Change of Cancer Symptom, Depression and Quality of Life based on Phases of Chemotherapy in Patients with Colorectal or Stomach Cancer: A Prospective Study
- Affiliations
-
- 1Department of Nursing, Sahmyook University, Seoul, Korea. ohpj@syu.ac.kr
- 2Department of Nursing, Graduate School, Sahmyook University, Seoul, Korea.
- KMID: 2406329
- DOI: http://doi.org/10.7475/kjan.2017.29.3.313
Abstract
- PURPOSE
The purpose of this study was to identify over time the changes of cancer symptom, depression and quality of life (QOL) among people who had stomach or colorectal cancer.
METHODS
Of the 74 participants recruited, 67 participated in the study. Participants were asked to complete three instruments at three different time. The instruments were the M. D. Anderson Symptom Inventory-Gastrointestinal Cancer Module, Hospital Anxiety Depression Scale, and the Functional Assessment of Cancer Therapy-General. The questionnaires were administered before chemotherapy, toward the end of chemotherapy, and six months after the completion of adjuvant therapy. Data were analyzed using descriptive statistics and repeated measure ANOVA.
RESULTS
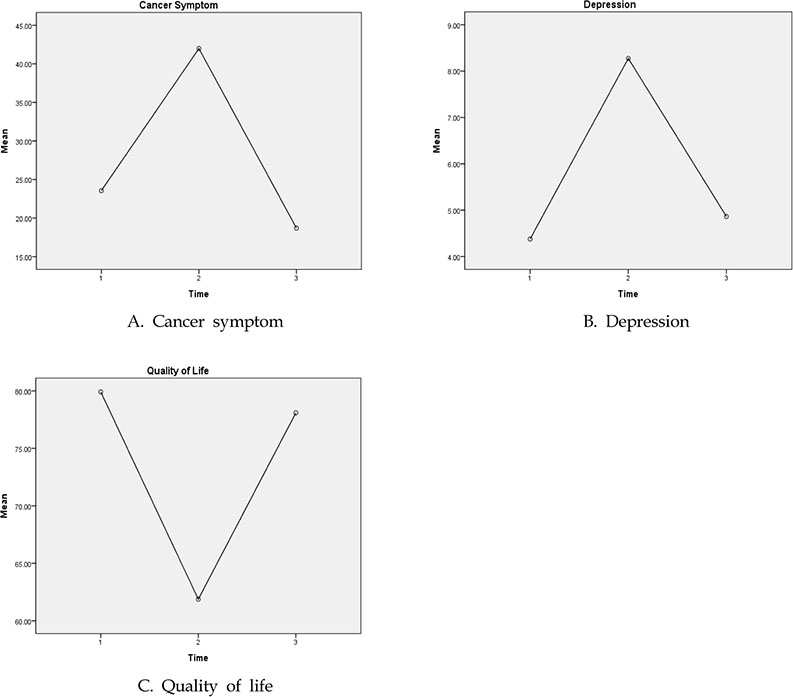
At the immediately after chemotherapy point, the most frequent symptom was lack of appetite, followed by fatigue and problem with remembering things. The mean score for depression was 8.27 with a prevalence of 31.3%. The mean score for quality of life was 61.88 out of 135. Repeated measures ANOVA showed a significant increase in cancer symptom (F=23.22, p < .001) and depression (F=35.29, p < .001) after chemotherapy. However, improvement was observed 6 months after the completion of chemotherapy. QOL (F=33.73, p < .001) also showed similar patterns as observed with cancer symptom and depression. Cancer symptom was the strongest predictor of QoL at pre-chemotherapy point. but depression was the strongest predictor at immediately after chemotherapy point.
CONCLUSION
Chemotherapy is highly associated with cancer symptom, depression and QOL in patients with cancer. The nursing intervention is needed to relieve depression as well as cancer symptoms to improve QOL in patients undergoing chemotherapy from baseline to follow-up.
