Korean Circ J.
2018 Jan;48(1):36-47. 10.4070/kcj.2017.0036.
The J-curve between Diastolic Blood Pressure and Risk of All-cause and Cardiovascular Death
- Affiliations
-
- 1Department of Epidemiology and Health Promotion, Institute for Health Promotion, Graduate School of Public Health, Yonsei University, Seoul, Korea. jsunha@yuhs.ac
- 2Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
- 3Health Insurance Policy Research Institute, National Health Insurance Service, Wonju, Korea.
- KMID: 2405044
- DOI: http://doi.org/10.4070/kcj.2017.0036
Abstract
- BACKGROUND AND OBJECTIVES
The J-curve phenomenon between diastolic blood pressure (DBP) and mortality has been reported repeatedly in treated patients. However, the baseline risk of low DBP has not been fully explored. This study was to examine the relationship between DBP and risk of mortality from all-cause, atherosclerotic vascular diseases (ASCVD), and ischemic heart disease (IHD) using a prospective cohort of general population.
METHODS
We analyzed 1,234,435 participants of the Korean Cancer Prevention Study cohort (789,255 men, 30-95 years of age) who had a medical evaluation from 1992 to 1995 using Cox proportional hazards models.
RESULTS
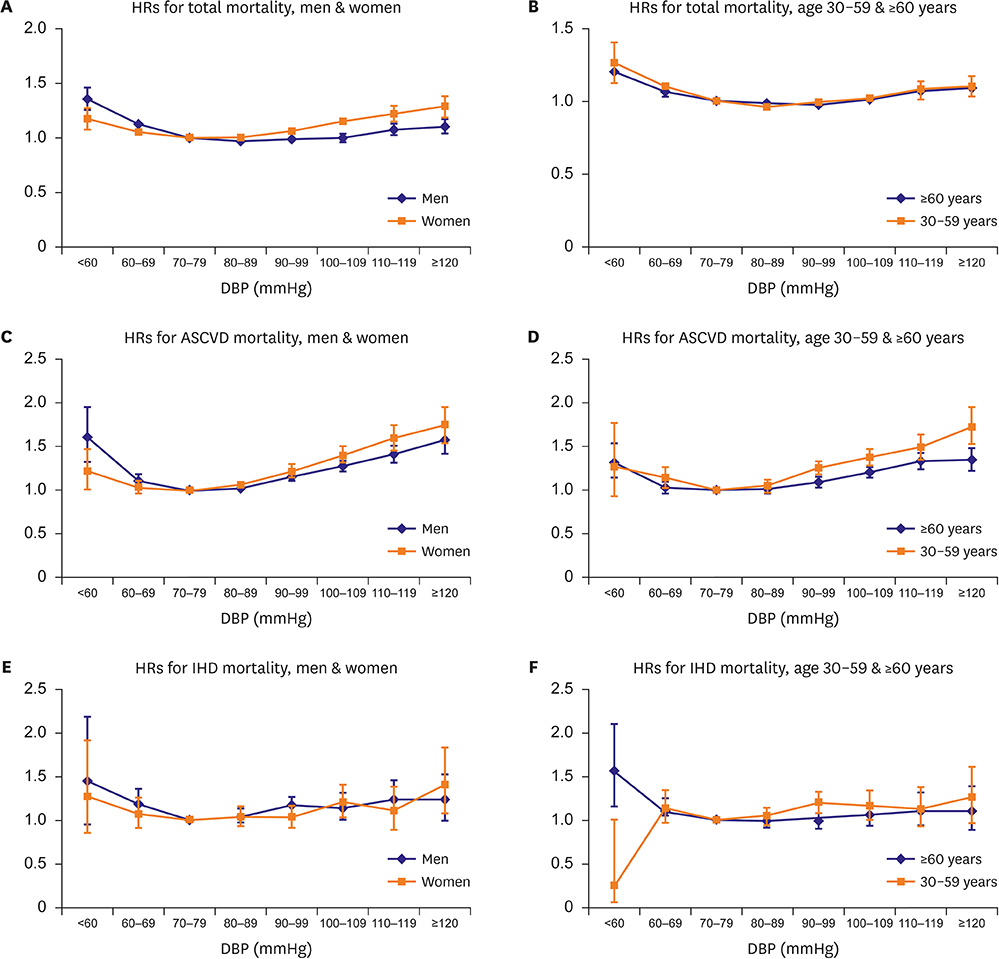
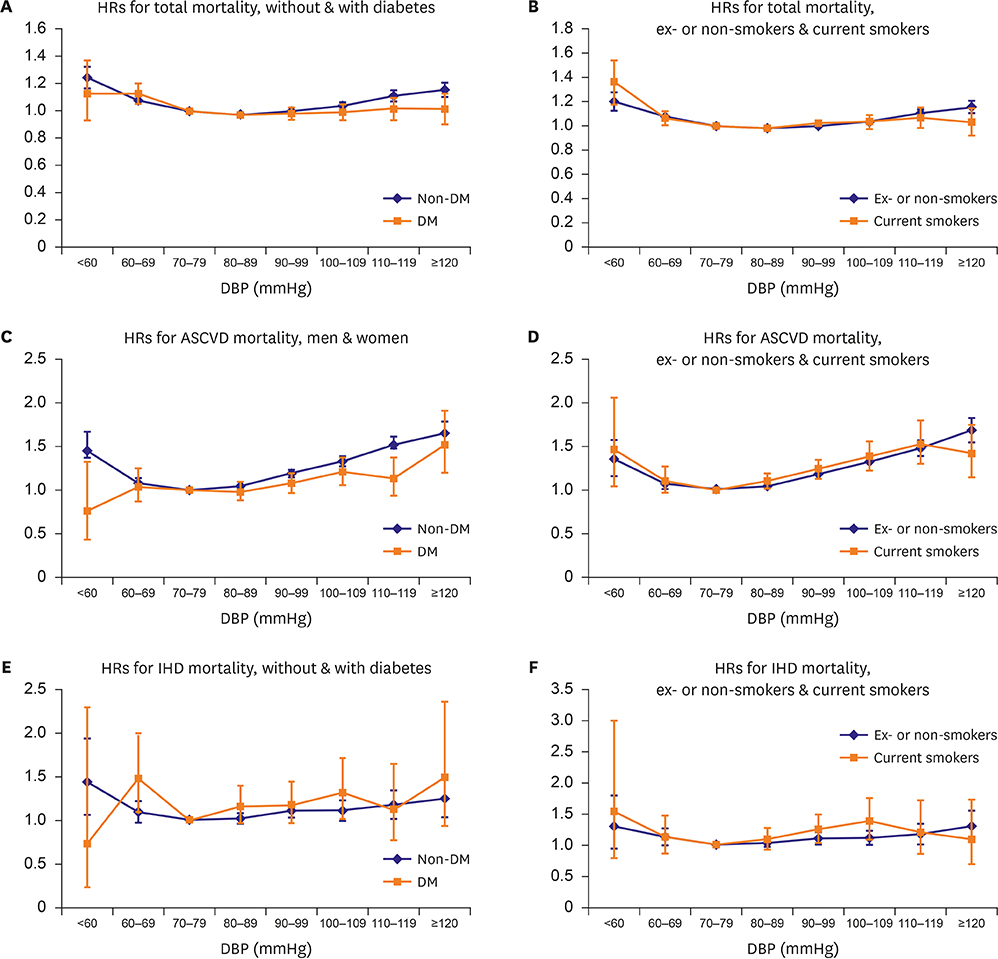
