J Korean Soc Radiol.
2018 Mar;78(3):147-156. 10.3348/jksr.2018.78.3.147.
Role of Magnetic Resonance Cholangiopancreatography in Evaluation of Choledocholithiasis in Patients with Suspected Cholecystitis
- Affiliations
-
- 1Department of Radiology, Nowon Eulji Medical Center, Eulji University, Seoul, Korea. jyy@eulji.ac.kr
- 2Department of Preventive Medicine, School of Medicine, Eulji University, Seoul, Korea.
- KMID: 2405716
- DOI: http://doi.org/10.3348/jksr.2018.78.3.147
Abstract
- PURPOSE
To determine the role of magnetic resonance cholangiopancreatography (MRCP) in evaluation of choledocholithiasis in patients with suspected cholecystitis.
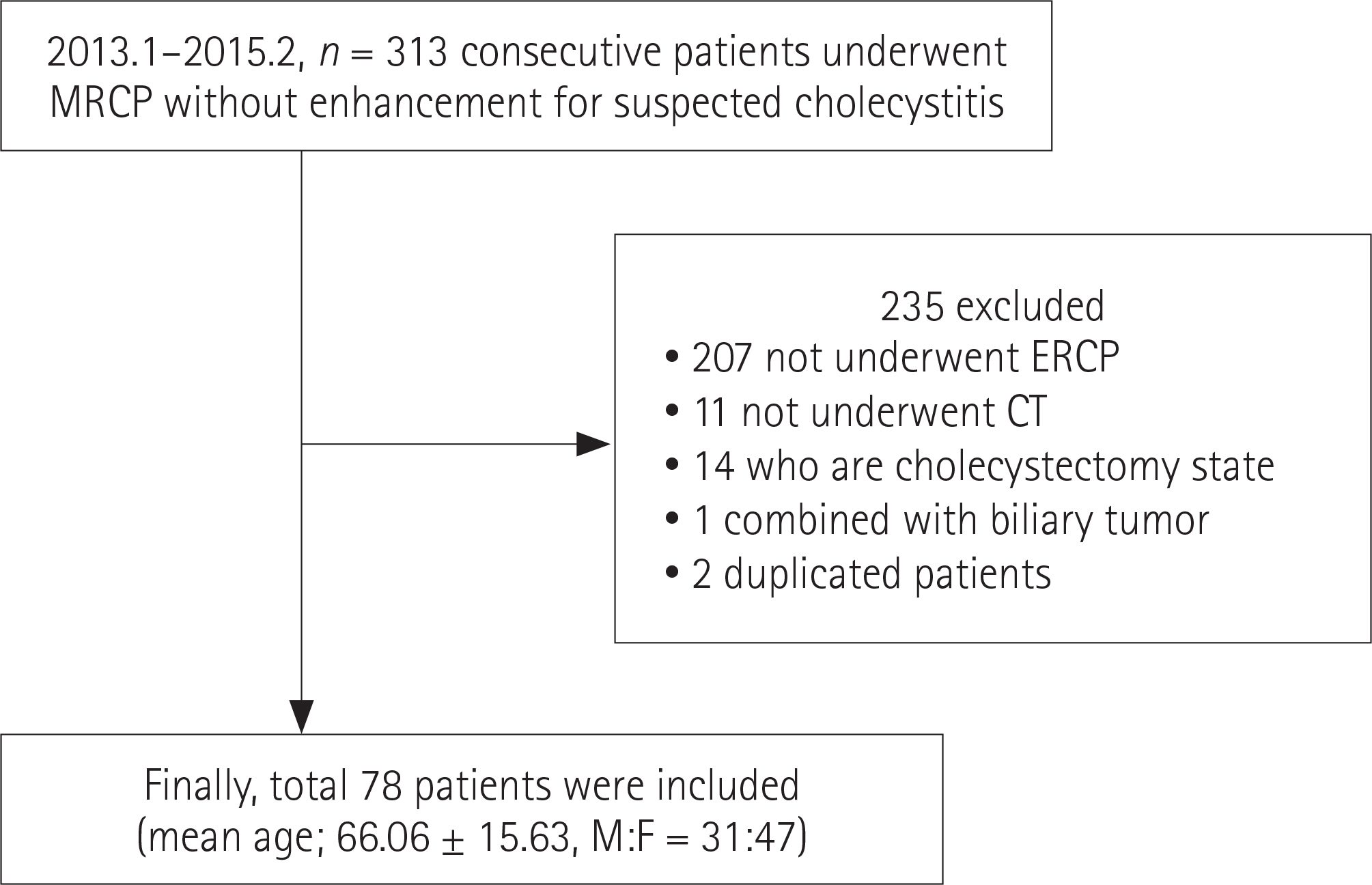
MATERIALS AND METHODS
A total of 78 patients (mean age: 66.06 ± 15.63 years; range: 21-94 years, Male:Female = 31:47) who had experienced symptoms of cholecystitis and who underwent computed tomography (CT), MRCP, and endoscopic retrograde cholangiopancreatography from January 2013 to February 2015 were included in this study. Two reviewers independently interpreted CT and MRCP images to determine the presence or absence of choledocholithiasis and cholelithiasis. Diagnostic performance (sensitivity, specificity, positive predictive value, negative predictive value, and accuracy) was compared between CT and MRCP. Interobserver agreement was also evaluated.
