Hanyang Med Rev.
2018 Mar;38(1):27-37. 10.7599/hmr.2018.38.1.27.
Perioperative Blood Management: Pros and Cons of ANH and Cell Salvage
- Affiliations
-
- 1Department of Surgery, Hanyang University College of Medicine, Seoul, Korea.
- 2Department of Anesthesiology and Pain Medicine, Sejong General Hospital, Bucheon, Korea. jonghyeonlee@gmail.com
- KMID: 2407799
- DOI: http://doi.org/10.7599/hmr.2018.38.1.27
Abstract
- Increasingly, autologous blood transfusion has been arousing concern owing to awareness of adverse effects of allogenic blood transfusion, blood shortage and patients, having religious or personal issues. With the development of medicine, Cell Salvage and Acute normovolemic hemodilution (ANH) has been proposed as an alternative to allogenic blood transfusion. This review looked at the use of ANH and cell salvage and evaluated the benefits and usefulness based on the strengths and indications. Although not consistent with all cases of ANH, there were benefits in the amount of hemorrhage and transfusion, and no supplementary plasma or platelet transfusion was needed after surgery when employing ANH. But, it showed a cutoff value only for massive bleeding surgery (at least 500 mL). In the case of cell salvage, the amount of blood transfusion was reduced in most cases and platelet or plasma transfusion was not required in most cases. When the Leukoreduction filter (LDF) was utilized, it showed the effect of removing bacterial infection or tumor cells. Nonetheless, the effectiveness and benefits for patients in certain condition of cell salvage and ANH is ambiguous with discrepancies among studies or patients. Therefore, the aim of this study is to provide clinical knowledge relative to the procedure, measure the efficacy and usefulness of peri-operative blood management mentioned above and discuss the forthcoming prospects and challenges.
MeSH Terms
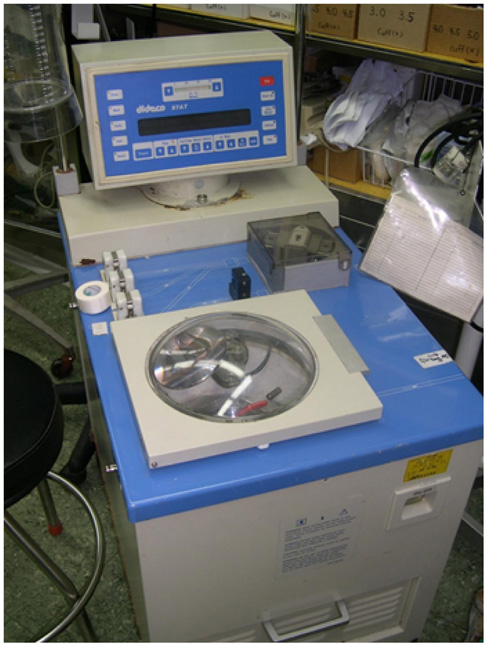
Figure
Cited by 1 articles
-
Cutting-Edge Technologies for Patient Blood Management
Dongho Choi
Hanyang Med Rev. 2018;38(1):1-2. doi: 10.7599/hmr.2018.38.1.1.
Reference
-
1. Waters JH, Potter PS. Cell Salvage in the Jehovah's witness patient. Anesth Analg. 2000; 90:229–230.
Article2. Vries Hd. Use of the cell saver in blood management. EACTA. 2012; 33–35.3. Eeles A, Baikady RR. Peri-operative blood management. Indian J Anaesth. 2017; 61:456–462.
Article4. Themistoklis T, Theodosia V, Konstantinos K, Georgios DI. Perioperative blood management strategies for patients undergoing total knee replacement: where do we stand now? World J Orthop. 2017; 8:441–454.
Article5. Sikorski RA, Rizkalla NA, Yang WW, Frank SM. Autologous blood salvage in the era of patient blood management. Vox Sang. 2017; 112:499–510.
Article6. De Araújo LMT, Garcia LV. Acute normovolemic hemodilution: a practical approach. Open J Anesthesiol. 2013; 3:38–43.
Article7. Segal JB, Blasco-Colmenares E, Norris EJ, Guallar E. Preoperative acute normovolemic hemodilution: a meta-analysis. Transfusion. 2004; 44:632–644.
Article8. Zhou X, Zhang C, Wang Y, Yu L, Yan M. Preoperative acute normovolemic hemodilution for minimizing allogeneic blood transfusion: a meta-analysis. Anesth Analg. 2015; 121:1443–1455.
Article9. Virmani S, Tempe DK, Pandey BC, Cheema AS, Datt V, Garg M, et al. Acute normovolemic hemodilution is not beneficial in patients undergoing primary elective valve surgery. Ann Card Anaesth. 2010; 13:34–38.
Article10. Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983; 58:277–280.11. Zhou J. A review of the application of autologous blood transfusion. Braz J Med Biol Res. 2016; 49:e5493.
