Korean J Radiol.
2018 Apr;19(2):272-283. 10.3348/kjr.2018.19.2.272.
Multimodality Imaging in Patients with Secondary Hypertension: With a Focus on Appropriate Imaging Approaches Depending on the Etiologies
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam 13620, Korea. drejchun@hanmail.net
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam 13620, Korea.
- KMID: 2404924
- DOI: http://doi.org/10.3348/kjr.2018.19.2.272
Abstract
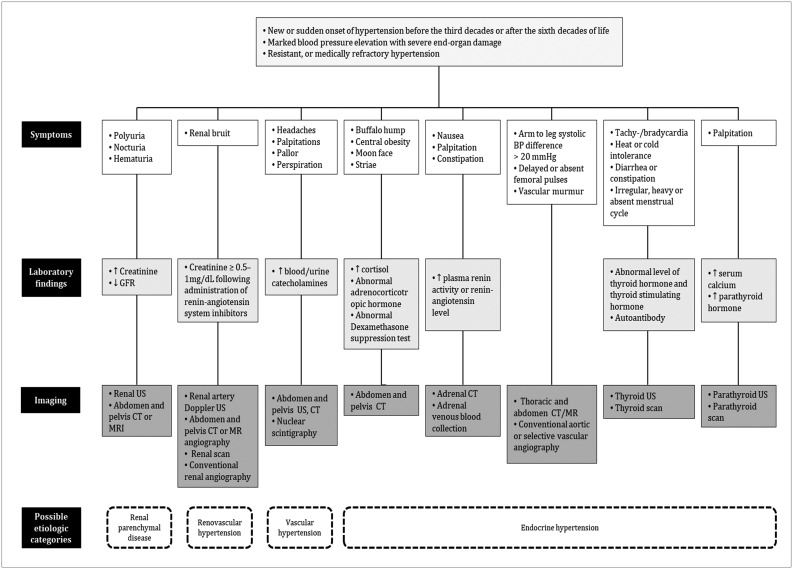
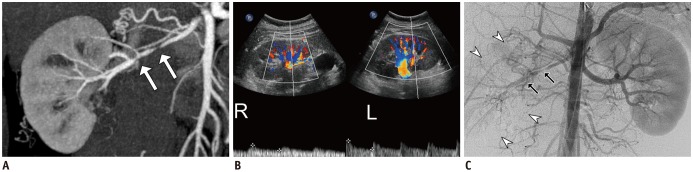
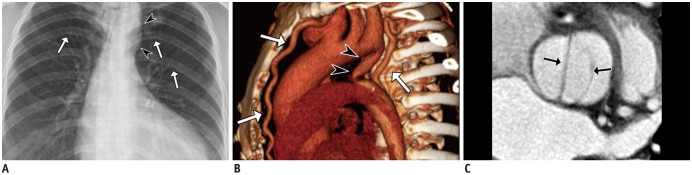
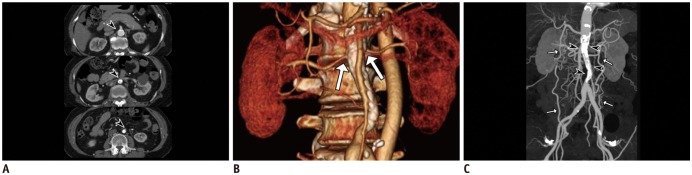
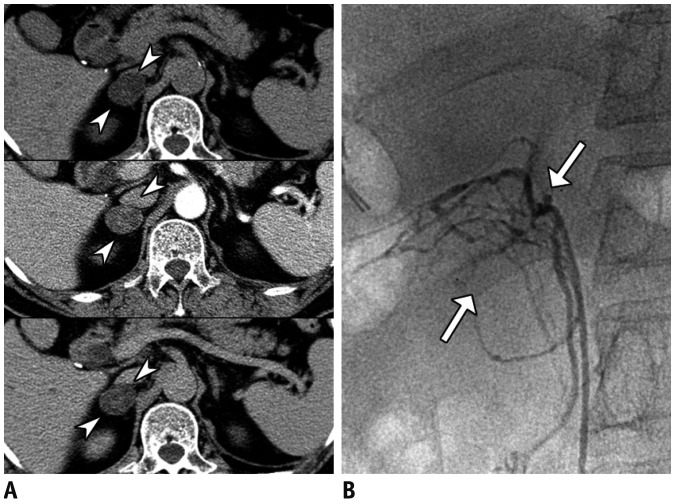
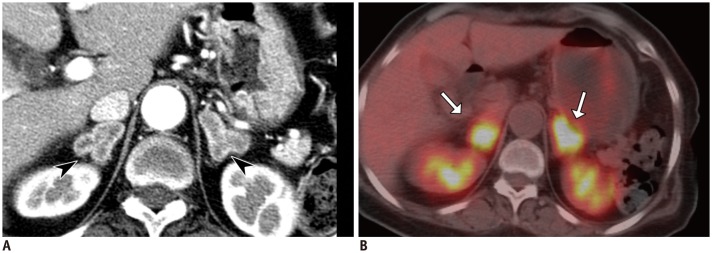
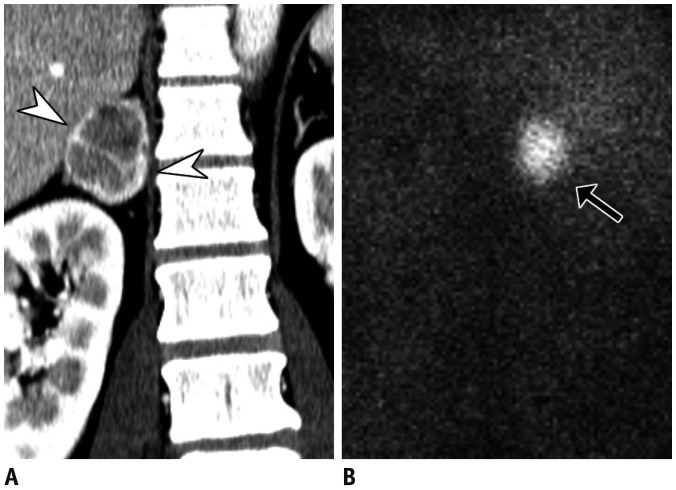
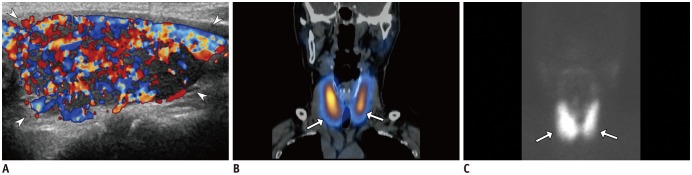
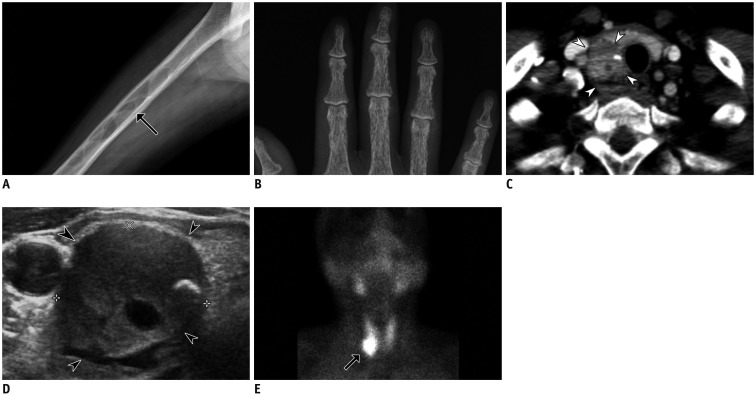
- Although the causes of hypertension are usually unknown, about 10% of the cases occur secondary to specific etiologies, which are often treatable. Common categories of secondary hypertension include renal parenchymal disease, renovascular stenosis, vascular and endocrinologic disorders. For diseases involving the renal parenchyma and adrenal glands, ultrasonography (US), computed tomography (CT) or magnetic resonance (MR) imaging is recommended. For renovascular stenosis and vascular disorders, Doppler US, conventional or noninvasive (CT or MR) angiography is an appropriate modality. Nuclear imaging can be useful in the differential diagnosis of endocrine causes. Radiologists should understand the role of each imaging modality and its typical findings in various causes of secondary hypertension. This article focuses on appropriate imaging approaches in accordance with the categorized etiologies leading to hypertension.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Guideline for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 1: Standardized Protocol
Yeseul Jo, JeongJae Kim, Chul Hwan Park, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee, Dong Jin Im, Su Jin Hong, Eun Young Kim, Eun-Ah Park, Pan Ki Kim, Hwan Seok Yong
Korean J Radiol. 2019;20(9):1313-1333. doi: 10.3348/kjr.2019.0398.
