J Rheum Dis.
2018 Jan;25(1):58-64. 10.4078/jrd.2018.25.1.58.
Prevalence, Risk Factors, and Expression of Human Leukocyte Antigen-DRB1 in Juvenile Idiopathic Arthritis-associated Uveitis
- Affiliations
-
- 1Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Korea. kwangnamkim@naver.com
- KMID: 2405021
- DOI: http://doi.org/10.4078/jrd.2018.25.1.58
Abstract
OBJECTIVE
This study investigated the prevalence and risk factors of juvenile idiopathic arthritis (JIA)-associated uveitis (JIA-U) in a pediatric tertiary center in Korea. In addition, this study examined whether a specific HLA-DRB1 allele could be a predictive risk factor of uveitis in JIA.
METHODS
The pediatric rheumatology and ophthalmology medical records for JIA between March 2006 and March 2016 were analyzed retrospectively. A total of 233 were enrolled in this study.
RESULTS
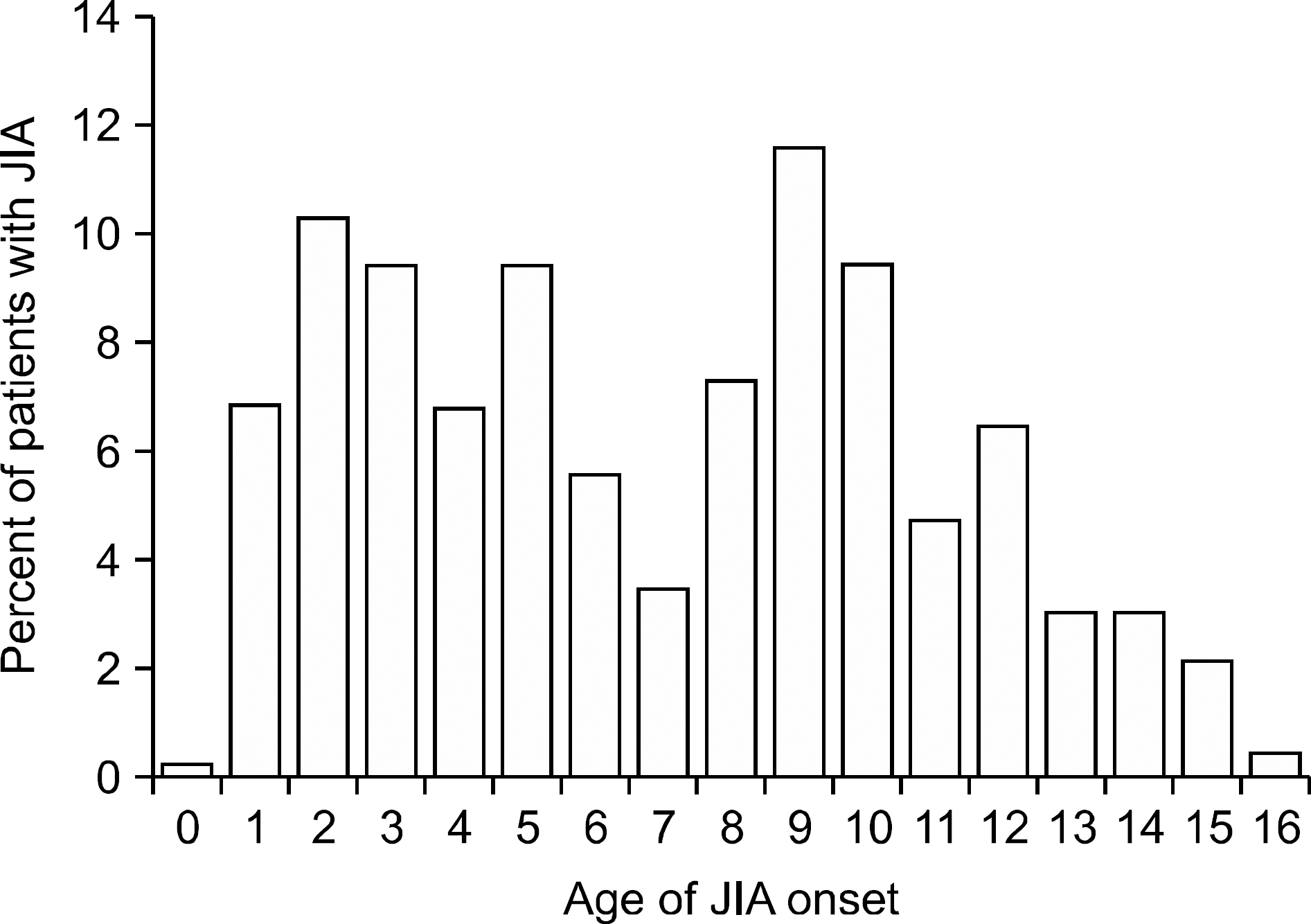
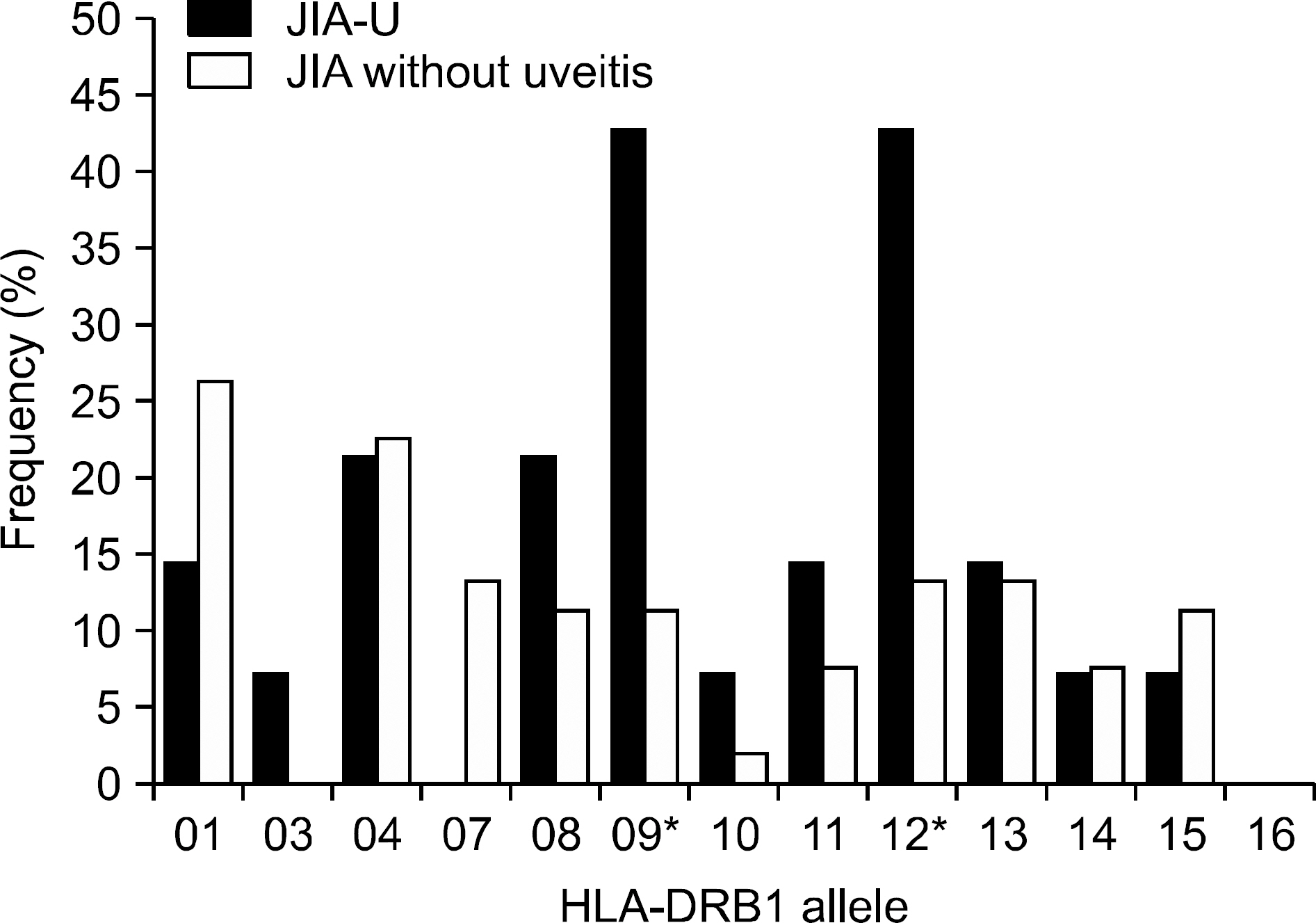
Of 233 patients, 31 developed uveitis (13.3%): 14 oligoarticular, three polyarticular, six systemic, seven enthesitis-related, and one undifferentiated-type JIA. In oligoarticular JIA, 26.4% developed uveitis. The percentage of females with JIA-U was 54.8%, and the median age of the onset of JIA was 7.02 years in JIA-U. Antinuclear antibody (ANA) positivity in oligoarticular JIA-U was 57.1%. Of the 31 JIA-U cases, 26 (83.9%) were clinically asymptomatic when diagnosed. The allele frequency of HLA-DRB1*09 of the total JIA-U was higher than that of JIA without uveitis. HLA-DRB1*09 and HLA-DRB1*12 were higher in oligoarticular JIA-U than in JIA without uveitis.