MeSH Terms
Figure
Cited by 4 articles
-
Changes of Cognitive Function and Fatigue following Chemotherapy in Patients with Gastrointestinal Cancer: A Prospective Controlled Study
Pok-Ja Oh, Sun Mi Moon
Asian Oncol Nurs. 2019;19(3):126-134. doi: 10.5388/aon.2019.19.3.126.Oxaliplatin-induced Peripheral Neuropathy, Symptoms, Distress and Quality of Life among Korean Patients with Gastrointestinal Cancer
Hye Jeong Jung, Soo jung Ahn, Yoo Ri Yang, Kyoung A Kim, Sang Joon Shin, Min Kyu Jung, Sang Hui Chu
Asian Oncol Nurs. 2019;19(4):204-213. doi: 10.5388/aon.2019.19.4.204.Predictors of Quality of Life and Social Support as a Mediator between Defecation Function and Quality of Life among Rectal Cancer Patients
Jung Rang Kim, Seon Young Hwang
Korean J Adult Nurs. 2019;31(5):487-495. doi: 10.7475/kjan.2019.31.5.487.Symptom Distress and Depression in Patients with Recurrent Gynecologic Cancer Undergoing Chemotherapy: Mediating Effect of Resilience
Eun Jung Yang, Ho Sihn Ryu
Korean J Adult Nurs. 2019;31(1):28-37. doi: 10.7475/kjan.2019.31.1.28.
Reference
-
1. Ministry of Health & Welfare. Korean Central Cancer Registry & National Cancer Center. Annual report of cancer statistics in Korea, 2013. Seoul: Korea Cancer Center Registry;2015.2. Jeong G, Kim KH, Kwak YH. Quality of life in colorectal cancer patients according to the severity of symptom clusters classification. Asian Oncol Nurs. 2014; 14(2):74–83. DOI: 10.5388/aon.2014.14.2.74.
Article3. Kim JH, Kim HJ. Influences of symptom experience and depression on quality of life in colorectal cancer patients with stoma reversal. J Korean Biol Nurs Sci. 2015; 17(4):306–314. DOI: 10.7586/jkbns.2015.17.4.306.
Article4. Byar KL, Berger AM, Bakken SL, Cetak MA. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life. Oncol Nurs Forum. 2006; 33(1):E18–E26. DOI: 10.1188/06.ONF.E18-E26.
Article5. Baek YA, Yi MS. Factors influencing quality of life chemotherapy for colorectal cancer patients in Shouth Korea. J Korean Acad Nurs. 2015; 45(4):604–612. DOI: 10.4040/jkan.2015.45.4.604.6. Tavoli A, Mohagheghi MA, Montazeri A, Roshan R, Tavoli Z, Omidvari S. Anxiety and depression in patient with gastrointestinal cancer: dose knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007; 7:28. DOI: 10.1186/1471-230X-7-28.
Article7. Fox SW, Lyon DE. Symptom clusters and quality of life in survivors of lung cancer. Oncol Nurs Forum. 2006; 33(5):931–936.
Article8. Li Q, Lin Y, Liu X, Xu Y. A systematic review on patient-reported outcomes in cancer survivors of randomized clinical trials: direction for future research. Psychooncology. 2014; 23(7):721–730. DOI: 10.1002/pon.3504.9. Xiao W, Chow KM, So WK, Leung DY, Chan CW. The effectiveness of psychoeducational intervention on managing symptom clusters in patients with cancer: a systematic review of randomized controlled trials. Cancer Nurs. 2016; 39(4):279–291. DOI: 10.1097/ncc.0000000000000313.10. Parahoo K, McCaughan E, Noyes J, McDonough S. Psychosocial interventions for men with prostate cancer. Cochrane Database Syst Rev. 2013; (12):CD008529. DOI: 10.1002/14651858.cd008529.pub2.
Article11. Chow KM, Chan JCY, Choi KKC, Chan CWH. A review of psychoeducational interventions to improve sexual functioning, quality of life, and psychologica outcomes in gynecological cancer patients. Cancer Nurs. 2016; 39(1):20–31. DOI: 10.1097/ncc.0000000000000234.12. Park JH, Bae SH, Jung YM. Changes of symptom distress and quality of life in breast cancer patients receiving adjuvant therapy. Asian Oncol Nurs. 2015; 15(2):67–74. DOI: 10.5388/aon.2015.15.2.67.