Reference
-
1. Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD, Robertson JW. Secondary hypertension in a blood pressure clinic. Arch Intern Med. 1987; 147:1289–1293. PMID: 3606286.
Article2. Anderson GH Jr, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens. 1994; 12:609–615. PMID: 7930562.
Article3. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014; 35:1245–1254. PMID: 24366917.
Article4. Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014; 37:253–390. PMID: 24705419.
Article5. Akpunonu BE, Mulrow PJ, Hoffman EA. Secondary hypertension: evaluation and treatment. Dis Mon. 1996; 42:609–722. PMID: 8948319.
Article6. Chiong JR, Aronow WS, Khan IA, Nair CK, Vijayaraghavan K, Dart RA, et al. Secondary hypertension: current diagnosis and treatment. Int J Cardiol. 2008; 124:6–21. PMID: 17462751.
Article7. Ferguson RK. Cost and yield of the hypertensive evaluation. Experience of a community-based referral clinic. Ann Intern Med. 1975; 82:761–776. PMID: 1138586.8. Danielson M, Dammström B. The prevalence of secondary and curable hypertension. Acta Med Scand. 1981; 209:451–455. PMID: 7257863.
Article9. Kimura G. Clinical pathology and treatment of renin-angiotensin system 2. Chronic kidney disease and the renin-angiotensin system. Intern Med. 2007; 46:1295–1298. PMID: 17704608.
Article10. Usami T, Nakao N, Fukuda M, Takeuchi O, Kamiya Y, Yoshida A, et al. Maps of end-stage renal disease and amounts of angiotensin-converting enzyme inhibitors prescribed in Japan. Kidney Int. 2003; 64:1445–1449. PMID: 12969164.
Article11. Ihm CG. Hypertension in chronic glomerulonephritis. Electrolyte Blood Press. 2015; 13:41–45. PMID: 26848302.
Article12. Joles JA, Koomans HA. Causes and consequences of increased sympathetic activity in renal disease. Hypertension. 2004; 43:699–706. PMID: 14981063.
Article13. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA task force on practice guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006; 113:e463–e654. PMID: 16549646.
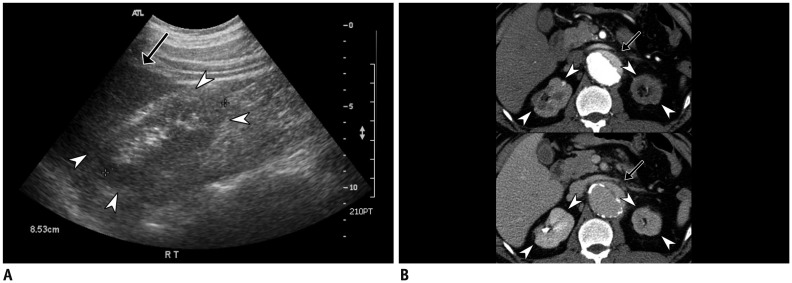
Article14. Nahm AM, Henriquez DE, Ritz E. Renal cystic disease (ADPKD and ARPKD). Nephrol Dial Transplant. 2002; 17:311–314. PMID: 11812890.
Article15. Higashihara E, Aso Y, Shimazaki J, Ito H, Koiso K, Sakai O. Clinical aspects of polycystic kidney disease. J Urol. 1992; 147:329–332. PMID: 1732586.
