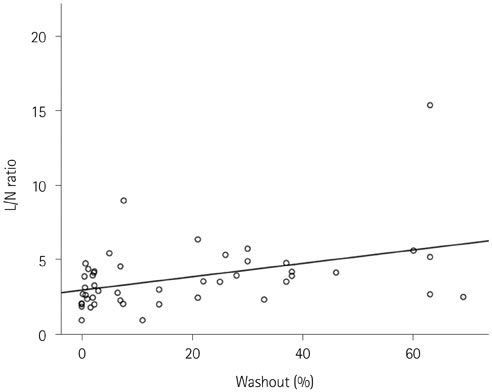
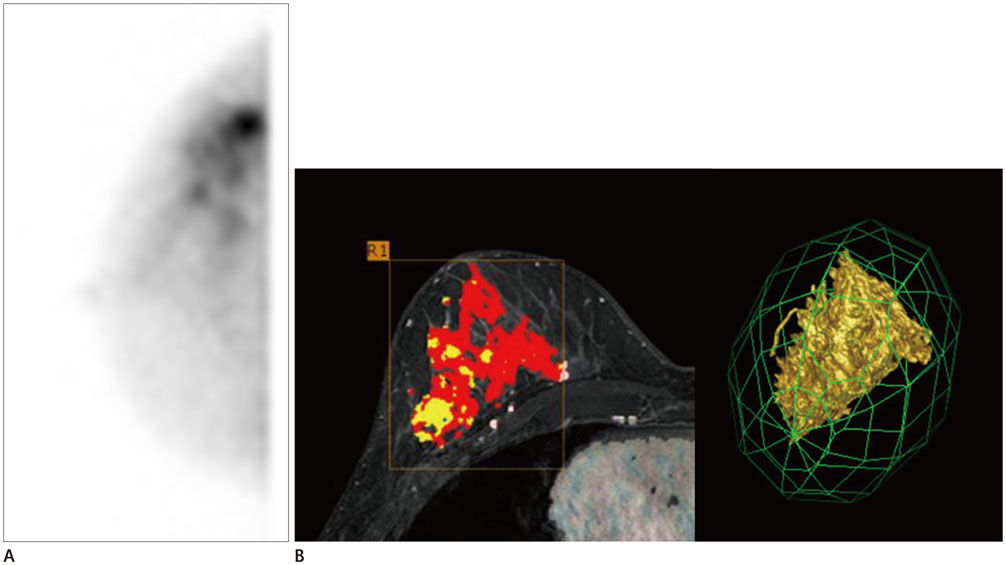
Semi-quantitative index of the lesion to non-lesion (L/N) ratio in BSGI and DCE-MRI parameters was assessed by a computer-aided evaluation program, where 47 cases of invasive breast cancer were obtained. Correlations between the L/N ratio and DCE-MRI parameters were assessed by a computer-aided evaluation program. Tumor diameter (cm), angio-volume (cc), degree of initial peak enhancement (%), persistent enhancement proportion (%), and washout enhancement proportion (%) were analysed. The relationships between the L/N ratio and DCE-MRI parameters were evaluated by a univariate and multivariate regression analysis.
RESULTS
The mean L/N ratio of the 47 tumors was 3.63 ± 2.19 (range: 1-13.1). The L/N ratio was higher in tumors with larger diameters (p < 0.001), increased angio-volume (p < 0.001), higher degree of initial peak enhancement (p = 0.005) and increased washout enhancement proportion (p = 0.004). In the multivariate regression analysis, angio-volume (cc) and washout enhancement proportion (%) were associated with L/N ratio (p = 0.007 and p = 0.024, respectively).
CONCLUSION
There was a correlation between the semi-quantitative L/N ratio in BSGI and DCE-MRI parameters assessed by a computer-aided evaluation program for breast cancer.
MeSH Terms
Figure
Reference
-
1. Brem RF, Rechtman LR. Nuclear medicine imaging of the breast: a novel, physiologic approach to breast cancer detection and diagnosis. Radiol Clin North Am. 2010; 48:1055–1074.
Article2. Yoon HJ, Kim Y, Chang KT, Kim BS. Prognostic value of semi-quantitative tumor uptake on Tc-99m sestamibi breast-specific gamma imaging in invasive ductal breast cancer. Ann Nucl Med. 2015; 29:553–560.
Article3. Yu X, Hu G, Zhang Z, Qiu F, Shao X, Wang X, et al. Retrospective and comparative analysis of (99m)Tc-Sestamibi breast specific gamma imaging versus mammography, ultrasound, and magnetic resonance imaging for the detection of breast cancer in Chinese women. BMC Cancer. 2016; 16:450.
