J Nutr Health.
2017 Apr;50(2):158-170. 10.4163/jnh.2017.50.2.158.
Study on relationship between milk intake and prevalence rates of chronic diseases in adults based on 5th and 6th Korea National Health and Nutrition Examination Survey data
- Affiliations
-
- 1Department of Statistics, Hannam University, Daejeon 34430, Korea.
- 2Department of Food and Nutrition, Kookmin University, Seoul 02707, Korea. leejs1945@kookmin.ac.kr
- KMID: 2407329
- DOI: http://doi.org/10.4163/jnh.2017.50.2.158
Abstract
- PURPOSE
The purpose of this study was to explore the relationship between milk intake and prevalence rates of chronic diseases using KNHANES data, and the significance of the relationship was tested based on meditators, socioeconomic status (income, education), dietary behaviors (smoking, alcohol drinking, breakfast, and eating out), and physical activity (walking, medium, and high).
METHODS
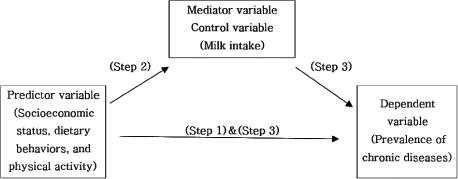
Using the 5(th) and 6(th) survey data of KNHANES, milk intake rates and presence of seven chronic diseases were summarized and analyzed by ANOVA for two groups of adult men and women as follows: hypertension, hypertriglyceridemia, low HDL-cholesterol, diabetes, abdominal obesity, obesity, and metabolic syndrome. The dependent variables for the presence of seven chronic diseases regressed with socioeconomic, dietary behavior, and physical activity variables according to Logistic models. The dependent variables for milk intake using predictor variables of socioeconomic, dietary behaviors and physical activity were analyzed according to Logistic models. Finally, the significant socioeconomic, dietary behavior, and physical activity variables in the above model along with milk intake as a control variable or mediator variable regressed with significant chronic diseases according to Logistic models.
RESULTS
Milk intake, socioeconomic status, dietary behaviors, and physical activity were significantly different among the two groups of adult men and women, which were also critical factors to the prevalence of chronic diseases. The dependent variable for prevalence of chronic diseases regressed with significant factors of socioeconomic status, dietary behavior, and physical activity variables according to chronic diseases using the control or mediator variable of milk intake and summarized as follows: For adult men, milk intake controlled the education effect on diabetes partly, alcohol on hypertension and hypertriglyceridemia, low HDL-cholesterol, metabolic syndrome, breakfast on metabolic syndrome, eating out on obesity, and medium physical activity on hypertriglyceridemia. For adult women, household income on hypertriglyceridemia, diabetes, abdominal obesity, education level on hypertension, alcohol drinking, eating out, and walking activity on abdominal obesity, alcohol, breakfast, eating out, walking activity on low HDL-cholesterol, and medium physical activity on hypertriglyceridemia and low HDL-cholesterol were partly controlled by milk intake. Other significant socioeconomic status, dietary behavior, and physical activity variables related to prevalence of chronic diseases were fully controlled or mediated by milk intake.
CONCLUSION
This study shows that milk intake (daily more than 200 g) prevents chronic diseases such as hypertension, hypertriglyceridemia, low HDL-cholesterol, diabetes, obesity, abdominal obesity, and metabolic syndrome.
MeSH Terms
Figure
Reference
-
1. Kim HR. Nutrition transition and shiting diet linked noncommunicable diseases and policy issues. Health Welf Policy Forum. 2013; 198:27–37.2. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2015: Korea National Health and Nutrition Examination Survey (KNHANES VI-3). Sejong: Korea Centers for Disease Control and Prevention;2016.3. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). Cheongju: Korea Centers for Disease Control and Prevention;2014.4. Nishida C, Uauy R, Kumanyika S, Shetty P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: process, product and policy implications. Public Health Nutr. 2004; 7(1A):245–250.
Article5. World Health Organization. Diet, nutrition and the prevention of chronic diseases. Geneva: World Health Organization;2003.6. Darnton-Hill I, Nishida C, James WP. A life course approach to diet, nutrition and the prevention of chronic diseases. Public Health Nutr. 2004; 7(1A):101–121.
Article7. Kim S, Nah EH, Cho HI. Association between smoking, metabolic syndrome, and arteriosclerosis in Korean men. J Health Info Stat. 2016; 41(1):18–26.
Article8. Park E, Choi SJ, Lee HY. The prevalence of metabolic syndrome and related risk factors based on the KNHANES V 2010. J Agric Med Community Health. 2013; 38(1):1–13.
Article9. Kwak YS. Effect of exercise on metabolic syndrome. Gwahaknonjip. 2016; 42:95–106.10. Lawlor DA, Ebrahim S, Timpson N, Davey Smith G. Avoiding milk is associated with a reduced risk of insulin resistance and the metabolic syndrome: findings from the British Women's Heart and Health Study. Diabet Med. 2005; 22(6):808–811.