A total of 22.5 million person-years were followed up (mean age 46.6 years, deaths 193,903 cases). The hazard ratios of mortality from all-cause and ASCVD, among those with DBP < 60 mmHg compared to 70-79 mmHg were 1.23 (95% confidence interval [CI], 1.16-1.30) and 1.37 (95% CI, 1.20-1.57), respectively, after adjustment for multivariable including systolic blood pressure. Increased risks of all-cause death in the lowest DBP category group were maintained in men or women, 30-59 or ≥60 years of age, smoker or non-smoker and diabetes mellitus (DM) or non-DM subgroups. The risk in DBP 60-69 mmHg groups increased in several subgroups. However, the risk for ASCVD death in 30-59 years and DM group, and risk for IHD death in most subgroups except for elderly (≥60 years) decreased.
CONCLUSION
A J-curve relationship between low DBP and all-cause death was found consistently. The baseline risk in the general population may be considered for risk assessment, particularly in case of interventions that lower DBP below 60 mmHg.
MeSH Terms
Figure
Cited by 3 articles
-
Updated Reasons and Clinical Implications of New Korean Hypertension Guidelines for Cardiologists
Jinho Shin, Myeong-Chan Cho
Korean Circ J. 2020;50(6):476-484. doi: 10.4070/kcj.2019.0338.J-curve Phenomenon Might Be Inherent: How to Know If It Is Treatment Induced?
Jinho Shin
Korean Circ J. 2018;48(1):80-81. doi: 10.4070/kcj.2017.0356.Ideal Target Blood Pressure in Hypertension
Sungha Park
Korean Circ J. 2019;49(11):1002-1009. doi: 10.4070/kcj.2019.0261.
