J Korean Soc Radiol.
2018 Apr;78(4):279-283. 10.3348/jksr.2018.78.4.279.
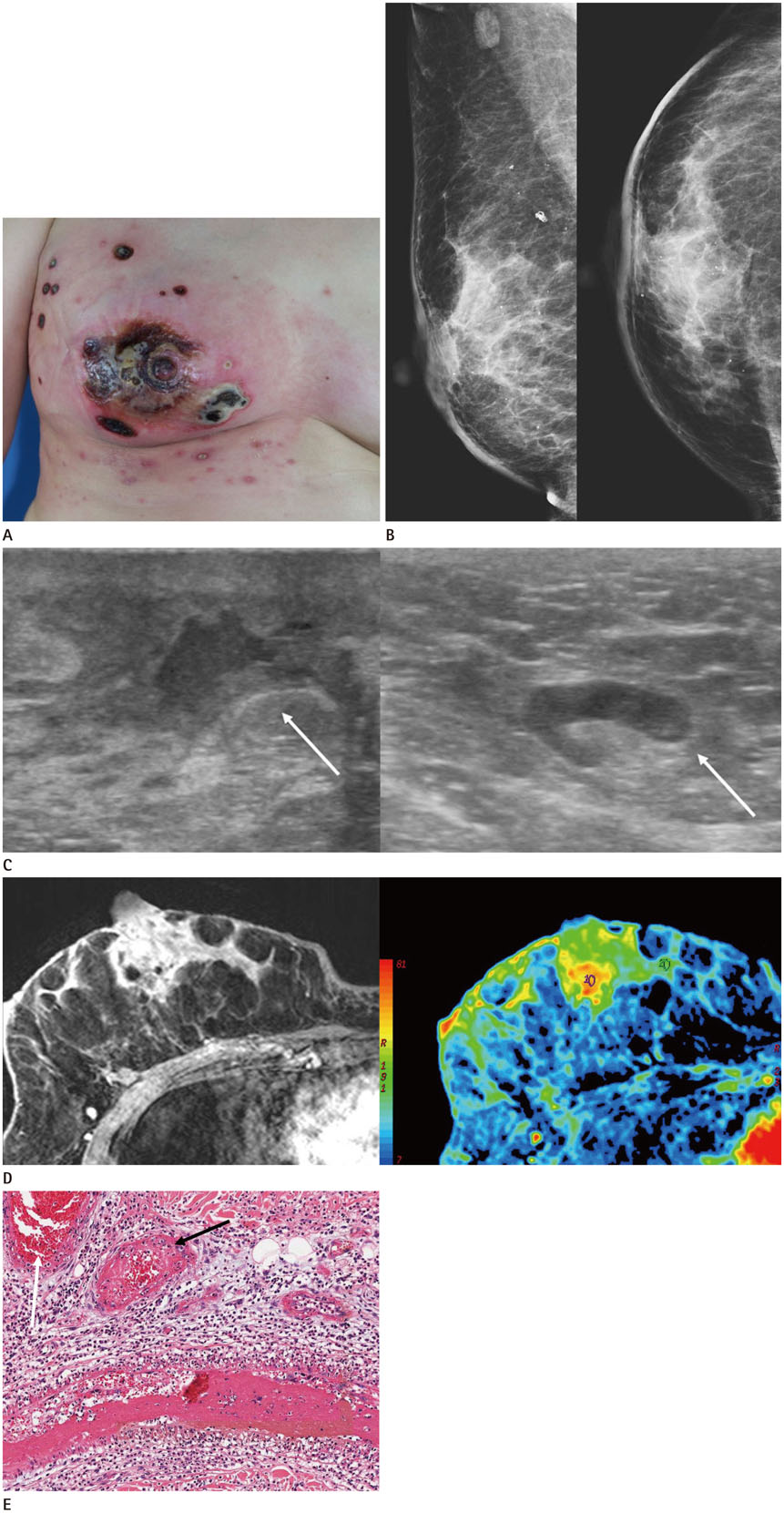
Leukocytoclastic Vasculitis of the Breast: A Case Report
- Affiliations
-
- 1Department of Radiology, Ajou University School of Medicine, Suwon, Korea. h219435@gmail.com
- 2Department of Pathology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2407933
- DOI: http://doi.org/10.3348/jksr.2018.78.4.279
Abstract
- Leukocytoclastic vasculitis is a rare disease characterized by neutrophil and immune-complex deposition in the small vessel walls. We report a 47-year-old female patient with leukocytoclastic vasculitis of the breast, presenting as breast edema on mammography, irregular hypoechoic lesion with central necrosis on ultrasonography and regionally distributed heterogeneous non-mass enhancement on magnetic resonance imaging.
MeSH Terms
Figure
Reference
-
1. Fiorentino DF. Cutaneous vasculitis. J Am Acad Dermatol. 2003; 48:311–340.
Article2. Dubost JJ, Souteyrand P, Sauvezie B. Drug-induced vasculitides. Baillieres Clin Rheumatol. 1991; 5:119–138.
Article3. Hernández-Rodríguez J, Hoffman GS. Updating single-organ vasculitis. Curr Opin Rheumatol. 2012; 24:38–45.
Article4. Kadotani Y, Enoki Y, Itoi N, Kojima F, Kato G, Lee CJ. Giant cell arteritis of the breast: a case report with a review of literatures. Breast Cancer. 2010; 17:225–232.
Article5. Khalil HH, Marsden J, Akbar N, Gordon P, Roberts J, Schulte KM. Polyarteritis nodosa of the breast: presentation and management. Int J Surg. 2009; 7:446–450.
Article6. Szabo-Moskal J. Wegener's granulomatosis of the breast: a case report. Pol J Radiol. 2014; 79:117–119.
Article7. Lee JY, Joo M. Isolated breast vasculitis manifested as breast edema with suggestive sonographic findings: a case report with imaging findings. J Med Ultrason. 2017; 44:191–195.
Article8. Ozturk M, Mavili E, Kahriman G, Akcan AC, Ozturk F. Granulomatous mastitis: radiological findings. Acta Radiol. 2007; 48:150–155.
Article9. Chu AN, Seiler SJ, Hayes JC, Wooldridge R, Porembka JH. Magnetic resonance imaging characteristics of granulomatous mastitis. Clin Imaging. 2017; 43:199–201.
Article10. Sunderkötter C, Bonsmann G, Sindrilaru A, Luger T. Management of leukocytoclastic vasculitis. J Dermatolog Treat. 2005; 16:193–206.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leukocytoclastic Vasculitis Following COVID-19 Vaccination
- Warfarin-induced Leukocytoclastic Vasculitis
- Sibutramine (Reductil(R))-Induced Cutaneous Leukocytoclastic Vasculitis: A Case Report
- A Case of Annular Leukocytoclastic Vasculitis
- A Case of Leukocytoclastic Vasculitis Associated with Pulmonary Tuberculosis