Investig Clin Urol.
2018 Mar;59(2):83-90. 10.4111/icu.2018.59.2.83.
Can pelvic node dissection at radical prostatectomy influence the nodal recurrence at salvage lymphadenectomy for prostate cancer?
- Affiliations
-
- 1Urology Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, NY, USA. sivarama@mskcc.org
- 2Department of Biostatistics and Epidemiology, Memorial Sloan Kettering Cancer Center, NY, USA.
- KMID: 2404976
- DOI: http://doi.org/10.4111/icu.2018.59.2.83
Abstract
- PURPOSE
To verify the quality of pelvic lymph node dissection (PLND) performed at radical prostatectomy (RP) and its impact on nodal recurrence in patients undergoing salvage lymph node dissection (sLND).
MATERIALS AND METHODS
Retrospective review of 48 patients who underwent sLND for presumed nodal recurrence, to describe the PLND characteristics at RP and correlate the anatomical sites and number of suspicious nodes reported in radiological imaging and final pathology of sLND.
RESULTS
Overall, at RP, 8 (16.7%) did not undergo PLND, 32 (66.7%) and 8 (16.7%) received a "limited" (between external iliac vein and obturator nerve) and an "extended" (external iliac, hypogastric, and obturator) dissection, respectively. Median nodes removed during limited and extended dissection were 2 and 24, respectively. At sLND, the mean age was 61.3 years and median prostate specific antigen (PSA) was 1.07 ng/mL. Median nodes removed at sLND were 17 with a median of 2 positive nodes. Recurrent nodes were identified within the template of an extended PLND in 62.5%, 50.0% and 12.5% patients, respectively, following prior no, limited and extended dissection at RP. Recurrence outside the expected lymphatic drainage pathway was noted in 37.5% patients with prior extended dissection at RP. There was a correlation between imaging and pathology specimen in 83% for node location and 58.3% for number of anatomical sites involved.
CONCLUSIONS
In prostate cancer patients undergoing sLND, most had inadequate PLND at the original RP. Pattern of nodal recurrence may be influenced by the prior dissection and pre sLND imaging appears to underestimate the nodal recurrence.
Keyword
MeSH Terms
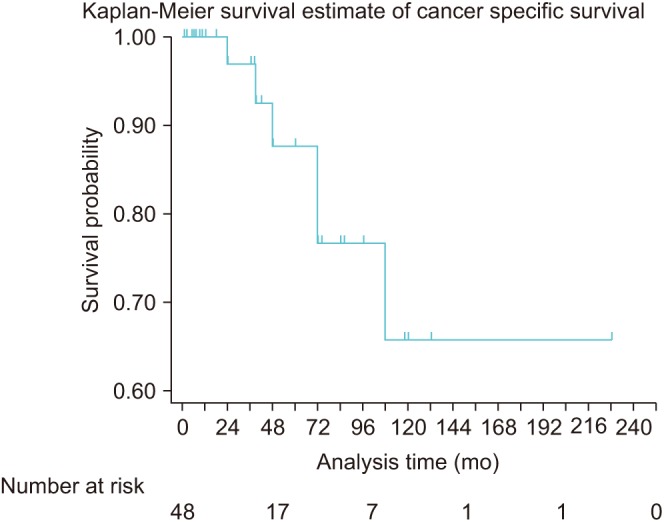
Figure
Reference
-
1. Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017; 71:618–629. PMID: 27568654.
Article2. American Urological Association. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline [Internet]. Linthicum: American Urological Association;2017. cited 2017 Apr 5. Available from: https://www.auanet.org/education/guidelines/prostate-cancer.cfm.3. Wang EH, Yu JB, Gross CP, Smaldone MC, Shah ND, Trinh QD, et al. Variation in pelvic lymph node dissection among patients undergoing radical prostatectomy by hospital characteristics and surgical approach: results from the National Cancer Database. J Urol. 2015; 193:820–825. PMID: 25242393.
Article4. Suardi N, Porter CR, Reuther AM, Walz J, Kodama K, Gibbons RP, et al. A nomogram predicting long-term biochemical recurrence after radical prostatectomy. Cancer. 2008; 112:1254–1263. PMID: 18286530.
Article5. Boorjian SA, Thompson RH, Tollefson MK, Rangel LJ, Bergstralh EJ, Blute ML, et al. Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur Urol. 2011; 59:893–899. PMID: 21388736.
Article6. Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, et al. Distribution of metastatic sites in patients with prostate cancer: a population-based analysis. Prostate. 2014; 74:210–216. PMID: 24132735.