Article16. Kelleher CL, McFann KK, Johnson AM, Schrier RW. Characteristics of hypertension in young adults with autosomal dominant polycystic kidney disease compared with the general U.S population. Am J Hypertens. 2004; 17(11 Pt 1):1029–1034. PMID: 15533729.
Article17. Wood CG 3rd, Stromberg LJ 3rd, Harmath CB, Horowitz JM, Feng C, Hammond NA, et al. CT and MR imaging for evaluation of cystic renal lesions and diseases. Radiographics. 2015; 35:125–141. PMID: 25590393.
Article18. Pirson Y, Chauveau D, Torres V. Management of cerebral aneurysms in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2002; 13:269–276. PMID: 11752048.
Article19. Ring T, Spiegelhalter D. Risk of intracranial aneurysm bleeding in autosomal-dominant polycystic kidney disease. Kidney Int. 2007; 72:1400–1402. PMID: 17882153.
Article20. Ong AC. Screening for intracranial aneurysms in ADPKD. BMJ. 2009; 339:b3763. PMID: 19770180.
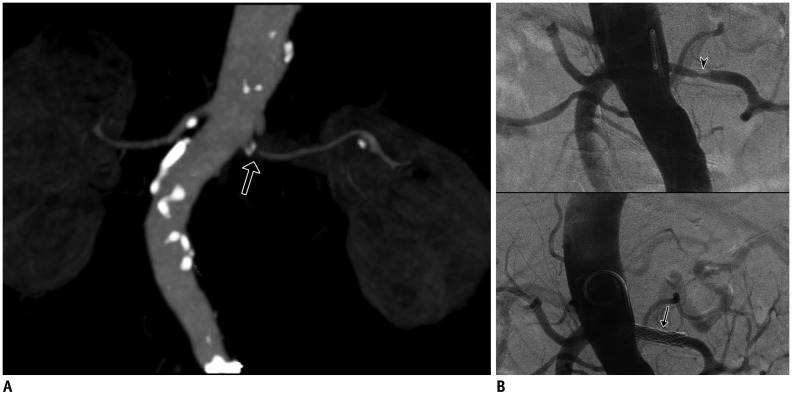
Article21. Mann SJ, Pickering TG. Detection of renovascular hypertension. State of the art: 1992. Ann Intern Med. 1992; 117:845–853. PMID: 1416561.22. Soulez G, Oliva VL, Turpin S, Lambert R, Nicolet V, Therasse E. Imaging of renovascular hypertension: respective values of renal scintigraphy, renal Doppler US, and MR angiography. Radiographics. 2000; 20:1355–1368. discussion 1368-1372. PMID: 10992024.
Article23. Slovut DP, Olin JW. Fibromuscular dysplasia. N Engl J Med. 2004; 350:1862–1871. PMID: 15115832.
Article24. Olin JW, Sealove BA. Diagnosis, management, and future developments of fibromuscular dysplasia. J Vasc Surg. 2011; 53:826–836.e1. PMID: 21236620.
Article25. Mohammed NM, Mahfouz A, Achkar K, Rafie IM, Hajar R. Contrast-induced nephropathy. Heart Views. 2013; 14:106–116. PMID: 24696755.
Article26. Hellman RN. Gadolinium-induced nephrogenic systemic fibrosis. Semin Nephrol. 2011; 31:310–316. PMID: 21784280.
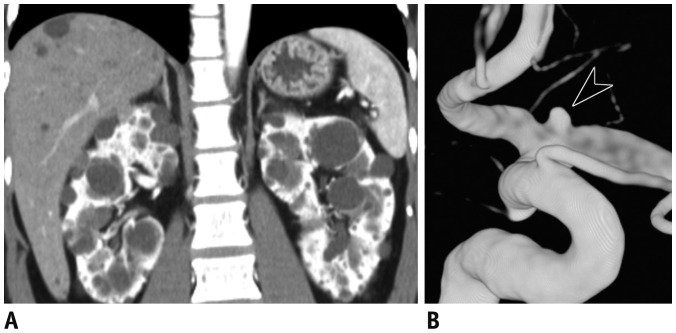
Article27. Kim HD, Kim MN, Kim SA, Choi SI, Choi JY, Seo JH, et al. Resistant hypertension caused by stenosis of the aorta in elderly women: three case reports. Clin Hypertens. 2014; 20:5. PMID: 26893910.