CONCLUSION
Korean JIA-U has different features from JIA-U in Western countries. The sex ratio and age of JIA onset showed no significant differences in Korean JIA-U. The ANA positivity was more common in JIA-U than in JIA without uveitis only in oligoarticular type JIA. These differences might be due to genetic factors, particularly HLA-DRB1. These results suggest HLA-DRB1*09 and HLA-DRB1*12 in oligoarticular JIA to be risk factors for JIA-U in Korea. This is the first study to analyze the association between HLA-DRB1 and JIA-U in Korea.
MeSH Terms
Figure
Reference
-
1. Edelsten C, Reddy MA, Stanford MR, Graham EM. Visual loss associated with pediatric uveitis in english primary and referral centers. Am J Ophthalmol. 2003; 135:676–80.
Article2. Angeles-Han ST, Yeh S, Vogler LB. Updates on the risk markers and outcomes of severe juvenile idiopathic arthritis-associated uveitis. Int J Clin Rheumtol. 2013; 8:109–21.
Article3. BenEzra D, Cohen E, Behar-Cohen F. Uveitis and juvenile idiopathic arthritis: A cohort study. Clin Ophthalmol. 2007; 1:513–8.4. Kanski JJ. Screening for uveitis in juvenile chronic arthritis. Br J Ophthalmol. 1989; 73:225–8.
Article5. Zierhut M, Michels H, Stübiger N, Besch D, Deuter C, Heiligenhaus A. Uveitis in children. Int Ophthalmol Clin. 2005; 45:135–56.
Article6. Saurenmann RK, Rose JB, Tyrrell P, Feldman BM, Laxer RM, Schneider R, et al. Epidemiology of juvenile idiopathic arthritis in a multiethnic cohort: ethnicity as a risk factor. Arthritis Rheum. 2007; 56:1974–84.
Article7. Clarke SL, Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Pediatr Rheumatol Online J. 2016; 14:27.
Article8. Chalom EC, Goldsmith DP, Koehler MA, Bittar B, Rose CD, Ostrov BE, et al. Prevalence and outcome of uveitis in a regional cohort of patients with juvenile rheumatoid arthritis. J Rheumatol. 1997; 24:2031–4.9. Saurenmann RK, Levin AV, Feldman BM, Rose JB, Laxer RM, Schneider R, et al. Prevalence, risk factors, and outcome of uveitis in juvenile idiopathic arthritis: a long-term followup study. Arthritis Rheum. 2007; 56:647–57.
Article10. Hoeve M, Kalinina Ayuso V, Schalij-Delfos NE, Los LI, Rothova A, de Boer JH. The clinical course of juvenile idiopathic arthritis-associated uveitis in childhood and puberty. Br J Ophthalmol. 2012; 96:852–6.
Article11. Moradi A, Amin RM, Thorne JE. The role of gender in juvenile idiopathic arthritis-associated uveitis. J Ophthalmol. 2014; 2014; 461078.
Article12. Kotaniemi K, Kautiainen H, Karma A, Aho K. Occurrence of uveitis in recently diagnosed juvenile chronic arthritis: a prospective study. Ophthalmology. 2001; 108:2071–5.
Article13. Paroli MP, Speranza S, Marino M, Pirraglia MP, Pivetti-Pezzi P. Prognosis of juvenile rheumatoid arthritis-associated uveitis. Eur J Ophthalmol. 2003; 13:616–21.
Article14. Woreta F, Thorne JE, Jabs DA, Kedhar SR, Dunn JP. Risk factors for ocular complications and poor visual acuity at presentation among patients with uveitis associated with juvenile idiopathic arthritis. Am J Ophthalmol. 2007; 143:647–55.
Article15. Edelsten C, Lee V, Bentley CR, Kanski JJ, Graham EM. An evaluation of baseline risk factors predicting severity in juvenile idiopathic arthritis associated uveitis and other chronic anterior uveitis in early childhood. Br J Ophthalmol. 2002; 86:51–6.
Article16. Saurenmann RK, Levin AV, Feldman BM, Laxer RM, Schneider R, Silverman ED. Risk factors for development of uveitis differ between girls and boys with juvenile idiopathic arthritis. Arthritis Rheum. 2010; 62:1824–8.