Article12. Drummond JC, Petrovitch CT, Lane TA. Hemostasis and transfusion medicine. 6 ed. 2009.13. Bryson GL, Laupacis A, Wells GA. does acute normovolemic hemodilution reduce perioperative allogenic transfusion? A metaanalysis. Anesth Analg. 1998; 86:9–15.
Article14. Barile L, Fominskiy E, Di Tomasso N, Alpizar Castro LE, Landoni G, De Luca M, et al. Acute normovolemic hemodilution reduces allogeneic red blood cell transfusion in cardiac surgery: a systematic review and meta-analysis of randomized trials. Anesth Analg. 2017; 124:743–752.
Article15. Sebastian R, Ratliff T, Winch PD, Tumin D, Gomez D, Tobias J, et al. Revisiting acute normovolemic hemodilution and blood transfusion during pediatric cardiac surgery: a prospective observational study. Paediatr Anaesth. 2017; 27:85–90.
Article16. Goldberg J, Paugh TA, Dickinson TA, Fuller J, Paone G, Theurer PF, et al. Greater volume of acute normovolemic hemodilution may aid in reducing blood transfusions after cardiac surgery. Ann Thorac Surg. 2015; 100:1581–1587. discussion 1587.
Article17. Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg. 2013; 79:719–724.
Article18. Murray D. Acute normovolemic hemodilution. Eur Spine J. 2004; 13:Suppl 1. S72–S75.
Article19. Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in anaesthesia. Br J Anaesth. 2010; 105:401–416.
Article20. Carless PA, Henry DA, Moxey AJ, O'Connell D, Brown T, Fergusson DA. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2010; CD001888.
Article21. Hovav T, Yedgar S, Manny N, Barshtein G. Alteration of red cell aggregability and shape during blood storage. Transfusion. 1999; 39:277–281.
Article22. Esper SA, Waters JH. Intra-operative cell salvage: a fresh look at the indications and contraindications. Blood Transfus. 2011; 9:139–147.23. Al-Mandhari S, Maddali MM, Al-Bahrani MJ. Cell salvage during coronary artery bypass surgery and allogenic blood exposure. Asian Cardiovasc Thorac Ann. 2015; 23:913–916.
Article24. Goel P, Pannu H, Mohan D, Arora R. Efficacy of cell saver in reducing homologous blood transfusions during OPCAB surgery: a prospective randomized trial. Transfus Med. 2007; 17:285–289.
Article25. Wang G, Bainbridge D, Martin J, Cheng D. The efficacy of an intraoperative cell saver during cardiac surgery: a meta-analysis of randomized trials. Anesth Analg. 2009; 109:320–330.
Article26. Almeida RM, Leitao L. The use of cell saver system in cardiac surgery with cardiopulmonary bypass. Rev Bras Cir Cardiovasc. 2013; 28:76–82.
Article27. Nusrath MA, Edge CJ, Ahmed-Nusrath A. Intraoperative red cell salvage in head and neck surgery. Br J Oral Maxillofac Surg. 2012; 50:272–274.
Article28. Kelly PD, Parker SL, Mendenhall SK, Bible JE, Sivasubramaniam P, Shau DN, et al. Cost-effectiveness of cell saver in short-segment lumbar laminectomy and fusion (</=3 levels). Spine (Phila Pa 1976). 2015; 40:E978–E985.29. Akgul T, Dikici F, Ekinci M, Buget M, Polat G, Sar C. The efficacy of cell saver method in the surgical treatment of adolescent idiopathic scoliosis. Acta Orthop Traumatol Turc. 2014; 48:303–306.
Article30. Konstantinou EA, Brady JM, Soultati A, Mitsos A, Mamoura K, Mariolis TS, et al. Intraoperative use of cell saver on patients undergoing open abdominal aortic aneurysm surgical repair: a Greek hospital experience. J Perianesth Nurs. 2011; 26:225–230.
Article31. Gilbert JB, Malkowicz SB, Wein AJ. Cell saver and radical retropubic prostatectomy: analysis of cost-effectiveness. Urology. 1995; 46:542–544.
Article32. Kumar N, Chen Y, Zaw AS, Nayak D, Ahmed Q, Soong R, et al. Use of intraoperative cell-salvage for autologous blood transfusions in metastatic spine tumour surgery: a systematic review. Lancet Oncol. 2014; 15:e33–e41.
Article33. ÉLias D, Billard V, Lapierre V. Use of the cell saver in oncologic surgery. Transfus Altern Transfus Med. 2001; 3:25–28.
Article34. Prieto MA, Guash S, Mendez JC, Munoz C, Planas A, Reyes G. Does use of cell saver decrease the inflammatory response in cardiac surgery? Asian Cardiovasc Thorac Ann. 2013; 21:37–42.
Article35. Davies L, Brown T, Haynes S, Payne K, Elliott R, McCollum C. cost-effectiveness fo cell salvage and alternative methods of minimising perioperative allogenic blood transfusion_a systematic review and economic model.pdf. Health Technol Assess. 2006; 10.
