J Korean Soc Radiol.
2018 Apr;78(4):225-234. 10.3348/jksr.2018.78.4.225.
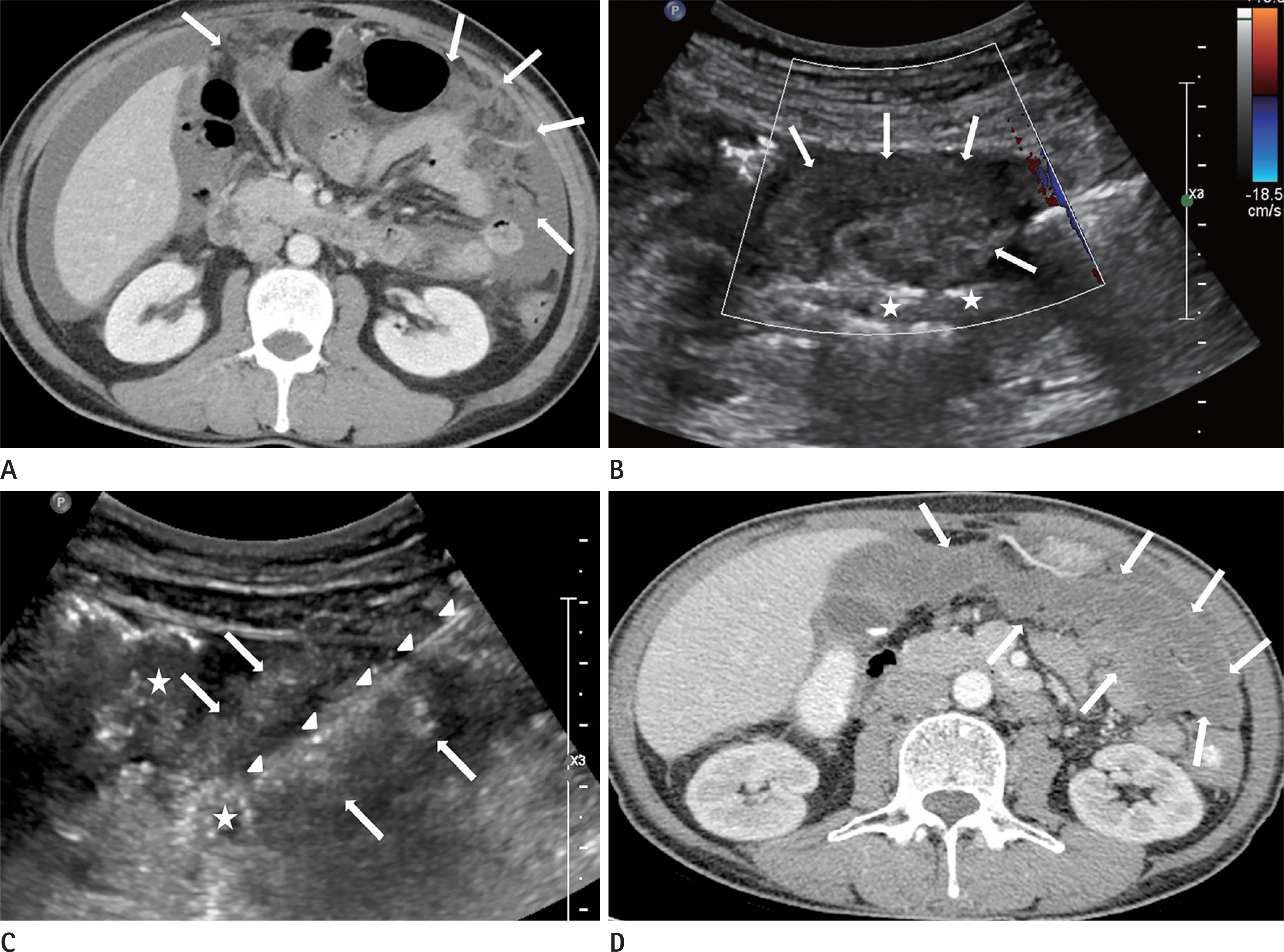
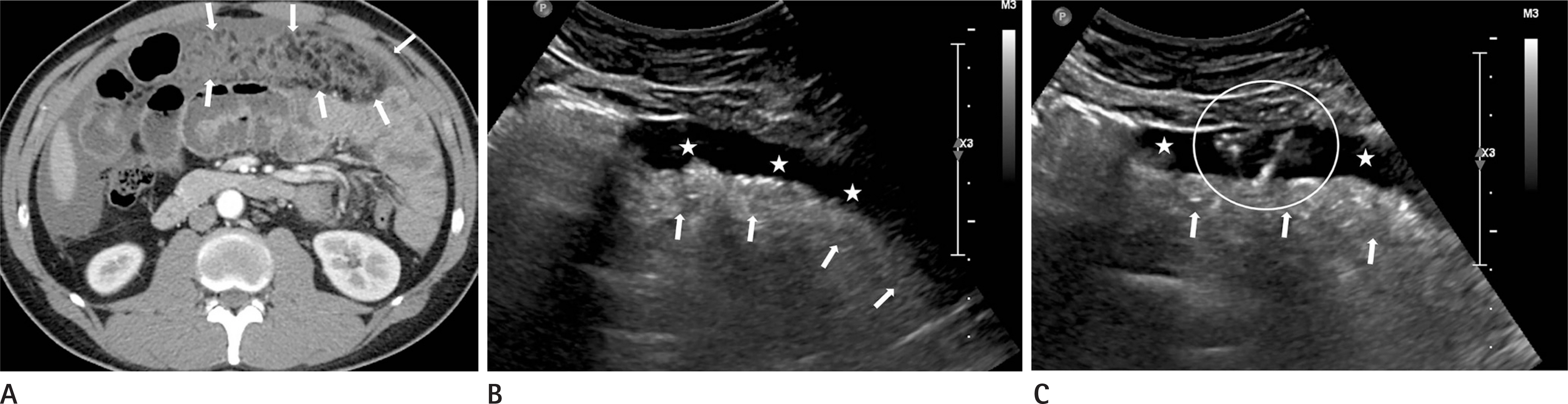
The Diagnostic Usefulness of Ultrasound-Guided Peritoneal Biopsy for the Solitary Peritoneal Thickening of an Unknown Cause Visualized as Only Infiltrated Fat Tissue on a CT Scan
- Affiliations
-
- 1Department of Radiology, Kyungpook National University Hospital, Daegu, Korea. hkryeom@knu.ac.kr
- 2Department of Radiology, Kyungpook National University Chilgok Hospital, Daegu, Korea.
- 3Public Health Medical Service, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2407927
- DOI: http://doi.org/10.3348/jksr.2018.78.4.225
Abstract
- PURPOSE
To assess the usefulness of an ultrasound (US)-guided peritoneal biopsy for the solitary peritoneal thickening visualized as only infiltrated fat on a computed tomography (CT) scan.
MATERIALS AND METHODS
This retrospective study included 36 patients (16 males, 20 females; mean age, 51.7 years) who underwent a US-guided biopsy for the solitary peritoneal thickening of unknown cause visualized as only infiltrated fat without an apparent mass formation on a CT scan. The rate of the specific histopathological diagnosis and accuracy for the diagnosis of malignant disease was assessed.
RESULTS
The procedure was technically successful with the acquisition of an adequate amount of the specimen for microscopic examination from all patients. A specific histopathological diagnosis was made in 31/36 patients (86.1%): peritoneal carcinomatosis in 15/31 (48.4%), tuberculous peritonitis in 15/31 (48.4%) and panniculitis in 1/31 (3.2%). A non-specific histopathological diagnosis was made in 5/36 (13.9%): chronic inflammation in 4/5 (80%) and mesothelial hyperplasia in 1/5 (20%). The procedure showed sensitivity of 83.3%, with a specificity of 100%, a positive predictive value of 100%, a negative predictive value of 85.7%, and an accuracy rate of 86.1% for the diagnosis of malignant diseases.
CONCLUSION
The US-guided peritoneal biopsy is a fairly accurate diagnostic procedure for the peritoneal thickening visualized as only infiltrated fat on a CT scan, and it can be used before performing laparoscopic or an open biopsy.
