Anesth Pain Med.
2017 Oct;12(4):320-325. 10.17085/apm.2017.12.4.320.
Comparison of several dosing schedules of intravenous dexmedetomidine in elderly patients under spinal anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea. yeomjh@hanyang.ac.kr
- KMID: 2405848
- DOI: http://doi.org/10.17085/apm.2017.12.4.320
Abstract
- BACKGROUND
Many clinicians have probably used subjective, unscientific methods for dose reduction to avoid overdose in elderly patients. The aim of this study was to compare several dosing schedules of intravenous dexmedetomidine (DEX) to identify the appropriate dosing schedule within the therapeutic dose range for adequate sedation of elderly patients under spinal anesthesia.
METHODS
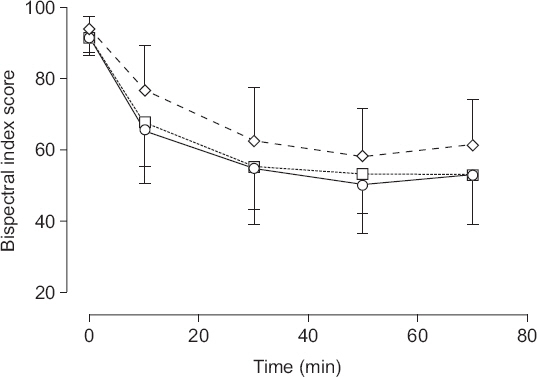
After administration of spinal anesthesia, a loading dose of DEX was injected over 10 min in three groups with the following dosages: group A, 1.0 μg/kg of actual body weight; group B, 1.0 μg/kg of ideal body weight (IBW); and group C, 0.8 μg/kg of IBW. Then, a maintenance infusion (0.5 μg/kg of each BW/h) was administered. The bispectral index score (BIS), the time required to reach BIS 80, airway obstruction score, and the occurrence of bradycardia were recorded.
RESULTS
The changes in the BIS among the groups over time were found to have statistically significant differences (P < 0.001). The times required to reach BIS 80 were 6.1 ± 5.3 min, 5.0 ± 3.6 min, and 11.0 ± 8.6 min in groups A, B, and C, respectively (P < 0.001). The airway obstruction score and the frequency of bradycardia did not have statistically significant differences among the groups.
CONCLUSIONS
An initial loading dose of DEX that is 0.8 μg/kg of IBW over 10 min, followed by an infusion rate of less than 0.5 μg/kg of IBW/h may be adequate for sedation in elderly patients receiving spinal anesthesia.
MeSH Terms
Figure
Reference
-
1. Son MS. Health Insurance Main Statistics of Health Insurance Review and Assessment Service of Korea. 12th ed. Wonju: Dahamgge Co-op;2016. p. ii.2. Sung SH. Operation Statistics Annual Report of National Health Insurance Service. Wonju: Dahamgge Co-op;2016; 2.3. Falzone E, Hoffmann C, Keita H. Postoperative analgesia in elderly patients. Drugs Aging. 2013; 30:81–90. DOI: 10.1007/s40266-012-0047-7. PMID: 23288604.4. Corsonello A, Pedone C, Incalzi RA. Age-related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr Med Chem. 2010; 17:571–84. DOI: 10.2174/092986710790416326. PMID: 20015034.5. Shi S, Klotz U. Age-related changes in pharmacokinetics. Curr Drug Metab. 2011; 12:601–10. DOI: 10.2174/138920011796504527. PMID: 21495970.6. Johson JO, Grecu L, Lawson NW. Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, editors. Autonomic nervous system. Clinical Anesthesia. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2009. p. 355.7. Arain SR, Ebert TJ. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002; 95:461–6. DOI: 10.1097/00000539-200208000-00042.8. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–94. DOI: 10.1097/00000542-200008000-00016. PMID: 10910487.9. Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, Pocock SJ, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation:two randomized controlled trials. JAMA. 2012; 307:1151–60. DOI: 10.1001/jama.2012.304. PMID: 22436955.10. Tellor BR, Arnold HM, Micek ST, Kollef MH. Occurrence and predictors of dexmedetomidine infusion intolerance and failure. Hosp Pract (1995). 2012; 40:186–92. DOI: 10.3810/hp.2012.02.959. PMID: 22406894.11. Smithburger PL, Smith RB, Kane-Gill SL, Empey PE. Patient predictors of dexmedetomidine effectiveness for sedation in intensive care units. Am J Crit Care. 2014; 23:160–5. DOI: 10.4037/ajcc2014678. PMID: 24585165. PMCID: PMC4132632.12. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–94. DOI: 10.1097/00000542-200008000-00016. PMID: 10910487.13. Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care. 2000; 4:302–8. DOI: 10.1186/cc712. PMID: 11056756.14. Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999; 90:1502–16. DOI: 10.1097/00000542-199906000-00003. PMID: 10360845.15. Park SH, Shin YD, Yu HJ, Bae JH, Yim KH. Comparison of two dosing schedules of intravenous dexmedetomidine in elderly patients during spinal anesthesia. Korean J Anesthesiol. 2014; 66:371–6. DOI: 10.4097/kjae.2014.66.5.371.16. Song J, Kim WM, Lee SH, Yoon MH. Dexmedetomidine for sedation of patients undergoing elective surgery under regional anesthesia. Korean J Anesthesiol. 2013; 65:203–8. DOI: 10.4097/kjae.2013.65.3.203. PMID: 24101953. PMCID: PMC3790030.17. Ok HG, Baek SH, Baik SW, Kim HK, Shin SW, Kim KH. Optimal dose of dexmedetomidine for sedation during spinal anesthesia. Korean J Anesthesiol. 2013; 64:426–31. DOI: 10.4097/kjae.2013.64.5.426. PMID: 23741565. PMCID: PMC3668104.18. Sim JH, Yu HJ, Kim ST. The effects of different loading doses of dexmedetomidine on sedation. Korean J Anesthesiol. 2014; 67:8–12. DOI: 10.4097/kjae.2014.67.1.8. PMID: 25097732. PMCID: PMC4121500.19. Yeom JH, Oh MK, Ahn DW, Park SI. A loading dose of 1 µg/kg and maintenance dose of 0.5 µg/kg/h of dexmedetomidine for sedation under spinal anesthesia may induce excessive sedation and airway obstruction. Anesth Pain Med. 2016; 11:255–9. DOI: 10.17085/apm.2016.11.3.255.20. Riker RR, Fraser GL. Adverse events associated with sedatives, analgesics, and other drugs that provide patient comfort in the intensive care unit. Pharmacotherapy. 2005; 25:S8–18. DOI: 10.1592/phco.2005.25.5_Part_2.8S.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of two dosing schedules of intravenous dexmedetomidine in elderly patients during spinal anesthesia
- Effect of Dexmedetomidine on the Corrected QT and Tp-e Intervals during Spinal Anesthesia
- Fatal pulmonary aspiration during balanced sedation with dexmedetomidine and midazolam: A case report
- Fluid loading during spinal anesthesia can reduce bradycardia after intravenous dexmedetomidine infusion
- Laparoscopic appendectomy under spinal anesthesia with dexmedetomidine infusion