RESULTS
Forty-three patients underwent cholecystectomy. The accuracy of CT and MRCP for detection of gallbladder stones showed no significant difference. The sensitivity and accuracy of MRCP for detection of extrahepatic duct stones were superior to those of CT for both reviewers (reviewer 1: MRCP: sensitivity, 73.3%; accuracy, 76.9%; CT: sensitivity, 50%, accuracy 59%; p = 0.01; reviewer 2: MRCP: sensitivity, 75%; accuracy, 73.1%; CT: sensitivity, 50%; accuracy, 56.4%; p = 0.018). The interobserver agreement was consistent for both CT (k-value: 0.738) and MRCP (k-value: 0.701).
CONCLUSION
MRCP showed superior diagnostic performance for the detection of choledocholithiasis with reliable interobserver agreement. Considering the lack of radiation and contrast enhancement, MRCP would be an appropriate first-line modality in evaluation of common bile duct stones in patients with suspected cholecystitis.
MeSH Terms
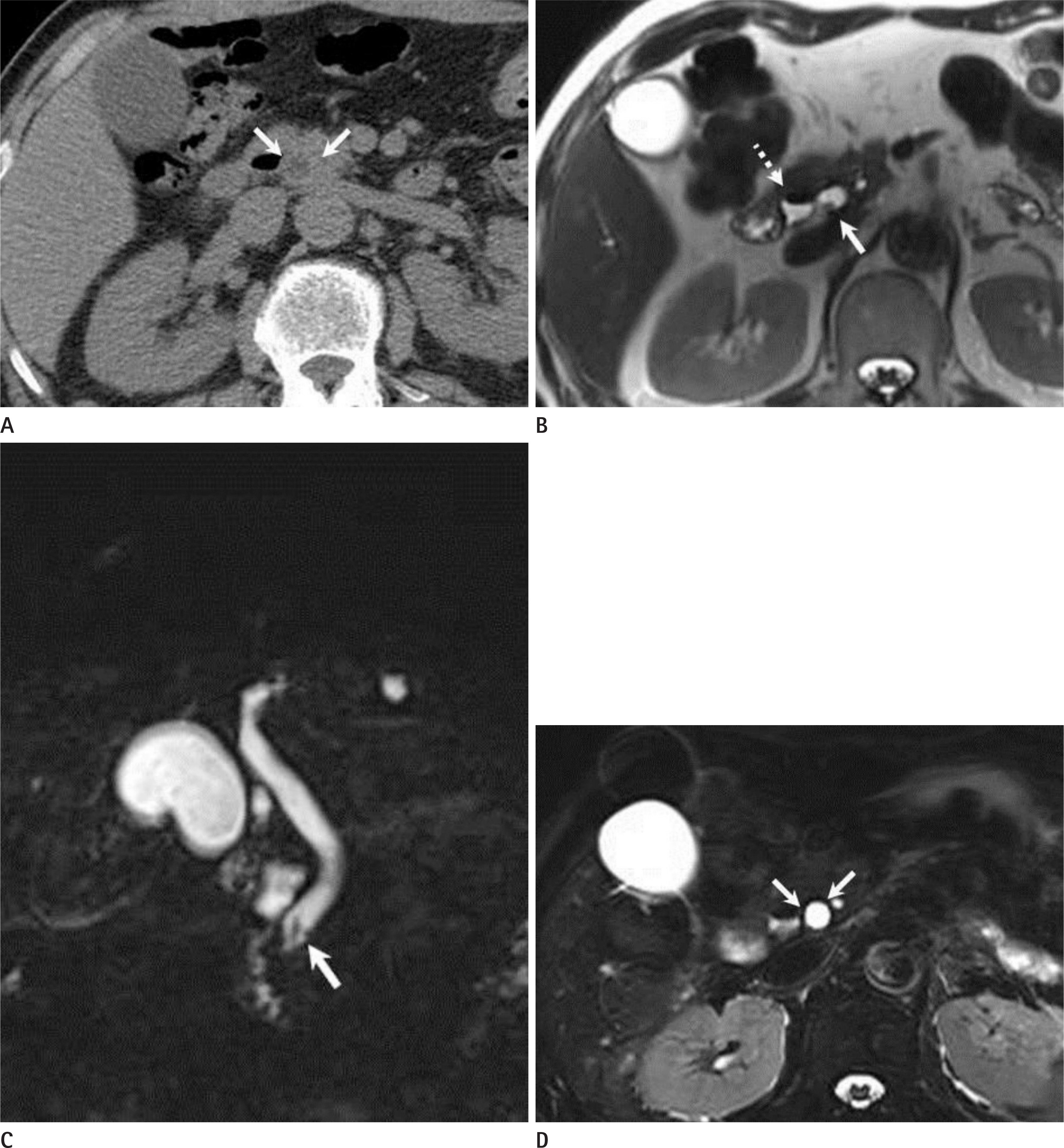
Figure
Reference
-
References
1. Chen W, Mo JJ, Lin L, Li CQ, Zhang JF. Diagnostic value of magnetic resonance cholangiopancreatography in choledocholithiasis. World J Gastroenterol. 2015; 21:3351–3360.