Article7. Yossepowitch O, Bianco FJ Jr, Eggener SE, Eastham JA, Scher HI, Scardino PT. The natural history of noncastrate metastatic prostate cancer after radical prostatectomy. Eur Urol. 2007; 51:940–947. discussion 947-8. PMID: 17125912.
Article8. Suardi N, Gandaglia G, Gallina A, Di Trapani E, Scattoni V, Vizziello D, et al. Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single-institution series with a minimum follow-up of 5 years. Eur Urol. 2015; 67:299–309. PMID: 24571959.
Article9. Zattoni F, Nehra A, Murphy CR, Rangel L, Mynderse L, Lowe V, et al. Mid-term outcomes following salvage lymph node dissection for prostate cancer nodal recurrence status post-radical prostatectomy. Eur Urol Focus. 2016; 2:522–531. PMID: 28723518.
Article10. Paño B, Sebastià C, Buñesch L, Mestres J, Salvador R, Macías NG, et al. Pathways of lymphatic spread in male urogenital pelvic malignancies. Radiographics. 2011; 31:135–160. PMID: 21257939.
Article11. Mattei A, Fuechsel FG, Bhatta Dhar N, Warncke SH, Thalmann GN, Krause T, et al. The template of the primary lymphatic landing sites of the prostate should be revisited: results of a multimodality mapping study. Eur Urol. 2008; 53:118–125. PMID: 17709171.
Article12. Tokuda Y, Carlino LJ, Gopalan A, Tickoo SK, Kaag MG, Guillonneau B, et al. Prostate cancer topography and patterns of lymph node metastasis. Am J Surg Pathol. 2010; 34:1862–1867. PMID: 21107093.
Article13. Fossati N, Willemse PM, Van den Broeck T, van den Bergh RCN, Yuan CY, Briers E, et al. The benefits and harms of different extents of lymph node dissection during radical prostatectomy for prostate cancer: a systematic review. Eur Urol. 2017; 72:84–109. PMID: 28126351.
Article14. Allaf ME, Palapattu GS, Trock BJ, Carter HB, Walsh PC. Anatomical extent of lymph node dissection: impact on men with clinically localized prostate cancer. J Urol. 2004; 172:1840–1844. PMID: 15540734.
Article15. Bader P, Burkhard FC, Markwalder R, Studer UE. Is a limited lymph node dissection an adequate staging procedure for prostate cancer? J Urol. 2002; 168:514–518. discussion 518. PMID: 12131300.
Article16. Briganti A, Blute ML, Eastham JH, Graefen M, Heidenreich A, Karnes JR, et al. Pelvic lymph node dissection in prostate cancer. Eur Urol. 2009; 55:1251–1265. PMID: 19297079.
Article17. Briganti A, Chun FK, Salonia A, Gallina A, Farina E, Da Pozzo LF, et al. Validation of a nomogram predicting the probability of lymph node invasion based on the extent of pelvic lymphadenectomy in patients with clinically localized prostate cancer. BJU Int. 2006; 98:788–793. PMID: 16796698.
Article18. Briganti A, Chun FK, Salonia A, Gallina A, Zanni G, Scattoni V, et al. Critical assessment of ideal nodal yield at pelvic lymphadenectomy to accurately diagnose prostate cancer nodal metastasis in patients undergoing radical retropubic prostatectomy. Urology. 2007; 69:147–151. PMID: 17270638.
Article19. Heidenreich A, Varga Z, Von Knobloch R. Extended pelvic lymphadenectomy in patients undergoing radical prostatectomy: high incidence of lymph node metastasis. J Urol. 2002; 167:1681–1686. PMID: 11912387.
Article20. Masterson TA, Bianco FJ Jr, Vickers AJ, DiBlasio CJ, Fearn PA, Rabbani F, et al. The association between total and positive lymph node counts, and disease progression in clinically localized prostate cancer. J Urol. 2006; 175:1320–1324. discussion 1324-5. PMID: 16515989.
Article21. Touijer K, Rabbani F, Otero JR, Secin FP, Eastham JA, Scardino PT, et al. Standard versus limited pelvic lymph node dissection for prostate cancer in patients with a predicted probability of nodal metastasis greater than 1%. J Urol. 2007; 178:120–124. PMID: 17499306.
Article22. Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, et al. Sensitivity, specificity, and predictors of positive (68)Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016; 70:926–937. PMID: 27363387.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Patients With High Risk Prostate Cancer
- Salvage Radiotherapy for Patients with PSA Relapse Following Radical Prostatectomy: Issues and Challenges
- Radical Prostatectomy
- Rationale of Surgery in Locally Advanced and Oligometastatic Prostate Cancer
- Radical Cystectomy with Pelvic Lymphadenectomy in Bladder Tumor: Review of 14 Cases