MeSH Terms
Figure
Cited by 1 articles
-
Reappraisal of the Role of Ascitic Fluid Adenosine Deaminase for the Diagnosis of Peritoneal Tuberculosis in Cirrhosis
Amol Sonyabapu Dahale, Amarender Singh Puri, Sanjeev Sachdeva, Anil K Agarwal, Ajay Kumar, Ashok Dalal, Pritul D Saxena
Korean J Gastroenterol. 2021;78(3):168-176. doi: 10.4166/kjg.2021.068.
Reference
-
References
1. Levy AD, Arnáiz J, Shaw JC, Sobin LH. From the archives of the AFIP: primary peritoneal tumors: imaging features with pathologic correlation. Radiographics. 2008; 28:583–607.2. Levy AD, Shaw JC, Sobin LH. Secondary tumors and tumorlike lesions of the peritoneal cavity: imaging features with pathologic correlation. Radiographics. 2009; 29:347–373.
Article3. Kang SJ, Kim JW, Baek JH, Kim SH, Kim BG, Lee KL, et al. Role of ascites adenosine deaminase in differentiating between tuberculous peritonitis and peritoneal carcinomatosis. World J Gastroenterol. 2012; 18:2837–2843.
Article4. Xiao WB, Liu YL. Elevation of serum and ascites cancer antigen 125 levels in patients with liver cirrhosis. J Gastroenterol Hepatol. 2003; 18:1315–1316.
Article5. Simsek H, Savas MC, Kadayifci A, Tatar G. Elevated serum CA 125 concentration in patients with tuberculous peritonitis: a case-control study. Am J Gastroenterol. 1997; 92:1174–1176.6. Hiller N, Lioubashevsky N. Tuberculous peritonitis: a diagnostic challenge. Abdom Imaging. 2001; 26:319–322.
Article7. Filippone A, Cianci R, Delli Pizzi A, Esposito G, Pulsone P, Tavoletta A, et al. CT findings in acute peritonitis: a pattern-based approach. Diagn Interv Radiol. 2015; 21:435–440.
Article8. Charoensak A, Nantavithya P, Apisarnthanarak P. Abdominal CT findings to distinguish between tuberculous peritonitis and peritoneal carcinomatosis. J Med Assoc Thai. 2012; 95:1449–1456.9. Vázquez Muñoz E, Gómez-Cerezo J, Atienza Saura M, Vázquez Rodriguez JJ. Computed tomography findings of peritoneal tuberculosis: systematic review of seven patients diagnosed in 6 years (1996–2001). Clin Imaging. 2004; 28:340–343.10. Chen R, Chen Y, Liu L, Zhou X, Liu J, Huang G. The role of 18F-FDG PET/CT in the evaluation of peritoneal thickening of undetermined origin. Medicine (Baltimore). 2016; 95:e3023.
Article11. Wang SB, Ji YH, Wu HB, Wang QS, Zhou WL, Lv L, et al. PET/CT for differentiating between tuberculous peritonitis and peritoneal carcinomatosis: the parietal peritoneum. Medicine (Baltimore). 2017; 96:e5867.12. Suzuki A, Kawano T, Takahashi N, Lee J, Nakagami Y, Miyagi E, et al. Value of 18F-FDG PET in the detection of peritoneal carcinomatosis. Eur J Nucl Med Mol Imaging. 2004; 31:1413–1420.
Article13. Târcoveanu E, Dimofte G, Bradea C, Lupas¸cu C, Moldovanu R, Vasilescu A. Peritoneal tuberculosis in laparoscopic era. Acta Chir Belg. 2009; 109:65–70.
Article14. Bedioui H, Ksantini R, Nouira K, Mekni A, Daghfous A, Chebbi F, et al. Role of laparoscopic surgery in the etiologic diagnosis of exsudative ascites: a prospective study of 90 cases. Gastroenterol Clin Biol. 2007; 31:1146–1149.
Article15. Abdelaal A, Alfkey R, Abdelaziem S, Abunada M, Alfaky A, Ibrahim WH, et al. Role of laparoscopic peritoneal biopsy in the diagnosis of peritoneal tuberculosis. A seven-year experience. Chirurgia (Bucur). 2014; 109:330–334.16. Hong KD, Lee SI, Moon HY. Comparison between laparoscopy and noninvasive tests for the diagnosis of tuberculous peritonitis. World J Surg. 2011; 35:2369–2375.