Reference
-
1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–1913.2. Mancia G, Grassi G. Aggressive blood pressure lowering is dangerous: the J-curve: pro side of the arguement. Hypertension. 2014; 63:29–36.3. Farnett L, Mulrow CD, Linn WD, Lucey CR, Tuley MR. The J-curve phenomenon and the treatment of hypertension. Is there a point beyond which pressure reduction is dangerous? JAMA. 1991; 265:489–495.
Article4. Egan BM, Kai B, Wagner CS, et al. Low blood pressure is associated with greater risk for cardiovascular events in treated adults with and without apparent treatment-resistant hypertension. J Clin Hypertens (Greenwich). 2017; 19:241–249.
Article5. Messerli FH, Mancia G, Conti CR, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006; 144:884–893.
Article6. Franklin SS, Gokhale SS, Chow VH, et al. Does low diastolic blood pressure contribute to the risk of recurrent hypertensive cardiovascular disease events? The Framingham Heart Study. Hypertension. 2015; 65:299–305.7. Vidal-Petiot E, Ford I, Greenlaw N, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016; 388:2142–2152.
Article8. McEvoy JW, Chen Y, Rawlings A, et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control. J Am Coll Cardiol. 2016; 68:1713–1722.9. Park H, Hong YJ, Cho JY, et al. Blood pressure targets and clinical outcomes in patients with acute myocardial infarction. Korean Circ J. 2017; 47:446–454.
Article10. Lawes CM, Rodgers A, Bennett DA, et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003; 21:707–716.11. Kikuya M, Ohkubo T, Asayama K, et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: the Ohasama study. Hypertension. 2005; 45:240–245.12. Vishram JK, Borglykke A, Andreasen AH, et al. Impact of age on the importance of systolic and diastolic blood pressures for stroke risk: the MOnica, Risk, Genetics, Archiving, and Monograph (MORGAM) Project. Hypertension. 2012; 60:1117–1123.13. Yi SW, Mok Y, Ohrr H, et al. Low systolic blood pressure and vascular mortality among more than 1 million Korean adults. Circulation. 2016; 133:2381–2390.
Article14. Jee SH, Kivimaki M, Kang HC, Park IS, Samet JM, Batty GD. Cardiovascular disease risk factors in relation to suicide mortality in Asia: prospective cohort study of over one million Korean men and women. Eur Heart J. 2011; 32:2773–2780.
Article15. National Health Insurance service (KR). National Health Insurance system of Korea, 2015 [Internet]. Seoul: National Health Insurance service;2015. cited 2017 Jan 26. Available from: https://www.nhis.or.kr/static/html/wbd/g/a/wbdga0704.html.16. Jee SH, Ohrr H, Sull JW, Samet JM. Cigarette smoking, alcohol drinking, hepatitis B, and risk for hepatocellular carcinoma in Korea. J Natl Cancer Inst. 2004; 96:1851–1856.
Article17. Liu X, Rodriguez CJ, Wang K. Prevalence and trends of isolated systolic hypertension among untreated adults in the United States. J Am Soc Hypertens. 2015; 9:197–205.
Article18. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.19. JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008; 31:2115–2127.20. Ogihara T, Saruta T, Rakugi H, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010; 56:196–202.21. Solini A, Grossman E. What should be the target blood pressure in elderly patients with diabetes? Diabetes Care. 2016; 39:Suppl 2. S234–S243.
Article22. Franklin SS, Lopez VA, Wong ND, et al. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation. 2009; 119:243–250.23. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article24. Kim RB, Kim BG, Kim YM, et al. Trends in the incidence of hospitalized acute myocardial infarction and stroke in Korea, 2006–2010. J Korean Med Sci. 2013; 28:16–24.
Article25. Yi SW, Odongua N, Nam CM, Sull JW, Ohrr H. Body mass index and stroke mortality by smoking and age at menopause among Korean postmenopausal women. Stroke. 2009; 40:3428–3435.
Article26. Sweeting MJ, Barrett JK, Thompson SG, Wood AM. The use of repeated blood pressure measures for cardiovascular risk prediction: a comparison of statistical models in the ARIC study. [Epub ahead of print]. Stat Med. 2016.
Article27. Hessel PA. Terminal digit preference in blood pressure measurements: effects on epidemiological associations. Int J Epidemiol. 1986; 15:122–125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blood pressure and heart failure
- The Significance of the J-Curve in Hypertension and Coronary Artery Diseases
- Blood Pressure Variability and Its Management in Hypertensive Patients
- A pilot study investigating the relationship between heart rate variability and blood pressure in young adults at risk for cardiovascular disease
- Effect of obesity and age on the blood pressure