Article4. Specht JM, Mankoff DA. Advances in molecular imaging for breast cancer detection and characterization. Breast Cancer Res. 2012; 14:206.
Article5. Sun Y, Wei W, Yang HW, Liu JL. Clinical usefulness of breast-specific gamma imaging as an adjunct modality to mammography for diagnosis of breast cancer: a systemic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2013; 40:450–463.
Article6. Tan H, Jiang L, Gu Y, Xiu Y, Han L, Wu P, et al. Visual and semi-quantitative analyses of dual-phase breast-specific gamma imaging with Tc-99m-sestamibi in detecting primary breast cancer. Ann Nucl Med. 2014; 28:17–24.
Article7. Kuhl CK, Mielcareck P, Klaschik S, Leutner C, Wardelmann E, Gieseke J, et al. Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology. 1999; 211:101–110.
Article8. Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology. 2001; 220:13–30.
Article9. Jena A, Taneja S, Singh A, Negi P, Mehta SB, Sarin R. Role of pharmacokinetic parameters derived with high temporal resolution DCE MRI using simultaneous PET/MRI system in breast cancer: a feasibility study. Eur J Radiol. 2017; 86:261–266.
Article10. Aghaei F, Tan M, Hollingsworth AB, Qian W, Liu H, Zheng B. Computer-aided breast MR image feature analysis for prediction of tumor response to chemotherapy. Med Phys. 2015; 42:6520–6528.
Article11. Dorrius MD, Jansen-van der Weide MC, van Ooijen PM, Pijnappel RM, Oudkerk M. Computer-aided detection in breast MRI: a systematic review and meta-analysis. Eur Radiol. 2011; 21:1600–1608.
Article12. Kim BS. Usefulness of breast-specific gamma imaging as an adjunct modality in breast cancer patients with dense breast: a comparative study with MRI. Ann Nucl Med. 2012; 26:131–137.
Article13. Johnson N, Sorenson L, Bennetts L, Winter K, Bryn S, Johnson W, et al. Breast-specific gamma imaging is a cost effective and efficacious imaging modality when compared with MRI. Am J Surg. 2014; 207:698–701. discussion 701.
Article14. Brem RF, Floerke AC, Rapelyea JA, Teal C, Kelly T, Mathur V. Breast-specific gamma imaging as an adjunct imaging modality for the diagnosis of breast cancer. Radiology. 2008; 247:651–657.
Article15. Tan H, Zhang H, Yang W, Fu Y, Gu Y, Du M, et al. Breast-specific gamma imaging with Tc-99m-sestamibi in the diagnosis of breast cancer and its semiquantitative index correlation with tumor biologic markers, subtypes, and clinicopathologic characteristics. Nucl Med Commun. 2016; 37:792–799.
Article16. Tadwalkar RV, Rapelyea JA, Torrente J, Rechtman LR, Teal CB, McSwain AP, et al. Breast-specific gamma imaging as an adjunct modality for the diagnosis of invasive breast cancer with correlation to tumour size and grade. Br J Radiol. 2012; 85:e212–e216.
Article17. Baltzer PA, Vag T, Dietzel M, Beger S, Freiberg C, Gajda M, et al. Computer-aided interpretation of dynamic magnetic resonance imaging reflects histopathology of invasive breast cancer. Eur Radiol. 2010; 20:1563–1571.
Article18. Narisada H, Aoki T, Sasaguri T, Hashimoto H, Konishi T, Morita M, et al. Correlation between numeric gadolinium-enhanced dynamic MRI ratios and prognostic factors and histologic type of breast carcinoma. AJR Am J Roentgenol. 2006; 187:297–306.
Article19. Bekiş R, Degirmenci B, Aydin A, Ozdogan O, Canda T, Durak H. Correlation between 99mTc-MIBI uptake and angiogenesis in MIBI-positive breast lesions. Nucl Med Biol. 2005; 32:465–472.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Findings of Breast Diseases
- Treatment Response Evaluation of Breast Cancer after Neoadjuvant Chemotherapy and Usefulness of the Imaging Parameters of MRI and PET/CT
- Use of Abbreviated Magnetic Resonance Imaging in Breast Cancer Screening
- Response Evaluation to Neoadjuvant Chemotherapy in Breast Cancer Patients: Sequential Dynamic Contrast-Enhanced MRI Using Computer-Aided Detection
- Breast-Specific Gamma Imaging in Breast Cancer Screening