Article28. Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. Am Fam Physician. 2010; 82:1471–1478. PMID: 21166367.29. Wu MH, Chen HC, Kao FY, Huang SK. Risk of systemic hypertension and cerebrovascular accident in patients with aortic coarctation aged <60 years (from a national database study). Am J Cardiol. 2015; 116:779–784. PMID: 26100586.30. Abbruzzese PA, Aidala E. Aortic coarctation: an overview. J Cardiovasc Med (Hagerstown). 2007; 8:123–128. PMID: 17299295.
Article31. Nance JW, Ringel RE, Fishman EK. Coarctation of the aorta in adolescents and adults: a review of clinical features and CT imaging. J Cardiovasc Comput Tomogr. 2016; 10:1–12. PMID: 26639936.
Article32. Sebastià C, Quiroga S, Boyé R, Perez-Lafuente M, Castellà E, Alvarez-Castells A. Aortic stenosis: spectrum of diseases depicted at multisection CT. Radiographics. 2003; 23(Spec No):S79–S91. PMID: 14557504.
Article33. Ho VB, Bakalov VK, Cooley M, Van PL, Hood MN, Burklow TR, et al. Major vascular anomalies in Turner syndrome: prevalence and magnetic resonance angiographic features. Circulation. 2004; 110:1694–1700. PMID: 15353492.
Article34. Campbell M. Natural history of coarctation of the aorta. Br Heart J. 1970; 32:633–640. PMID: 5470045.
Article35. Connolly JE, Wilson SE, Lawrence PL, Fujitani RM. Middle aortic syndrome: distal thoracic and abdominal coarctation, a disorder with multiple etiologies. J Am Coll Surg. 2002; 194:774–781. PMID: 12081068.36. Delis KT, Gloviczki P. Middle aortic syndrome: from presentation to contemporary open surgical and endovascular treatment. Perspect Vasc Surg Endovasc Ther. 2005; 17:187–203. PMID: 16273154.
Article37. Daghero F, Bueno N, Peirone A, Ochoa J, Torres GF, Ganame J. Coarctation of the abdominal aorta: an uncommon cause of arterial hypertension and stroke. Circ Cardiovasc Imaging. 2008; 1:e4. e6. PMID: 19808505.39. Sica DA. Endocrine causes of secondary hypertension. J Clin Hypertens (Greenwich). 2008; 10:534–540. PMID: 18607139.
Article40. Gallay BJ, Ahmad S, Xu L, Toivola B, Davidson RC. Screening for primary aldosteronism without discontinuing hypertensive medications: plasma aldosterone-renin ratio. Am J Kidney Dis. 2001; 37:699–705. PMID: 11273868.
Article41. Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004; 22:2217–2226. PMID: 15480108.42. Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008; 93:3266–3281. PMID: 18552288.
Article43. Boland GW, Lee MJ, Gazelle GS, Halpern EF, McNicholas MM, Mueller PR. Characterization of adrenal masses using unenhanced CT: an analysis of the CT literature. AJR Am J Roentgenol. 1998; 171:201–204. PMID: 9648789.
Article44. Sohaib SA, Peppercorn PD, Allan C, Monson JP, Grossman AB, Besser GM, et al. Primary hyperaldosteronism (Conn syndrome): MR imaging findings. Radiology. 2000; 214:527–531. PMID: 10671606.
Article45. Blake MA, Kalra MK, Sweeney AT, Lucey BC, Maher MM, Sahani DV, et al. Distinguishing benign from malignant adrenal masses: multi-detector row CT protocol with 10-minute delay. Radiology. 2006; 238:578–585. PMID: 16371582.