Article17. Perugini RA, Callery MP. Complications of laparoscopic surgery. In Holzheimer RG, Mannick JA, eds. Surgical treatment: evidencebased and problem-oriented. Munich: Zuckschw-erdt. 2001.18. Beleña JM, Nuñez M. Postoperative complications of laparoscopic surgery. Int J Clin Anesthesiol. 2014; 2:1034.19. Souza FF, Mortelé KJ, Cibas ES, Erturk SM, Silverman SG. Predictive value of percutaneous imaging-guided biopsy of peritoneal and omental masses: results in 111 patients. AJR Am J Roentgenol. 2009; 192:131–136.
Article20. Wang J, Gao L, Tang S, Li T, Lei Y, Xie H, et al. A retrospective analysis on the diagnostic value of ultrasound-guided percutaneous biopsy for peritoneal lesions. World J Surg Oncol. 2013; 11:251.
Article21. Que Y, Wang X, Liu Y, Li P, Ou G, Zhao W. Ultrasound-guided biopsy of greater omentum: an effective method to trace the origin of unclear ascites. Eur J Radiol. 2009; 70:331–335.
Article22. Mahmood K, Saeedi MI, Mohammad R, Ziauddin , Kamal M. Percutaneous needle peritoneal biopsy in the diagnosis of exudative ascites. J Ayub Med Coll Abbottabad. 2008; 20:94–96.23. Khati NJ, Gorodenker J, Hill MC. Ultrasound-guided biopsies of the abdomen. Ultrasound Q. 2011; 27:255–268.
Article24. Kim YH, Ryeom HK, Chung TG, Park HY, Kim YJ, Kang DS. Ultrasound-guided biopsy of the thickened peritoneal reflections: efficacy and diagnostic role in the differential diagnosis of peritoneal tuberculosis and peritoneal carcinomatosis. J Korean Radiol Soc. 2000; 43:215–221.
Article25. Mehta JB, Dutt A, Harvill L, Mathews KM. Epidemiology of extrapulmonary tuberculosis: a comparative analysis with pre-AIDS era. Chest. 1991; 99:1134–1138.26. Cegielski JP, Chin DP, Espinal MA, Frieden TR, Rodriquez Cruz R, Talbot EA, et al. The global tuberculosis situation: progress and problems in the 20th century, prospects for the 21st century. Infect Dis Clin North Am. 2002; 16:1–58.
Article27. Gore RM, Miller FH, Yaghmai V. Acquired immunodeficiency syndrome (AIDS) of the abdominal organs: imaging features. Semin Ultrasound CT MR. 1998; 19:175–189.
Article28. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–867.
Article29. Ji HL, Nie HG. Electrolyte and fluid transport in mesothelial cells. J Epithel Biol Pharmacol. 2008; 1:1–7.
Article30. Smith EH. Complications of percutaneous abdominal fine-needle biopsy review. Radiology. 1991; 178:253–258.
Article31. Satava RM Jr, van Heerden JA, Sheedy PF 2nd, Summerskill WH. Omental arteriovenous fistula following liver biopsy. Gastroenterology. 1975; 69:492–495.
Article32. Gottlieb RH, Tan R, Widjaja J, Fultz PJ, Robinette WB, Rubens DJ. Extravisceral masses in the peritoneal cavity: sonographically guided biopsies in 52 patients. AJR Am J Roentgenol. 1998; 171:697–701.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided Biopsy of the Thickened Peritoneal Reflections: Efficacy and Diagnostic Role in the Differential Diagnosis of Peritoneal Tuberculosis and Peritoneal Carcinomatosis
- Idiopathic Isolated Omental Panniculitis Confirmed by Percutaneous CT-Guided Biopsy
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Endoscopic ultrasound-guided tissue acquisition: Needle types, technical issues, and sample handling
- Unusual Peritoneal Metastasis of Late Recurrent Uterine Cervical Cancer: A Case Report and Literature Review