Article2. Bahram M, Gaballa G. The value of preoperative magnetic resonance cholangiopancreatography (MRCP) in management of patients with gall stones. Int J Surg. 2010; 8:342–345.
Article3. Wong HP, Chiu YL, Shiu BH, Ho LC. Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. J Hepatobiliary Pancreat Sci. 2012; 19:458–464.
Article4. S¸urlin V, Sa˘ftoiu A, Dumitrescu D. Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol. 2014; 20:16544–16549.5. Yun EJ, Choi CS, Yoon DY, Seo YL, Chang SK, Kim JS, et al. Combination of magnetic resonance cholangiopancreatography and computed tomography for preoperative diagnosis of the Mirizzi syndrome. J Comput Assist Tomogr. 2009; 33:636–640.
Article6. Ward WH, Fluke LM, Hoagland BD, Zarow GJ, Held JM, Ricca RL. The role of magnetic resonance cholangiopancreatography in the diagnosis of choledocholithiasis: do benefits outweigh the costs? Am Surg. 2015; 81:720–725.
Article7. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013; 20:35–46.
Article8. Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, et al. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. Am J Gastroenterol. 2001; 96:2900–2904.
Article9. Singh A, Mann HS, Thukral CL, Singh NR. Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. J Clin Diagn Res. 2014; 8:103–107.
Article10. Petrescu I, Bratu AM, Petrescu S, Popa BV, Cristian D, Burcos T. CT vs. MRCP in choledocholithiasis jaundice. J Med Life. 2015; 8:226–231.11. Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005; 54:271–275.
Article12. Moon JH, Cho YD, Cha SW, Cheon YK, Ahn HC, Kim YS, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005; 100:1051–1057.
Article13. Aydelotte JD, Ali J, Huynh PT, Coopwood TB, Uecker JM, Brown CV. Use of magnetic resonance cholangiopancreatography in clinical practice: not as good as we once thought. J Am Coll Surg. 2015; 221:215–219.
Article14. Nebiker CA, Baierlein SA, Beck S, von Flüe M, Ackermann C, Peterli R. Is routine MR cholangiopancreatography (MRCP) justified prior to cholecystectomy? Langenbecks Arch Surg. 2009; 394:1005–1010.
Article15. Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013; 17:863–871.
Article16. Scaffidi MG, Luigiano C, Consolo P, Pellicano R, Giacobbe G, Gaeta M, et al. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangio-pancreatography in the diagnosis of common bile duct stones: a prospective comparative study. Minerva Med. 2009; 100:341–348.17. De Waele E, Op de Beeck B, De Waele B, Delvaux G. Magnetic resonance cholangiopancreatography in the preoperative assessment of patients with biliary pancreatitis. Pancreatol-ogy. 2007; 7:347–351.18. Romagnuolo J, Currie G. Calgary Advanced Therapeutic Endoscopy Center study group. Noninvasive vs. selective invasive biliary imaging for acute biliary pancreatitis: an economic evaluation by using decision tree analysis. Gastrointest Endosc. 2005; 61:86–97.
Article19. Aljebreen AM. Role of endoscopic ultrasound in common bile duct stones. Saudi J Gastroenterol. 2007; 13:11–16.
Article20. Polistina FA, Frego M, Bisello M, Manzi E, Vardanega A, Perin B. Accuracy of magnetic resonance cholangiography compared to operative endoscopy in detecting biliary stones, a single center experience and review of literature. World J Radiol. 2015; 7:70–78.
Article21. Ueno K, Ajiki T, Sawa H, Matsumoto I, Fukumoto T, Ku Y. Role of intraoperative cholangiography in patients whose biliary tree was evaluated preoperatively by magnetic resonance cholangiopancreatography. World J Surg. 2012; 36:2661–2665.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of gallstone
- US Diagnosis of Choledocholithiasis in Patients with Acute Cholecystitis: Its Clinical Significance
- Sensitivity and Specificity of Magnetic Resonance Cholangiopancreatography versus Endoscopic Ultrasonography against Endoscopic Retrograde Cholangiopancreatography in Diagnosing Choledocholithiasis: The Indonesian Experience
- A Case of an Accessory Cystic Duct Draining into the Right Intrahepatic Duct
- Optimal Evaluation of Suspected Choledocholithiasis: Does This Patient Really Have Choledocholithiasis?