Article36. Solomon L, von Rahden RP, Allorto NL. Intra-operative cell salvage in South Africa: feasible, beneficial and economical. S Afr Med J. 2013; 103:754–757.
Article37. Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. Jama. 2015; 313:471–482.38. Crystal GJ, Doll D, Boggs SD, Stueber F. Reduced blood viscosity plays minor role in regional blood flow increases during acute normovolemic hemodilution. Anesth Analg. 2017; 124:1739–1740.
Article39. Guo JR, Jin XJ, Yu J, Xu F, Zhang YW, Shen HC, et al. Acute normovolemic hemodilution effects on perioperative coagulation in elderly patients undergoing hepatic carcinectomy. Asian Pac J Cancer Prev. 2013; 14:4529–4532.
Article40. Perez-Ferrer A, Gredilla-Díaz E, de Vicente-Sánchez J, Navarro-Suay R, Gilsanz-Rodríguez F. Vancomycin added to the wash solution of the cell-saver. Effect on bacterial contamination. Rev Esp Anestesiol Reanim. 2017; 64:185–191.
Article41. Meybohm P, Choorapoikayil S, Wessels A, Herrmann E, Zacharowski K, Spahn DR. Washed cell salvage in surgical patients: a review and meta-analysis of prospective randomized trials under PRISMA. Medicine (Baltimore). 2016; 95:e4490.42. Catling S, Williams S, Freites O, Rees M, Davies C, Hopkins L. Use of a leucocyte filter to remove tumour cells from intra-operative cell salvage blood. Anaesthesia. 2008; 63:1332–1338.
Article43. Sullivan I, Faulds J, Ralph C. Contamination of salvaged maternal blood by amniotic fluid and fetal red cells during elective Caesarean section. Br J Anaesth. 2008; 101:225–229.
Article44. Araujo RL, Pantanali CA, Haddad L, Rocha Filho JA, D'Albuquerque LA, Andraus W. Does autologous blood transfusion during liver transplantation for hepatocellular carcinoma increase risk of recurrence. World J Gastrointest Surg. 2016; 8:161–168.
Article45. Al-Riyami AZ, Al-Khabori M, Baskaran B, Siddiqi M, Al-Sabti H. Intra-operative cell salvage in cardiac surgery may increase platelet transfusion requirements: a cohort study. Vox Sang. 2015; 109:280–286.
Article46. Qureshi R, Puvanesarajah V, Jain A, Hassanzadeh H. Perioperative Management of Blood Loss in Spine Surgery. Clin Spine Surg. 2017.
Article47. van den Goor JM, Nieuwland R, van Oeveren W, Rutten PM, Tijssen JG, Hau CM, et al. Cell Saver device efficiently removes cell-derived microparticles during cardiac surgery. J Thorac Cardiovasc Surg. 2007; 134:798–799.
Article48. Gum JL, Carreon LY, Kelly MP, Hostin R, Robinson C, Burton DC, et al. Cell saver for adult spinal deformity surgery reduces cost. Spine Deform. 2017; 5:272–276.
Article49. Miao YL, Ma HS, Guo WZ, Wu JG, Liu Y, Shi WZ, et al. The efficacy and cost-effectiveness of cell saver use in instrumented posterior correction and fusion surgery for scoliosis in school-aged children and adolescents. PLoS One. 2014; 9:e92997.
Article50. Stone N, Sardana V, Missiuna P. Indications and outcomes of cell saver in adolescent scoliosis correction surgery: a systematic review. Spine (Phila Pa 1976). 2017; 42:E363–E370.51. Bilgili MG, Ercin E, Peker G, Kural C, Basaran SH, Duramaz A, et al. Efficiency and cost analysis of cell saver auto transfusion system in total knee arthroplasty. Balkan Med J. 2014; 31:149–153.
Article52. Dusik CJ, Hutchison C, Langelier D. The merits of cell salvage in arthroplasty surgery: an overview. Can J Surg. 2014; 57:61–66.
Article53. Lyon TD, Ferroni MC, Turner R 2nd, Jones C, Jacobs BL, Davies BJ. Short-term outcomes of intraoperative cell saver transfusion during open partial nephrectomy. Urology. 2015; 86:1153–1158.
Article54. Elmalky M, Yasin N, Rodrigues-Pinto R, Stephenson J, Carroll C, Smurthwaite G, et al. The safety, efficacy, and cost-effectiveness of intraoperative cell salvage in metastatic spine tumor surgery. Spine J. 2017; 17:977–982.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Blood Management in Hip Replacement Arthroplasty
- Effect of Acute Normovolemic Hemodilution on Homologous Blood Saving during Off-Pump CABG
- Patient Blood Management: Anesthesiologist's Perspectives
- A Single-Center Experience of Transfusion Free Surgical Treatment over 13 Years in Korea
- Effect of Acute Normovolemic Hemodilution on Postoperative Allogenic Blood Requirement after Total Knee Arthroplasty