Article11. Lee CJ, Joung H. Milk intake is associated with metabolic syndrome: using data from the Korea National Health and Nutrition Examination Survey 2007–2010. Korean J Community Nutr. 2012; 17(6):795–804.12. Marques-Vidal P, Gonçalves A, Dias CM. Milk intake is inversely related to obesity in men and in young women: data from the Portuguese Health Interview Survey 1998–1999. Int J Obes (Lond). 2006; 30(1):88–93.
Article13. Pereira MA, Jacobs DR Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002; 287(16):2081–2089.
Article14. Satija A, Agrawal S, Bowen L, Khandpur N, Kinra S, Prabhakaran D, Reddy KS, Smith GD, Ebrahim S. Association between milk and milk product consumption and anthropometric measures in adult men and women in India: a cross-sectional study. PLoS One. 2013; 8(4):e60739.
Article15. Sohn KH, Min SH, Lee MJ, Lee HJ. A study on the consumption of dairy beverage of female and factors affecting the consumption status. Korean J Food Nutr. 2000; 13(5):465–476.16. Talaei M, Pan A, Yuan JM, Koh WP. Dairy food intake is inversely associated with risk of hypertension: the Singapore Chinese Health Study. J Nutr. 2017; 147(2):235–241.
Article17. Lin SL, Tarrant M, Hui LL, Kwok MK, Lam TH, Leung GM, Schooling CM. The role of dairy products and milk in adolescent obesity: evidence from Hong Kong's “Children of 1997” birth cohort. PLoS One. 2012; 7(12):e52575.
Article18. Martini LA, Wood RJ. Milk intake and the risk of type 2 diabetes mellitus, hypertension and prostate cancer. Arq Bras Endocrinol Metabol. 2009; 53(5):688–694.
Article19. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary reference intakes for Koreans 2015. Sejong: Ministry of Health and Welfare;2016.20. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Cheongwon: Korea Centers for Disease Control and Prevention;2012.21. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2014: Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Cheongju: Korea Centers for Disease Control and Prevention;2015.22. National Institutes of Health (US). ATP III guidelines at-a-glance quick desk reference [Internet]. Bethesda (MD): National Institutes of Health;2001. cited 2017 Feb 2. Available from: https://www.nhlbi.nih.gov/files/docs/guidelines/atglance.pdf.23. Mann CJ. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J. 2003; 20(1):54–60.
Article24. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51(6):1173–1182.
Article25. Kutner M, Nachtsheim C, Neter JL, Li W. Applied linear statistical models. 5th ed. Boston: McGraw-Hill;2005.26. Dietz WH, Douglas CE, Brownson RC. Chronic disease prevention: tobacco avoidance, physical activity, and nutrition for a healthy start. JAMA. 2016; 316(16):1645–1646.27. Biong AS, Veierød MB, Ringstad J, Thelle DS, Pedersen JI. Intake of milk fat, reflected in adipose tissue fatty acids and risk of myocardial infarction: a case-control study. Eur J Clin Nutr. 2006; 60(2):236–244.
Article28. German JB, Gibson RA, Krauss RM, Nestel P, Lamarche B, van Staveren WA, Steijns JM, de Groot LC, Lock AL, Destaillats F. A reappraisal of the impact of dairy foods and milk fat on cardiovascular disease risk. Eur J Nutr. 2009; 48(4):191–203.
Article29. Warensjö E, Jansson JH, Berglund L, Boman K, Ahrén B, Weinehall L, Lindahl B, Hallmans G, Vessby B. Estimated intake of milk fat is negatively associated with cardiovascular risk factors and does not increase the risk of a first acute myocardial infarction. A prospective case-control study. Br J Nutr. 2004; 91(4):635–642.
Article30. Berkey CS, Rockett HR, Willett WC, Colditz GA. Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Arch Pediatr Adolesc Med. 2005; 159(6):543–550.31. Elwood PC, Pickering JE, Givens DI, Gallacher JE. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids. 2010; 45(10):925–939.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The relationship between the prevalence of anemia and dietary intake among adults according to household types based on data from the 7th (2016–2018) Korea National Health and Nutrition Examination Survey
- Yearly trend of milk intake in Korean children and adolescents and their nutritional status by the milk intake level using 2007–2015 Korea National Health and Nutrition Examination Survey
- The Changes in Obesity Prevalence and Dietary Habits in Korean Adults by Residential Area during the Last 10 Years – Based on the 4th (2007-2009) and the 7th (2016-2018) Korea National Health and Nutrition Examination Survey Data
- Relationship between intake of soft drinks and current prevalence of adult atopic dermatitis: based on the Korea National Health and Nutrition Examination Survey data (2015-2016)
- An iodine database establishment and iodine intake in Korean adults: Based on the 1998~2014 Korea National Health and Nutrition Examination Survey