Article17. Melin-Aldana H, Giannini EH, Taylor J, Lovell DJ, Levinson JE, Passo MH, et al. Human leukocyte antigen-DRB1*1104 in the chronic iridocyclitis of pauciarticular juvenile rheumatoid arthritis. J Pediatr. 1992; 121:56–60.
Article18. Ploski R, Vinje O, Rønningen KS, Spurkland A, Sørskaar D, Vartdal F, et al. HLA class II alleles and heterogeneity of juvenile rheumatoid arthritis. DRB1*0101 may define a novel subset of the disease. Arthritis Rheum. 1993; 36:465–72.19. Zeggini E, Packham J, Donn R, Wordsworth P, Hall A, Thomson W. BSPAR Study Group. Association of HLA-DRB1*13 with susceptibility to uveitis in juvenile idiopathic arthritis in two independent data sets. Rheumatology (Oxford). 2006; 45:972–4.
Article20. Kalinina Ayuso V, Makhotkina N, van Tent-Hoeve M, de Groot-Mijnes JD, Wulffraat NM, Rothova A, et al. Pathogenesis of juvenile idiopathic arthritis associated uveitis: the known and unknown. Surv Ophthalmol. 2014; 59:517–31.
Article21. Berntson L, Andersson Gäre B, Fasth A, Herlin T, Kristinsson J, Lahdenne P, et al. Incidence of juvenile idiopathic arthritis in the Nordic countries. A population based study with special reference to the validity of the ILAR and EULAR criteria. J Rheumatol. 2003; 30:2275–82.22. Heiligenhaus A, Niewerth M, Ganser G, Heinz C, Minden K. German Uveitis in Childhood Study Group. Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nationwide study in Germany: suggested modification of the current screening guidelines. Rheumatology (Oxford). 2007; 46:1015–9.
Article23. Ravelli A, Felici E, Magni-Manzoni S, Pistorio A, Novarini C, Bozzola E, et al. Patients with antinuclear antibody-positive juvenile idiopathic arthritis constitute a homogeneous subgroup irrespective of the course of joint disease. Arthritis Rheum. 2005; 52:826–32.
Article24. Petty RE, Laxer RM, Lindsley CB, Wedderburn L. Textbook of pediatric rheumatology. 7th ed.Philadelphia: Elsevier;2016. p. 276.25. Kesen MR, Setlur V, Goldstein DA. Juvenile idiopathic arthritis-related uveitis. Int Ophthalmol Clin. 2008; 48:21–38.
Article26. American Academy of Pediatrics Section on Rheumatology and Section on Ophthalmology: Guidelines for ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 1993; 92:295–6.27. Coughlin L. Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Am Fam Physician. 2007; 75:1886.28. Kliegman RM, Stanton BMD, St Geme J, Schor NF, Behrman RE. Nelson textbook of pediatrics. 20th ed.Philadelphia: Elsevier;2016. p. 1164.29. Prahalad S, Glass DN. A comprehensive review of the genetics of juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2008; 6:11.
Article30. Clemens LE, Albert E, Ansell BM. Sibling pairs affected by chronic arthritis of childhood: evidence for a genetic predisposition. J Rheumatol. 1985; 12:108–13.31. Säilä H, Kotaniemi K, Savolainen A, Kautiainen H, Leirisalo-Repo M, Aho K. Uveitis in sibling pairs with juvenile idiopathic arthritis. Rheumatology (Oxford). 2001; 40:221–4.32. Moroldo MB, Tague BL, Shear ES, Glass DN, Giannini EH. Juvenile rheumatoid arthritis in affected sibpairs. Arthritis Rheum. 1997; 40:1962–6.
Article33. Zulian F, Martini G, Falcini F, Gerloni V, Zannin ME, Pinello L, et al. Early predictors of severe course of uveitis in oligoarticular juvenile idiopathic arthritis. J Rheumatol. 2002; 29:2446–53.34. Lee CJ, Sohn TY, Lee DH, Lee HR, Kim M, Kim KN. Human leukocyte antigen-DRB1 associations in Korean juvenile rheumatoid arthritis. J Rheum Dis. 2014; 21:182–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Human Leukocyte Antigen-DRB1 Associations in Korean Juvenile Rheumatoid Arthritis
- Association of Human Leukocyte Antigen-DRB1 with Juvenile Idiopathic Arthritis
- Clinical Manifestation of Juvenile Idiopathic Arthritis Associated Uveitis in Korea
- Human Leukocyte Antigen B27 and Juvenile Idiopathic Arthritis and Classification of Juvenile Spondyloarthropathies by the Assessment of SpondyloArthritis International Society Criteria
- A Case of Lung Involvement Associated with Juvenile Idiopathic Arthritis