Article13. Wang XS, Williams LA, Eng C, Mendoza TR, Shah NA, Kirkendoll KJ, et al. Validation and application of a module of the M. D. Anderson Symptom Inventory for measuring multiple symptoms in patients with gastrointestinal cancer (the MDASI-GI). Cancer. 2010; 116(8):2053–2063. DOI: 10.1002/cncr.24920.
Article14. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370. DOI: 10.1111/j.1600-0447.1983.tb09716.x.
Article15. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999; 38(2):289–296.16. Kim H, Yoo HJ, Kim YJ, Han OS, Lee KH, Lee JH, et al. Development and validation of Korean functional assessment cancer therapy-general (FACT-G). Korean J Clin Psychol. 2003; 22(1):215–229.17. Chaiy SI. Soical science research methodology. Seoul: Hakhyunsa;2000.18. Hofsø K, Miaskowski C, Bjordal K, Cooper BA, Rustøen T. Previous chemotherapy influences the symptom experience and quality of life of women with breast cancer prior to radiation therapy. Cancer Nurs. 2012; 35(3):167–177. DOI: 10.1097/NCC.0b013e31821f5eb5.
Article19. Gehring K, Roukema JA, Sitskoorn MM. Review of recent studies on interventions for cognitive deficits in patients with cancer. Expert Rev Anticancer Ther. 2012; 12(2):255–269. DOI: 10.1586/era.11.202.
Article20. Kim MY. Transition of symptoms and quality of life in cancer patients on chemotherapy. J Korean Acad Nurs. 2009; 39(3):433–445. DOI: 10.4040/jkan.2009.39.3.433.
Article21. Lee JR. A structural model for chemotherapy related cognitive change in breast cancer patients [dissertation]. Seoul: Sahmyook University;2016.22. Kim HJ, Kim SH, Lee HK, Oh SE. Factors affecting symptom experiences of breast cancer patients: based on the theory of unpleasant symptoms. Asian Oncol Nurs. 2014; 14(1):7–14. DOI: 10.5388/aon.2014.14.1.7.
Article23. Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008; 30(2):112–126. DOI: 10.1016/j.genhosppsych.2007.10.008.
Article24. Hurria A, Hurria A, Zuckerman E, Panageas KS, Fornier M, D'Andrea G, et al. A prospective longitudinal study of the functional status and quality of life of older patients with breast cancer receiving adjuvant chemotherapy. J Am Geriatr Soc. 2006; 54(7):1119–1124. DOI: 10.1111/j.1532-5415.2006.00789.x.
Article25. Tsunoda A, Nakao K, Hiratsuka K, Yasuda N, Shibusawa M, Kusano M. Anxiety, depression and quality of life in colorectal cancer patients. Int J Clin Oncol. 2005; 10(6):411–417. DOI: 10.1007/s10147-005-0524-7.
Article26. Reyes-Gibby CC, Anderson KO, Morrow PK, Shete S, Hassan S. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health (Larchmt). 2012; 21(3):311–318. DOI: 10.1089/jwh.2011.2852.
Article27. Park JH, Jun EY, Kang MY, Joung YS, Kim GS. Symptom experience and quality of life in breast cancer survivors. J Korean Acad Nurs. 2009; 39(5):613–621. DOI: 10.4040/jkan.2009.39.5.613.
Article28. Park JS, Oh YJ. The effects of psychosocial intervention on depression, hope and quality of life of home-based cancer patients. Korean Journal of Adult Nursing. 2010; 22(6):594–605.29. Bevans M. Health-related quality of life following allogeneic hematopoietic stem cell transplantation. Hematology Am Soc Hematol Educ Program. 2010; 2010:248–254. DOI: 10.1182/asheducation-2010.1.248.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influencing Factors on Depression in Stomach Cancer Patients Receiving Chemotherapy
- Symptom Cluster and Quality of Life in Patients with Breast Cancer undergoing Chemotherapy
- Factors Influencing Quality of Life during Chemotherapy for Colorectal Cancer Patients in South Korea
- Influences of Symptom Experience and Depression on Quality of Life in Colorectal Cancer Patients with Stoma Reversal
- The Trajectory of Fatigue and Quality of Life in Stomach Cancer Patients Receiving Chemotherapy