Article46. Korobkin M, Brodeur FJ, Francis IR, Quint LE, Dunnick NR, Londy F. CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol. 1998; 170:747–752. PMID: 9490968.
Article47. Peña CS, Boland GW, Hahn PF, Lee MJ, Mueller PR. Characterization of indeterminate (lipid-poor) adrenal masses: use of washout characteristics at contrast-enhanced CT. Radiology. 2000; 217:798–802. PMID: 11110946.
Article48. Seo JM, Park BK, Park SY, Kim CK. Characterization of lipid-poor adrenal adenoma: chemical-shift MRI and washout CT. AJR Am J Roentgenol. 2014; 202:1043–1450. PMID: 24758658.
Article49. Rossi GP, Sacchetto A, Chiesura-Corona M, De Toni R, Gallina M, Feltrin GP, et al. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab. 2001; 86:1083–1090. PMID: 11238490.
Article50. Raff H, Sharma ST, Nieman LK. Physiological basis for the etiology, diagnosis, and treatment of adrenal disorders: Cushing's syndrome, adrenal insufficiency, and congenital adrenal hyperplasia. Compr Physiol. 2014; 4:739–769. PMID: 24715566.
Article51. Sohaib SA, Hanson JA, Newell-Price JD, Trainer PJ, Monson JP, Grossman AB, et al. CT appearance of the adrenal glands in adrenocorticotrophic hormone-dependent Cushing's syndrome. AJR Am J Roentgenol. 1999; 172:997–1002. PMID: 10587135.
Article52. Rockall AG, Babar SA, Sohaib SA, Isidori AM, Diaz-Cano S, Monson JP, et al. CT and MR imaging of the adrenal glands in ACTH-independent cushing syndrome. Radiographics. 2004; 24:435–452. PMID: 15026592.
Article53. Sukor N. Endocrine hypertension--current understanding and comprehensive management review. Eur J Intern Med. 2011; 22:433–440. PMID: 21925049.54. Tischler AS. Pheochromocytoma and extra-adrenal paraganglioma: updates. Arch Pathol Lab Med. 2008; 132:1272–1284. PMID: 18684026.
Article55. Leung K, Stamm M, Raja A, Low G. Pheochromocytoma: the range of appearances on ultrasound, CT, MRI, and functional imaging. AJR Am J Roentgenol. 2013; 200:370–378. PMID: 23345359.
Article56. Prisant LM, Gujral JS, Mulloy AL. Hyperthyroidism: a secondary cause of isolated systolic hypertension. J Clin Hypertens (Greenwich). 2006; 8:596–599. PMID: 16896276.
Article57. Marcisz C, Jonderko G, Kucharz EJ. Influence of short-time application of a low sodium diet on blood pressure in patients with hyperthyroidism or hypothyroidism during therapy. Am J Hypertens. 2001; 14:995–1002. PMID: 11710792.
Article58. Nachiappan AC, Metwalli ZA, Hailey BS, Patel RA, Ostrowski ML, Wynne DM. The thyroid: review of imaging features and biopsy techniques with radiologic-pathologic correlation. Radiographics. 2014; 34:276–293. PMID: 24617678.
Article59. Silverberg SJ, Bilezikian JP. The diagnosis and management of asymptomatic primary hyperparathyroidism. Nat Clin Pract Endocrinol Metab. 2006; 2:494–503. PMID: 16957763.
Article60. Feldstein CA, Akopian M, Pietrobelli D, Olivieri A, Garrido D. Long-term effects of parathyroidectomy on hypertension prevalence and circadian blood pressure profile in primary hyperparathyroidism. Clin Exp Hypertens. 2010; 32:154–158. PMID: 20504122.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Right Ventricular Function in Pulmonary Hypertension with Multimodality Imaging
- Multi Modality Imaging Features of Cardiac Myxoma
- Multimodality Imaging in Coronary Artery Disease: Focus on Computed Tomography
- FDG-PET in Multimodality Assessment of Cardiac Myxoma
- Aortic Coarctation Following Aortic Valve Replacement: Problem Solving with Multimodality Cardiac Imaging