Korean Circ J.
2018 Mar;48(3):217-226. 10.4070/kcj.2017.0031.
Low Common Carotid Artery Systolic Occlusion Pressure and Symptomatic Carotid Artery Stenosis Are Associated with Development of Neurologic Intolerance during Proximal Protected Carotid Artery Stenting
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea. myheart@cnu.ac.kr
- 2Department of Neurology, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea.
- 3Clinical Trial Center, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea.
- KMID: 2406925
- DOI: http://doi.org/10.4070/kcj.2017.0031
Abstract
- BACKGROUND AND OBJECTIVES
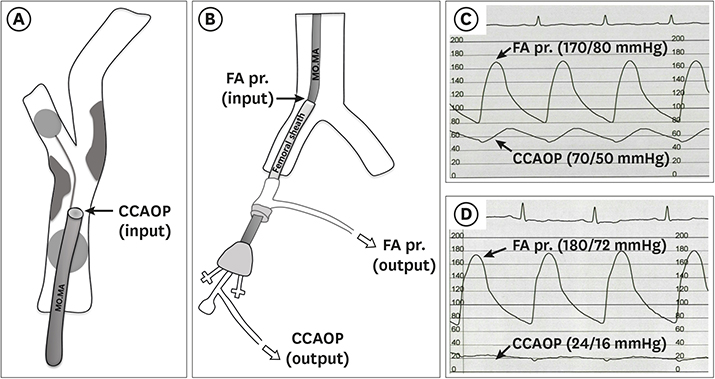
Neurologic intolerance (NI) is defined as the occurrence of neurological symptoms during carotid artery stenting (CAS). Because NI is inevitable problem, it may be helpful to anticipate its occurrence. So, we studied factors associated with NI during proximal protected CAS.
METHODS
We retrospectively analyzed all consecutive patients underwent proximal protected CAS from August 2012 to January 2017.
RESULTS
We included total 123 patients (109 males, 72±8 years old). The total procedure time was 43±12 minutes, and mean occlusion time was 4.8±1.2 minutes. We divided CAS patients into 2 groups according to presence of NI; neurologic tolerance (NT; n=74, 60%) and NI (n=49, 40%) groups. After the univariate analysis, symptomatic carotid artery stenosis (p = 0.003), absence of anterior communicating artery (p = 0.015) and low common carotid artery occlusion pressure (CCAOP, p < 0.001) were associated with NI. After the multivariate analysis, NI was significantly associated with symptomatic carotid artery stenosis (odds ratio [OR], 5.549; p = 0.014) and systolic CCAOP≤42 mmHg (OR, 6.461; p < 0.001). In NI group, 43 patients (88%) recovered right after the balloon deflation and 2 patients were normalized within 2 hours. However, 1 had major stroke and 3 had minor strokes in 4 patients with persistent NI ≥24 hours.
CONCLUSIONS
About 40% showed NI during the CAS. Most of them (88%, 43 of 49 patients) recovered after the balloon deflation, but stroke incidence was significantly higher in NI group. Symptomatic carotid artery stenosis and systolic CCAOP ≤42 mmHg were significantly associated with the development of NI during proximal protected CAS.
MeSH Terms
Figure
Cited by 2 articles
-
Proximal Protected Carotid Artery Stenting and Neurologic Intolerance: Can We Predict before Stenting?
Seung-Woon Rha
Korean Circ J. 2018;48(3):230-232. doi: 10.4070/kcj.2018.0017.Feasibility and Applicability of Wireless Handheld Ultrasound Measurement of Carotid Intima-Media Thickness in Patients with Cardiac Symptoms
Albert Youngwoo Jang, Jeongwon Ryu, Pyung Chun Oh, Jeonggeun Moon, Wook-Jin Chung
Yonsei Med J. 2020;61(2):129-136. doi: 10.3349/ymj.2020.61.2.129.
Reference
-
1. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/ SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Vasc Med. 2011; 16:35–77.2. Bersin RM, Stabile E, Ansel GM, et al. A meta-analysis of proximal occlusion device outcomes in carotid artery stenting. Catheter Cardiovasc Interv. 2012; 80:1072–1078.
Article3. Bijuklic K, Wandler A, Hazizi F, Schofer J. The PROFI study (Prevention of Cerebral Embolization by Proximal Balloon Occlusion Compared to Filter Protection During Carotid Artery Stenting): a prospective randomized trial. J Am Coll Cardiol. 2012; 59:1383–1389.4. Montorsi P, Caputi L, Galli S, et al. Microembolization during carotid artery stenting in patients with high-risk, lipid-rich plaque. A randomized trial of proximal versus distal cerebral protection. J Am Coll Cardiol. 2011; 58:1656–1663.5. Cassese S, Ndrepepa G, King LA, et al. Proximal occlusion versus distal filter for cerebral protection during carotid stenting: updated meta-analysis of randomised and observational MRI studies. EuroIntervention. 2015; 11:238–246.
Article6. Giugliano G, Stabile E, Biamino G, et al. Predictors of carotid occlusion intolerance during proximal protected carotid artery stenting. JACC Cardiovasc Interv. 2014; 7:1237–1244.7. Reimers B, Sievert H, Schuler GC, et al. Proximal endovascular flow blockage for cerebral protection during carotid artery stenting: results from a prospective multicenter registry. J Endovasc Ther. 2005; 12:156–165.8. Cremonesi A, Manetti R, Liso A, Ricci E, Bianchi P, Castriota F. Endovascular treatment of soft carotid plaques: a single-center carotid stent experience. J Endovasc Ther. 2006; 13:190–195.9. Stabile E, Salemme L, Sorropago G, et al. Proximal endovascular occlusion for carotid artery stenting: results from a prospective registry of 1,300 patients. J Am Coll Cardiol. 2010; 55:1661–1667.10. Shahidi S, Owen-Falkenberg A, Gottschalksen B. Clinical validation of 40-mmHg carotid stump pressure for patients undergoing carotid endarterectomy under general anesthesia. J Cardiovasc Surg (Torino). 2017; 58:431–438.
Article11. Montisci R, Sanfilippo R, Bura R, Branca C, Piga M, Saba L. Status of the circle of Willis and intolerance to carotid cross-clamping during carotid endarterectomy. Eur J Vasc Endovasc Surg. 2013; 45:107–112.
Article12. Bagan P, Vidal R, Martinod E, et al. Cerebral ischemia during carotid artery cross-clamping: predictive value of phase-contrast magnetic resonance imaging. Ann Vasc Surg. 2006; 20:747–752.
Article13. Diederich KW, Scheinert D, Schmidt A, et al. First clinical experiences with an endovascular clamping system for neuroprotection during carotid stenting. Eur J Vasc Endovasc Surg. 2004; 28:629–633.
Article14. White CJ. Carotid artery stenting. J Am Coll Cardiol. 2014; 64:722–731.
Article15. Howell M, Krajcer Z, Dougherty K, et al. Correlation of periprocedural systolic blood pressure changes with neurological events in high-risk carotid stent patients. J Endovasc Ther. 2002; 9:810–816.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Carotid Artery Occlusive Diseases Treated with Staged Subclavian-carotid Artery bypass and Carotid Endarterectomy: Case Report
- A Case of Transseptal Approach to Carotid Artery Stenting in Right Internal Carotid Stenosis
- Carotid Artery Stenting
- Proximal Protected Carotid Artery Stenting and Neurologic Intolerance: Can We Predict before Stenting?
- Carotid Artery Stenting in a Patient with Spontaneous Recanalization of a Proximal Internal Carotid Artery Occlusion: a Case Report